2159-8290.CD-21-0007.Full-Text.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
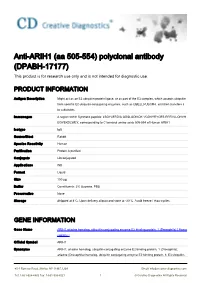
Anti-ARIH1 (Aa 505-554) Polyclonal Antibody (DPABH-17177) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-ARIH1 (aa 505-554) polyclonal antibody (DPABH-17177) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Antigen Description Might act as an E3 ubiquitin-protein ligase, or as part of the E3 complex, which accepts ubiquitin from specific E2 ubiquitin-conjugating enzymes, such as UBE2L3/UBCM4, and then transfers it to substrates. Immunogen A region within Synthetic peptide: LSGYLERDIS QDSLQDIKQK VQDKYRYCES RRRVLLQHVH EGYEKDLWEY, corresponding to C terminal amino acids 505-554 of Human ARIH1 Isotype IgG Source/Host Rabbit Species Reactivity Human Purification Protein A purified Conjugate Unconjugated Applications WB Format Liquid Size 100 μg Buffer Constituents: 2% Sucrose, PBS Preservative None Storage Shipped at 4°C. Upon delivery aliquot and store at -20°C. Avoid freeze / thaw cycles. GENE INFORMATION Gene Name ARIH1 ariadne homolog, ubiquitin-conjugating enzyme E2 binding protein, 1 (Drosophila) [ Homo sapiens ] Official Symbol ARIH1 Synonyms ARIH1; ariadne homolog, ubiquitin-conjugating enzyme E2 binding protein, 1 (Drosophila); ariadne (Drosophila) homolog, ubiquitin conjugating enzyme E2 binding protein, 1; E3 ubiquitin- 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 1 © Creative Diagnostics All Rights Reserved protein ligase ARIH1; ARI; ariadne; Drosophila; homolog of; HARI; HHARI; UBCH7BP; ARI-1; MOP-6; H7-AP2; monocyte protein 6; ubcH7-binding protein; protein ariadne-1 homolog; ubcM4- interacting protein; ariadne, -

ARIH1 (NM 005744) Human Untagged Clone – SC116547 | Origene
OriGene Technologies, Inc. 9620 Medical Center Drive, Ste 200 Rockville, MD 20850, US Phone: +1-888-267-4436 [email protected] EU: [email protected] CN: [email protected] Product datasheet for SC116547 ARIH1 (NM_005744) Human Untagged Clone Product data: Product Type: Expression Plasmids Product Name: ARIH1 (NM_005744) Human Untagged Clone Tag: Tag Free Symbol: ARIH1 Synonyms: ARI; HARI; HHARI; UBCH7BP Vector: pCMV6-XL5 E. coli Selection: Ampicillin (100 ug/mL) Cell Selection: None This product is to be used for laboratory only. Not for diagnostic or therapeutic use. View online » ©2021 OriGene Technologies, Inc., 9620 Medical Center Drive, Ste 200, Rockville, MD 20850, US 1 / 4 ARIH1 (NM_005744) Human Untagged Clone – SC116547 Fully Sequenced ORF: >OriGene sequence for NM_005744 edited GAATTCGGCACGAGGCAGCCGTCAAACGCCAACCGCCGCTCCTGGGGAGGAGCCGCGGCT CGCGGGGCCGGAGCCAGGCCTGCGTCCGGACATCAGCCGGAGCCGGAGCGAGAGCCGGGG CCTCGGCGTCCCCGCCCTCTCCCCGCCTCGGCCAGCGTCCGCCGGGCCCCCGCGCGTCGC GCCATGGACTCGGACGAGGGCTACAACTACGAGTTCGACGAGGACGAGGAGTGCAGTGAG GAGGACAGCGGCGCCGAGGAGGAGGAGGACGAAGACGACGACGAGCCGGACGATGATACC CTGGATCTGGGCGAGGTGGAGCTGGTGGAGCCCGGGCTGGGCGTCGGCGGGGAGCGGGAC GGACTGCTGTGCGGGGAGACGGGCGGTGGCGGCGGCAGCGCTCTGGGGCCCGGCGGTGGC GGCGGCGGCGGCGGCGGCGGTGGTGGTGGCGGGCCGGGGCATGAGCAGGAGGAGGATTAC CGCTACGAGGTGCTCACGGCCGAGCAGATTCTACAACACATGGTGGAATGTATCCGGGAG GTCAACGAGGTCATCCAGAATCCAGCAACTATCACAAGAATACTCCTTAGCCACTTCAAT TGGGATAAAGAGAAGCTAATGGAAAGGTACTTTGATGGAAACCTGGAGAAGCTCTTTGCT GAGTGTCATGTAATTAATCCAAGTAAAAAGTCTCGAACACGCCAGATGAATACAAGGTCA TCAGCACAGGATATGCCTTGTCAGATCTGCTACTTGAACTACCCTAACTCGTATTTCACT -

A High Throughput, Functional Screen of Human Body Mass Index GWAS Loci Using Tissue-Specific Rnai Drosophila Melanogaster Crosses Thomas J
