Increasing Private Payment Rates to Health Centers in Hawaii
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Representative Faye Hanohano, Chair Representative Henry Aquino, Vice Chair and Board of Directors Members Ofthe Committee on Public Safety Pamela Lichty, M.P.H
121 Mystic Avenue, Medford. Massachusetts 02155 - Tele: 781.393.6985 Fax; 781.393.2964 [email protected] www.leap.cc BOARD OF DIRECTORS Representative Faye Hanohano, Chair Jack A. Cole Representative Henry Aquino, Vice Chair and Executive Director - Medford. MA Members ofthe Committee on Public Safety Peter Christ Vice Director - Syracuse, NY Representative Ryan Yamane, Chair James Gieraeh Representative Scott Nishimoto, Vice Chairand Secretary - Chicago, IL Members ofthe Committee on Health Tony Ryan Treasurer - Tucson, AZ SB 2213, SDI Relating to Counties James Anthony Hearing: Thursday, March 11, 10:45 a.m, Room 309 Oakland, CA Position: Support Stanford "Neill" Franklin Baltimore, MD Submitted by: Jay Fleming Maria lucia Karam Rio de Janeiro, Brazil Law Enforcement Against Prohibition www.CopsSayLegalizeDrugs.com Terry Nelson Dallas, TX Thank you for allowing me to submit this statement in favor ofSB 2213 SO 2. I fought against the Jerry Paradis British Columbia, Canada drug trade for 15 years, including time spent as an undercover narcotics officer. I am a speaker for Law Enforcement Against Prohibition, an organization of 16,000 current and former criminal ADVISORY BOARD justice professionals and civilian members. We are cops, sheriffs, prosecutors, judges, prison Senator larry Campbell guards and others from nearly every level oflaw enforcement. Former Mayor of Vancouver, Canada and Royal Canadian Mounted Police As a former officer, I know that the voice ofpolice is crucial in the dialogue about drug policy. But libby Davies in the case ofmedical marijuana, physicians, caregivers, and patients are the ones who should be Member of Canadian Parliament making decisions about medical care. -

The Twenty-Sixth Legislature Regular Session of 20 II HOUSE OF
The Twenty-Sixth Legislature Regular Session of20II HOUSE OF REPRESENTATIVES Committee on Health Rep. Ryan 1. Yamane, Chair Rep. Dee Morikawa, Vice Chair State Capitol, Conference Room 329 Tuesday, March 22, 2011; 9:00 a.m. STATEMENT OF THE ILWU LOCAL 142 ON S.B.1086, SD1 RELATING TO CONSUMER INFORMATION The ILWU Local 142 strongly supports S.B. 1086, SD1, which requires sliced, sandwich-style bread products that have been baked and then frozen to be labeled "previously frozen" and prohibits bread that has been frozen to be labeled or advertised as "fresh." The II.WU represents almost 300 members who work at Love's Bakery in production, driver-sales, office clerical work, and the thrift stores. Many ofthem have worked at the bakery for many years under various owners. Today, the company is owned and managed by a local team that invested its own money to keep this manufacturing company viable. For 160 years, Love's Bakery has put fresh sandwich bread on our table. It was only in the last decade that previously frozen bread took over a greater share ofthe market. However, the consumer was never informed that the previously frozen bread was baked on the mainland, then frozen and later thawed before sale. The consumer did not have the information needed to make an informed choice. This lack ofinformation has given previously frozen bread an unfair advantage over fresh bread. S.B. 1086, SDI will require that packaging ofpreviously frozen and thawed sliced, sandwich-style bread be imprinted with the words "previously frozen." With this information, consumers can ask their own questions, then make an informed decision about which bread to purchase. -