Washington University School of Medicine Digital Commons@Becker Open Access Publications 2018 A high throughput, functional screen of human Body Mass Index GWAS loci using tissue-specific RNAi Drosophila melanogaster crosses Thomas J. Baranski Washington University School of Medicine in St. Louis Aldi T. Kraja Washington University School of Medicine in St. Louis Jill L. Fink Washington University School of Medicine in St. Louis Mary Feitosa Washington University School of Medicine in St. Louis Petra A. Lenzini Washington University School of Medicine in St. Louis See next page for additional authors Follow this and additional works at: https://digitalcommons.wustl.edu/open_access_pubs Recommended Citation Baranski, Thomas J.; Kraja, Aldi T.; Fink, Jill L.; Feitosa, Mary; Lenzini, Petra A.; Borecki, Ingrid B.; Liu, Ching-Ti; Cupples, L. Adrienne; North, Kari E.; and Province, Michael A., ,"A high throughput, functional screen of human Body Mass Index GWAS loci using tissue-specific RNAi Drosophila melanogaster crosses." PLoS Genetics.14,4. e1007222. (2018). https://digitalcommons.wustl.edu/open_access_pubs/6820 This Open Access Publication is brought to you for free and open access by Digital Commons@Becker. It has been accepted for inclusion in Open Access Publications by an authorized administrator of Digital Commons@Becker. For more information, please contact [email protected]. Authors Thomas J. Baranski, Aldi T. Kraja, Jill L. Fink, Mary Feitosa, Petra A. Lenzini, Ingrid B. Borecki, Ching-Ti Liu, L. Adrienne Cupples, Kari E. North, and Michael A. Province This open access publication is available at Digital Commons@Becker: https://digitalcommons.wustl.edu/open_access_pubs/6820 RESEARCH ARTICLE A high throughput, functional screen of human Body Mass Index GWAS loci using tissue-specific RNAi Drosophila melanogaster crosses Thomas J. -
Uncovering New Mechanisms of Cdc34 and Cullin-Ring Activity
UNLV Theses, Dissertations, Professional Papers, and Capstones 12-15-2019 Uncovering New Mechanisms of Cdc34 and Cullin-Ring Activity Spencer Hill Follow this and additional works at: https://digitalscholarship.unlv.edu/thesesdissertations Part of the Biochemistry Commons Repository Citation Hill, Spencer, "Uncovering New Mechanisms of Cdc34 and Cullin-Ring Activity" (2019). UNLV Theses, Dissertations, Professional Papers, and Capstones. 3808. http://dx.doi.org/10.34917/18608668 This Dissertation is protected by copyright and/or related rights. It has been brought to you by Digital Scholarship@UNLV with permission from the rights-holder(s). You are free to use this Dissertation in any way that is permitted by the copyright and related rights legislation that applies to your use. For other uses you need to obtain permission from the rights-holder(s) directly, unless additional rights are indicated by a Creative Commons license in the record and/or on the work itself. This Dissertation has been accepted for inclusion in UNLV Theses, Dissertations, Professional Papers, and Capstones by an authorized administrator of Digital Scholarship@UNLV. For more information, please contact [email protected]. UNCOVERING NEW MECHANISMS OF CDC34 AND CULLIN-RING ACTIVITY By Spencer Wayne Hill Bachelor of Science in Biochemistry University of Nevada, Las Vegas 2013 A dissertation submitted in partial fulfillment of the requirements for the Doctor of Philosophy - Chemistry Department of Chemistry and Biochemistry College of Sciences The Graduate College University of Nevada, Las Vegas December 2019 Dissertation Approval The Graduate College The University of Nevada, Las Vegas November 1st, 2019 This dissertation prepared by Spencer Wayne Hill entitled Uncovering New Mechanisms of Cdc34 and Cullin-Ring Activity is approved in partial fulfillment of the requirements for the degree of Doctor of Philosophy - Chemistry Department of Chemistry and Biochemistry Gary Kleiger, Ph.D. -

Supplementary Information Supplement To: Large-Scale Identification of Clonal Hematopoiesis and Mutations Recurrent in Blood Cancers
Supplementary Information Supplement to: Large-Scale Identification of Clonal Hematopoiesis and Mutations Recurrent in Blood Cancers Julie E. Feusier, Sasi Arunachalam, Tsewang Tashi, Monika J. Baker, Chad VanSant-Webb, Amber Ferdig, Bryan E. Welm, Christopher Ours, Juan L. Rodriguez-Flores, Lynn B. Jorde, Josef T. Prchal, Clinton C. Mason (JEF and SA contributed equally.) Department of Pediatrics, Division of Pediatric Hematology and Oncology, University of Utah, Salt Lake City, Utah (JEF, SA, MJB, CVS-W, AF, CO, CCM); Department of Human Genetics, University of Utah, Salt Lake City, Utah (JEF, LBJ); Huntsman Cancer Institute, University of Utah, Salt Lake City, Utah (SA, TT, BEW, JTP); Department of Oncological Sciences, University of Utah, Salt Lake City, Utah (SA); Division of Hematology and Hematologic Malignancies, University of Utah, Salt Lake City, Utah (TT, JTP); VA Medical Center, Salt Lake City, Utah (TT, JTP); Department of Surgery, University of Utah, Salt Lake City, Utah (BEW); Department of Genetic Medicine, Weill Cornell Medical College, New York, New York (JLR-F) Table of Contents Supp. Methods ………………………………….………………...……….…….… 2 Supp. Figure 1. ………………………………….………………...……….…….… 9 Supp. Figure 2. ………………………………….…………………….………..… 10 Supp. Figure 3. ………………………………….…………………….………..… 11 Supp. Figure 4. ………………………………….…………………….………..… 12 Supp. Figure 5. ………………………………….…………………….………..… 14 1 Supplementary Methods. A. Hotspot mutation analysis: Criteria for inclusion of somatic mutation studies and samples Of the identified somatic mutation studies, only those meeting sample identifiability criteria were included in an effort to include only mutations from diagnostic samples and to greatly reduce the likelihood of an individual’s mutations being included twice in our extraction process. Studies were required to have assessed somatic mutations with NGS methods in eight or more diagnostic samples of one of seven hematologic malignancies (ALL, AML, CML, CMML, JMML, MDS, and MPN). -

Promoterless Transposon Mutagenesis Drives Solid Cancers Via Tumor Suppressor Inactivation
bioRxiv preprint doi: https://doi.org/10.1101/2020.08.17.254565; this version posted August 17, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. 1 Promoterless Transposon Mutagenesis Drives Solid Cancers via Tumor Suppressor Inactivation 2 Aziz Aiderus1, Ana M. Contreras-Sandoval1, Amanda L. Meshey1, Justin Y. Newberg1,2, Jerrold M. Ward3, 3 Deborah Swing4, Neal G. Copeland2,3,4, Nancy A. Jenkins2,3,4, Karen M. Mann1,2,3,4,5,6,7, and Michael B. 4 Mann1,2,3,4,6,7,8,9 5 1Department of Molecular Oncology, Moffitt Cancer Center & Research Institute, Tampa, FL, USA 6 2Cancer Research Program, Houston Methodist Research Institute, Houston, Texas, USA 7 3Institute of Molecular and Cell Biology, Agency for Science, Technology and Research (A*STAR), 8 Singapore, Republic of Singapore 9 4Mouse Cancer Genetics Program, Center for Cancer Research, National Cancer Institute, Frederick, 10 Maryland, USA 11 5Departments of Gastrointestinal Oncology & Malignant Hematology, Moffitt Cancer Center & Research 12 Institute, Tampa, FL, USA 13 6Cancer Biology and Evolution Program, Moffitt Cancer Center & Research Institute, Tampa, FL, USA 14 7Department of Oncologic Sciences, Morsani College of Medicine, University of South Florida, Tampa, FL, 15 USA. 16 8Donald A. Adam Melanoma and Skin Cancer Research Center of Excellence, Moffitt Cancer Center, Tampa, 17 FL, USA 18 9Department of Cutaneous Oncology, Moffitt Cancer Center & Research Institute, Tampa, FL, USA 19 These authors contributed equally: Aziz Aiderus, Ana M. -