TO: the Honorable John M. Mizuno, Chair House Committee on Health and Human Services
DAVID Y. IGE PANKAJ BHANOT GOVERNOR DIRECTOR CATHY BETTS DEPUTY DIRECTOR STATE OF HAWAII DEPARTMENT OF HUMAN SERVICES P. O. Box 339 Honolulu, Hawaii 96808 February 13, 2018 TO: The Honorable John M. Mizuno, Chair House Committee on Health and Human Services The Honorable Aaron Ling Johanson, Chair House Committee on Labor and Public Employment FROM: Pankaj Bhanot, Director SUBJECT: HB 2204 - RELATING TO HUMAN SERVICES Hearing: Tuesday, February 13, 2018, 8:35 a.m. Conference Room 329, State Capitol DEPARTMENT’S POSITION: The Department of Human Services (DHS) supports the intent of this bill and provides comments. PURPOSE: The purpose of this bill is to establish a task force that shall develop a restructured welfare payment system; re-establishes the exit and retention bonus program to encourage welfare recipients to transition back into the workforce; and appropriates funds. The Financial Assistance Advisory Council (FAAC) was established in accordance with section 346-14.5, Hawaii Revised Statutes. The purpose of the FAAC is to render advice and information relating to the financial assistance programs. The proposed task force will be duplicative of what is already established in the Hawaii Revised Statutes. The department suggests that the committees consider utilizing the FAAC for this purpose, rather than establishing a task force. Regarding the exit and retention bonus program, in October 2006, DHS implemented the “Reward Works” initiative which included the exit and retention bonus payments. The bonuses were based on a family’s average number of employment hours per week. The Reward Works initiative ended February 1, 2012 because DHS did not have funds to fiscally sustain the exit and retention bonuses. -

2014 Political Corporate Contributions 2-19-2015.Xlsx
2014 POLITICAL CORPORATE CONTRIBUTIONS Last Name First Name Committee Name State Office District Party 2014 Total ($) Alabama 2014 PAC AL Republican 10,000 Free Enterprise PAC AL 10,000 Mainstream PAC AL 10,000 Collins Charles Charlie Collins Campaign Committee AR Representative AR084 Republican 750 Collins‐Smith Linda Linda Collins‐Smith Campaign Committee AR Senator AR019 Democratic 1,050 Davis Andy Andy Davis Campaign Committee AR Representative AR031 Republican 750 Dotson Jim Jim Dotson Campaign Committee AR Representative AR093 Republican 750 Griffin Tim Tim Griffin Campaign Committee AR Lt. Governor AR Republican 2,000 Rapert Jason Jason Rapert Campaign Committee AR Senator AR035 Republican 1,000 Rutledge Leslie Leslie Rutledge Campaign Committee AR Attorney General AR Republican 2,000 Sorvillo Jim Jim Sorvillo Campaign Committee AR Representative AR032 Republican 750 Williams Eddie Joe GoEddieJoePAC AR Senator AR029 Republican 5,000 Growing Arkansas AR Republican 5,000 Senate Victory PAC AZ Republican 2,500 Building Arizona's Future AZ Democratic 5,000 House Victory PAC AZ Republican 2,500 Allen Travis Re‐Elect Travis Allen for Assembly 2014 CA Representative CA072 Republican 1,500 Anderson Joel Tax Fighters for Joel Anderson, Senate 2014 CA Senator CA038 Republican 2,500 Berryhill Tom Tom Berryhill for Senate 2014 CA Senator CA008 Republican 2,500 Bigelow Frank Friends of Frank Bigelow for Assembly 2014 CA Representative CA005 Republican 2,500 Bonin Mike Mike Bonin for City Council 2013 Officeholder Account CA LA City Council -

HCUL PAC Fund Financial Report for the Period Ending June 30, 2019
HCUL PAC Fund Financial Report For the Period Ending June 30, 2019 State PAC CULAC Total Beginning Balance 07/01/2018 58,614.22 1,210.53 59,824.75 ADD: PAC Contributions 15,649.90 9,667.00 25,316.90 Interest & Dividends 408.03 2.88 410.91 74,672.15 10,880.41 85,552.56 LESS: Contributions to state and county candidates (8,693.96) - (8,693.96) CULAC Contribution Transfer - (10,068.00) (10,068.00) Federal & State Income Taxes - - - Fees (Svc Chrgs, Chk Rrders, Rtn Chk, Stop Pmt, Tokens, Etc.) - (398.27) (398.27) Wire charges, fees & other - - - (8,693.96) (10,466.27) (19,160.23) Ending Balance as of 6/30/2019 65,978.19 414.14 66,392.33 Balance per GL 65,978.19 414.14 66,392.33 Variance - (0) - Contributions to State and County Candidates for Fiscal Year Ending June 2019 Date Contributed To Amount Total 7/25/2018 Friends of Mike Molina $ 100.00 Total for July 2018 $ 100.00 8/16/2018 David Ige for Governor 500.00 Total for August 2018 500.00 9/18/2018 Friends of Alan Arakawa 200.00 9/18/2018 Friends of Stacy Helm Crivello 200.00 Total for September 2018 400.00 10/2/2018 Friends of Mike Victorino 750.00 10/18/2018 Friends of Justin Woodson 150.00 10/18/2018 Friends of Gil Keith-Agaran 150.00 10/18/2018 Friends of Riki Hokama 200.00 Total for October 2018 1,250.00 11/30/2018 Plexcity 43.96 Total for November 2018 43.96 1/11/2019 Friends of Glenn Wakai 150.00 1/17/2019 Friends of Scott Nishimoto 150.00 1/17/2019 Friends of Sylvia Luke 150.00 1/17/2019 Friends of Gil Keith-Agaran 300.00 1/17/2019 Friends of Della Au Belatti 150.00 1/17/2019 Friends -