LETTER Doi:10.1038/Nature12364
LETTER doi:10.1038/nature12364 Genetic programs in human and mouse early embryos revealed by single-cell RNA sequencing Zhigang Xue1*, Kevin Huang2*, Chaochao Cai2, Lingbo Cai3, Chun-yan Jiang3, Yun Feng1, Zhenshan Liu1, Qiao Zeng1, Liming Cheng1, Yi E. Sun1, Jia-yin Liu3, Steve Horvath2 & Guoping Fan2 Mammalian pre-implantation development is a complex process Intriguingly, cluster analyses showed that both pronuclear and involving dramatic changes in the transcriptional architecture1–4. zygote (1-cell stage) embryos clustered closely together but away from We report here a comprehensive analysis of transcriptome dynamics oocytes and cleavage embryos, indicating that the 1-cell stage exhibits a from oocyte to morula in both human and mouse embryos, using distinct transcriptome pattern. Comparisons between mature oocytes single-cell RNA sequencing. Based on single-nucleotide variants in and 1-cell embryos identified 149 differentially expressed genes (false human blastomere messenger RNAs and paternal-specific single- discovery rate (FDR) , 5%, .2-fold change), 79 and 70 of which were nucleotide polymorphisms, we identify novel stage-specific mono- up- and downregulated in 1-cell embryos, respectively (Fig. 1c). Inter- allelic expression patterns for a significant portion of polymorphic estingly, approximately half of the upregulated genes remain highly gene transcripts (25 to 53%). By weighted gene co-expression network expressed in 2- and 4-cell stages but are downregulated at the 8-cell analysis5,6, we find that each developmental stage can be delineated stage, whereas the other half is further upregulated at the 8-cell stage concisely by a small number of functional modules of co-expressed (Fig. -

Structure and Function of Multimeric BTB Proteins and Cullin3 Substrate Adaptors
Structure and Function of Multimeric BTB Proteins and Cullin3 Substrate Adaptors by Xian Alan Ji A thesis submitted in conformity with the requirements for the degree of Doctor of Philosophy Graduate Department of Biochemistry University of Toronto © Copyright by Xian Alan Ji 2017 ii Structure and Function of Multimeric BTB Proteins and Cullin3 Substrate Adaptors Xian Alan Ji Doctor of Philosophy Department of Biochemistry University of Toronto 2017 Abstract Oligomerization and ubiquitylation are fundamental to the function of many proteins. Protein oligomerization confers numerous advantages including allosteric regulation, increased coding efficiency, and reduced transcriptional and translational error rates. Ubiquitylation is a widespread post-translational modification that targets modified proteins to a variety of fates including degradation by the 26S proteasome. Dysfunctional protein degradation is a common mechanism shared by a diverse range of human diseases. Many members of the BTB domain superfamily have roles centered on protein oligomerization and ubiquitylation. The BTB domain can facilitate self-assembly to form dimers, tetramers, and pentamers. In addition, many BTB proteins provide substrate specificity for the Cullin3 (Cul3) E3 ubiquitin ligase. Dysfunctional BTB/Cullin3 ubiquitinylation complexes are involved in certain forms of prostate cancer, medulloblastoma, hereditary hypertension and other diseases. Thus, understanding the details of BTB protein oligomerization and Cul3 interaction is important towards many aspects of human disease. The research presented in this thesis addresses several areas of BTB/Cul3 biology. The mechanism of dimeric BTB protein to Cul3 association was expanded to include the contributions iii from the BACK domain observed in the crystal structure of KLHL3/Cul3. Several KLHL3 mutations associated with familial hypertension were found to disrupt Cul3 binding. -

University of California San Diego
UNIVERSITY OF CALIFORNIA SAN DIEGO Regulation of Ubiquitylation and Ubiquitin-like Post-Translational Modifications A dissertation submitted in partial satisfaction of the requirements for the degree of Doctor of Philosophy in Chemistry by Ryan James Lumpkin Committee in charge: Professor Elizabeth A. Komives, Chair Professor Rommie Amaro Professor Gouri Ghosh Professor Randy Hampton Professor Susan Taylor 2019 Copyright Ryan James Lumpkin, 2019 All rights reserved The dissertation of Ryan James Lumpkin is approved, and it is acceptable in quality and form for publication on microfilm and electronically: Chair University of California San Diego 2019 iii DEDICATION To my parents who have helped me get this far, my friends who supported me along the way, my PI who believed in me, and my cat who was always waiting for me. iv TABLE OF CONTENTS Signature page.....................................................................................................................iii Dedication............................................................................................................................iv Table of Contents..................................................................................................................v List of Abbreviations............................................................................................................xi Lists of Figures...................................................................................................................xiii Lists of Tables....................................................................................................................xvi -

Promoterless Transposon Mutagenesis Drives Solid Cancers Via Tumor Suppressor Inactivation
cancers Article Promoterless Transposon Mutagenesis Drives Solid Cancers via Tumor Suppressor Inactivation Aziz Aiderus 1,† , Ana M. Contreras-Sandoval 1,† , Amanda L. Meshey 1,†, Justin Y. Newberg 1,2,‡, Jerrold M. Ward 3,§, Deborah A. Swing 4, Neal G. Copeland 2,3,4,k, Nancy A. Jenkins 2,3,4,k, Karen M. Mann 1,2,3,4,5,6,7,* and Michael B. Mann 1,2,3,4,6,7,8,9,* 1 Department of Molecular Oncology, Moffitt Cancer Center & Research Institute, Tampa, FL 33612, USA; Aziz.Aiderus@moffitt.org (A.A.); Ana.ContrerasSandoval@moffitt.org (A.M.C.-S.); Amanda.Meshey@moffitt.org (A.L.M.); [email protected] (J.Y.N.) 2 Cancer Research Program, Houston Methodist Research Institute, Houston, TX 77030, USA; [email protected] (N.G.C.); [email protected] (N.A.J.) 3 Institute of Molecular and Cell Biology, Agency for Science, Technology and Research (A*STAR), Singapore 138673, Singapore; [email protected] 4 Mouse Cancer Genetics Program, Center for Cancer Research, National Cancer Institute, Frederick, MD 21702, USA; [email protected] 5 Departments of Gastrointestinal Oncology & Malignant Hematology, Moffitt Cancer Center & Research Institute, Tampa, FL 33612, USA 6 Cancer Biology and Evolution Program, Moffitt Cancer Center & Research Institute, Tampa, FL 33612, USA 7 Department of Oncologic Sciences, Morsani College of Medicine, University of South Florida, Tampa, FL 33612, USA 8 Donald A. Adam Melanoma and Skin Cancer Research Center of Excellence, Moffitt Cancer Center, Tampa, FL 33612, USA 9 Department of Cutaneous Oncology, Moffitt Cancer Center & Research Institute, Tampa, FL 33612, USA * Correspondence: Karen.Mann@moffitt.org (K.M.M.); Michael.Mann@moffitt.org (M.B.M.) † These authors contributed equally. -