Department of Public Safety Testimony on Senate Bill
CLAYTON A. FRANK LINDA LINGLE DIRECTOR GOVERNOR DAVID F. FESTERLING Deputy Director of Administration TOMMYJOHNSON Deputy Director Corrections STATE OF HAWAII JAMES L. PROPOTNICK DEPARTMENT OF PUBLIC SAFETY Deputy Director 1h 919 Ala Moana Blvd. 4 Floor Law Enforcement Honolulu, Hawaii 96813 No. _ TESTIMONY ON SENATE BILL 2213 SD2 A BILL FOR AN ACT RELATING TO COUNTIES Clayton A. Frank, Director Department of Public Safety Committee on Public Safety Representative Faye P. Hanohano, Chair Representative Henry J.C. Aquino, Vice Chair Committee on Health Representative Ryan I. Yamane, Chair Representative Scott Y. Nishimoto, Vice Chair Thursday, March 11, 2010, 10:45 AM State Capitol, Room 309 Representative Hanohano, Yamane and Members of the Committees: The Department of Public Safety does not support Senate Bill 2213 SD2 that proposes to amend Section 46-1.5 relating to general powers and limitations of the counties by allowing Hawaii's four counties to independently develop and establish dispensaries for the distrib~tion of marijuana for medical use to qualifying patients and primary caregivers registered under section 329-123 HRS. This could result in four separate sets of rules and regulations set by the counties that would have to be regulated and enforced, without any clarification as to which government entity is to regulate this practice. Senate Bill 2213 SD2 requires the Department of Public Safety to annually register these compassion centers, although it is not clear if the Department or the counties will be tasked with the collection and dispersment of the $5000.00 registration fee, nor does the SB2213 SD2 March 11,2010 Page 2 bill allocate any manpower or funds to implement this new program. -

Pacific Basin TRC Feb. 2020 Legislative Update
Pacific Basin TRC Feb. 2020 Legislative Update Last Updated: February 28, 2020 The Pacific Basin Telehealth Resource Center provides telehealth technical assistance to the state of Hawaii. A few notes about this report: 1. Bills are organized into specific telehealth "topic area". 2. The Fiscal Note (FN) Outlook: The left hand column indicates the bill's Pre-Floor Score, and the right hand column indicates the bill's actual Floor Score of the last chamber it was in (either Senate or House). 3. Regulations are listed at the end in order of their publication date. 4. If you would like to learn more about any piece of legislation or regulation, the bill numbers and regulation titles are clickable and link out to additional information. Bills by Issue Bills by Status Broadband 1 1 Cross-State Licensi… 2 2 Demonstrations, … 1 Medicaid Reimbur… 0 Medicare Reimbur… Network Adequacy 0 Online Prescribing Other 2 2 Private Payer Rei… 0 Provider-Patient R… 7 - Introduced Regulatory, Licensi… 3 3 Substance Use Dis… 0 2 - Passed First Chamber 0 2 4 High Medium Low None All Bills Broadband (1) State Bill Number Last Action Status FN Outlook HI HB 2264 Passed Second Reading As Amended In Hd 1 In House 90.2% 66.4% And Referred To The Committee S On Cpc With None Voting Aye With Reservations None Voting No 0 And Representative S Mcdermott Yamashita Excused 2 2020 02 07 Title Bill Summary: Establishes the Executive Office on Broadband Relating To Broadband Development. Development and the Hawaii Broadband Advisory Council. Directs the council to promote statewide access to broadband services and Description encourage the use of broadband for telehealth, among other goals. -

ILWU Endorses Ige, Tsutsui, Schatz, Takai and Gabbard
OF September/October 2014 VOICE THE ILWU page 1 HAWAII Volume 54 • No. 5 The VOICE of the ILWU—Published by Local 142, International Longshore & Warehouse Union September/October 2014 ILWU endorses Ige, Tsutsui, ADDRESS L A BE Schatz, Takai and Gabbard L The ILWU Local 142 Political Action Committee is endorsing David Ige, the democratic nominee for Governor, and Lieutenant Governor Shan Tsutsui in the November 4 General Election. Together, this team has over 38 years of legislative experience. Both candidates have and will continue to champion issues important to working families such as better education, lowering the cost of healthcare, maintaining workers’ compensation, and improving long-term care. We can depend on them to work hard to set a course that meets the needs of Hawaii’s future generations. Some of those needs include working on developing clean energy and a statewide grid, maintaining the Jones Act, and stimulating job growth and economic and environmental sustainability. Remember the Lingle Administration? Oahu Division Business Agent Paris Fernandez, Local Secretary-Treasurer Governor Linda Lingle and Lieutenant Guy Fujimura, U.S. Senator Brian Schatz, Oahu Division Representative Jose Governor James “Duke” Aiona opposed Miramontes and Oahu Division Business Agent Dillon Hullinger at the Hawaii or used the power of the governor’s Labor Unity Picnic at the Waikiki Shell on Labor Day, September 1, 2014. On the Inside veto to block nearly every single issue 1,100 Foodland members that was important to Hawaii’s working in the best interests of working people, and principles of the ILWU. We can ratify contract ........................... -

STATE of HAWAII Testimony COMMENTING on HB1896
DAVID Y. IGE VIRGINIA PRESSLER, M.D. GOVERNOR OF HAWAII DIRECTOR OF HEALTH STATE OF HAWAII DEPARTMENT OF HEALTH P. O. Box 3378 Honolulu, HI 96801-3378 [email protected] Testimony COMMENTING on HB1896 RELATING TO HEALTH. REP. JOHN M. MIZUNO, CHAIR HOUSE COMMITTEE ON HEALTH & HUMAN SERVICES Hearing Date: January 24, 2018 Room Number: 329 1 Fiscal Implications: None for Department of Health. 2 Department Testimony: The Department of Health supports the intent of HB1896, which is to 3 review health care policies, the Affordable Care Act, and other jurisdictions' health care 4 legislative proposals to determine ways the state can increase access to health care. However, 5 the department respectfully requests that proposals for increasing access to health care be 6 postponed until after a health analytics program is established and operational. 7 Based on the references the task force shall study, HB1896 appears to focus on the affordability 8 of health insurance. However, increasing access to health care also depends on a strong public 9 health infrastructure, supportive primary prevention policies, adequate provider supply, robust 10 health care analytics, and patient health literacy. 11 The Department of Health, in collaboration with other Cabinet agencies like the Department of 12 Human Services, the Department of Commerce and Consumer Affairs, the Department of Labor 13 and Industrial Relations, and the University of Hawaii, as well as private sector stakeholders, 14 discuss and prioritize these key components of health care access. 15 It is therefore noteworthy to call attention to HB2361, Relating to Health Analytics, which is part 16 of the Governor’s Administrative Package from the Department of Human Services, that calls for 17 resources and authority to establish a health analytics program to study both clinical and 18 financial health data. -

Financial Audit of GMO Money Blocking a GMO Labeling Bill
Financial Audit of GMO Money blocking a GMO Labeling Bill Politicians allow experimental GMO field trials near our homes, schools & oceans Our Politicians have turned our ‘Aina into a Chemical Wasteland The final deadline to hear a GMO labeling bill is gone, and the Chairpersons of both Senate and House Agriculture, Health, and Economic Development/Consumer Protection Committees refuse to hold a hearing. In November we will vote these corrupt Committee Chairpersons out that blocked a GMO labeling bill this year: Senate: Clarence Nishihara, Rosalyn Baker House: Clift Tsuji, Calvin Say, Ryan Yamane, Bob Herkes GMO Money to State Legislators 2008 2009 2011 Neil Abercrombie 1,000 1,500 Rosalyn Baker 750 500 500 (1,500) Kirk Caldwell 550 (Fred Perlak 500) Jerry Chang 500 500 Isaac Choy 500 Suzanne Chun Oakland 1000 Ty Cullen 250 Donovan Dela Cruz 500 (Dow 500) Will Espero 500 500 Brickwood Galuteria 500 Colleen Hanabusa 500 Mufi Hannemann (Dean Okimoto) 250 1,000 Sharon Har 1,000 1,000 500 Clayton Hee 1,000 500 (2,000) (Dow 500) (Syngenta 1000) Bob Herkes 750 500 500 Ken Ito 500 500 500 Gil Kahele 500 Daryl Kaneshiro 200 Michelle Kidani 250 500 (Dow 500) (DuPont 500) (Perlak 500) Donna Mercado Kim 1,000 Russell Kokubun 500 Ronald Kouchi 500 Sylvia Luke 250 (Perlak 500) Joe Manahan 500 500 Ernie Martin (Alicia Maluafiti) 250 (Perlak 500) Barbara Marumoto (Bayer 500) Angus McKelvey 500 Clarence Nishihara 750 500 Scott Nishimoto (Syngenta 250) GMO MONEY 2008 2009 2011 Blake Oshiro (Fred Perlak) 500 Calvin Say 2010 Biotech Legislator 1,000 500 -