Biomedical Informatics
BIOMEDICAL INFORMATICS Abstract GENE LIST AUTOMATICALLY DERIVED FOR YOU (GLAD4U): DERIVING AND PRIORITIZING GENE LISTS FROM PUBMED LITERATURE JEROME JOURQUIN Thesis under the direction of Professor Bing Zhang Answering questions such as ―Which genes are related to breast cancer?‖ usually requires retrieving relevant publications through the PubMed search engine, reading these publications, and manually creating gene lists. This process is both time-consuming and prone to errors. We report GLAD4U (Gene List Automatically Derived For You), a novel, free web-based gene retrieval and prioritization tool. The quality of gene lists created by GLAD4U for three Gene Ontology terms and three disease terms was assessed using ―gold standard‖ lists curated in public databases. We also compared the performance of GLAD4U with that of another gene prioritization software, EBIMed. GLAD4U has a high overall recall. Although precision is generally low, its prioritization methods successfully rank truly relevant genes at the top of generated lists to facilitate efficient browsing. GLAD4U is simple to use, and its interface can be found at: http://bioinfo.vanderbilt.edu/glad4u. Approved ___________________________________________ Date _____________ GENE LIST AUTOMATICALLY DERIVED FOR YOU (GLAD4U): DERIVING AND PRIORITIZING GENE LISTS FROM PUBMED LITERATURE By Jérôme Jourquin Thesis Submitted to the Faculty of the Graduate School of Vanderbilt University in partial fulfillment of the requirements for the degree of MASTER OF SCIENCE in Biomedical Informatics May, 2010 Nashville, Tennessee Approved: Professor Bing Zhang Professor Hua Xu Professor Daniel R. Masys ACKNOWLEDGEMENTS I would like to express profound gratitude to my advisor, Dr. Bing Zhang, for his invaluable support, supervision and suggestions throughout this research work. -

Downloaded from Here
bioRxiv preprint doi: https://doi.org/10.1101/017566; this version posted April 6, 2015. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. 1 1 Testing for ancient selection using cross-population allele 2 frequency differentiation 1;∗ 3 Fernando Racimo 4 1 Department of Integrative Biology, University of California, Berkeley, CA, USA 5 ∗ E-mail: [email protected] 6 1 Abstract 7 A powerful way to detect selection in a population is by modeling local allele frequency changes in a 8 particular region of the genome under scenarios of selection and neutrality, and finding which model is 9 most compatible with the data. Chen et al. [1] developed a composite likelihood method called XP-CLR 10 that uses an outgroup population to detect departures from neutrality which could be compatible with 11 hard or soft sweeps, at linked sites near a beneficial allele. However, this method is most sensitive to recent 12 selection and may miss selective events that happened a long time ago. To overcome this, we developed 13 an extension of XP-CLR that jointly models the behavior of a selected allele in a three-population three. 14 Our method - called 3P-CLR - outperforms XP-CLR when testing for selection that occurred before two 15 populations split from each other, and can distinguish between those events and events that occurred 16 specifically in each of the populations after the split.