April 1, 2010 the Honorable John M. Mizuno, Chair House Committee On
STATE OF HAWAII STATE COUNCIL ON DEVELOPMENTAL DISABILITIES 919 ALA MOANA BOULEVARO, ROOM 113 HONOLULU, HAWAII ,96814 TELEPHONE: (608) 566-8100 FAX: (808) 586-7543 April 1, 2010 The Honorable John M. Mizuno, Chair House Committee on Human Services and . The Honorable Suzanne Chun Oakland, Chair Senate Committee on Human Services Twenty-Fifth Legislature State Capitol State of Hawaii Honolulu, Hawaii 96813 Dear Representative Mizuno and Senator Chun Oakland and Members of the Committees: SUBJECT: Informational Briefing on the Department of Human Services' (DHS) Actions to Eliminate 228 DHS Employees from the Benefit, Employment and Support Services Division, Med-Quest Division, and Other Functions of the Department Without Meaningful Consultation with the Affected Employees and/or Their Union Representatives The position and views expressed in this testimony do not represent nor reflect the position and views of the Department of Health (DOH) or Department of Human Services (DHS). The State Council on Developmental Disabilities (DD) is very concerned about DHS's proposed reorganization of the Benefits, Employment, Support Services and Med-Quest Divisions into the Electronic Processing and Operations Division (EPOD). The proposed reorganization would create EPOD to save money and streamline operations for eligibility. We are greatly concerned that rather than save money and streamline operations, the result would be more costly to the State, and create chaos and mass confusion for recipients. People with DD will be directly impacted by this proposed reorganization. Due to their disability (intellectual and/or physical), they may not be able to use a computer or fax machine, or have access to the equipment. -
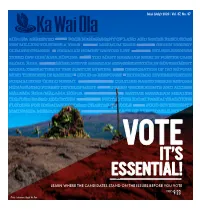
Learn Where the Candidates Stand on the Issues Before
Iulai (July) 2020 | Vol. 37, No. 07 VOTE IT’S ESSENTIAL! LEARN WHERE THE CANDIDATES STAND ON THE ISSUES BEFORE YOU VOTE PAGES 9-23 Photo: Lehuanani Waipä Ah Nee MARK YOUR CALENDARS! DID YOU FINAL DAY TO REGISTER TO RECEIVE BALLOT BY MAIL KNOW... go to olvr.hawaii.gov to register online ▸ 16-year-olds can CHECK YOUR MAIL! pre-register to vote? Delivery of ballot packages begin ▸ If you will be 18 by PLACE YOUR BALLOT IN election day, that you THE MAIL BY THIS DATE! can vote? Ballots must be received by August 8 at 7:00 pm ▸ You can register to vote on your phone? ▸ Hawai‘i has mail-in elections this year? HOW TO VOTE BY MAIL YOUR MAIL BALLOT WILL INCLUDE: GO TO olvr.hawaii.gov TO REGISTER TO VOTE 1. BALLOT 2. SECRET BALLOT 3. RETURN Before voting your ballot, review ENVELOPE ENVELOPE instructions and the contests and After voting your ballot, re-fold it and Read the affirmation statement and candidates on both sides of the seal it in the secret ballot envelope. sign the return envelope before ballot. To vote, completely darken in The secret ballot envelope ensures returning it to the Clerk’s Office. Upon the box to the left of the candidate your right to secrecy as the ballots are receipt of your return envelope, the using a black or blue pen. opened and prepared for counting. Once Clerk’s Office validates the signature sealed, place the secret ballot envelope on the envelope. After your signature is in the return envelope.