BCPS J Sept. 07 Make.Qxd
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Bangladesh Development Bibliography List of Publications from 2000 – 2005 (As of January 16, 2012)
Bangladesh Development Bibliography List of publications from 2000 – 2005 (as of January 16, 2012) Aaby, Peter; Abbas Bhuiya; Lutfun Nahar; Kim Knudsen; Andres de Francisco; and Michael Strong (2003) The survival benefit of measles immunization may not be explained entirely by the prevention of measles disease: a community study from rural Bangladesh ; International Journal of Epidemiology, Vol. 32, No. 1 (February), pp. 106-115. Abbasi, Kamran (2002) Health policy in action: the World Bank in South Asia; Brighton, UK: University of Sussex, Institute of Development Studies (IDS). Abdalla, Amr; A. N. M. Raisuddin; and Suleiman Hussein with the assistance of Dhaka Ahsania Mission (2004) Bangladesh Educational Assessment - Pre-primary and Primary Madrasah Education in Bangladesh ; Washington, DC, USA: United States Agency for International Development (USAID) for Basic Education and Policy Support (BEPS) Activity (Contract No. HNE-I-00-00-00038-00) (June). Abdullah, Abu (2001) The Bangladesh Economy in the Year 2000: Achievements and Failures; In: Abu Abdullah (ed.) Bangladesh Economy 2000: Selected issues (Dhaka: Bangladesh Institute of Development Studies (BIDS)), pp. xv-xxix. Abdullah, Abu (ed.) (2001) Bangladesh Economy 2000: Selected Issues; Dhaka, Bangladesh: University Press Ltd. and Bangladesh Institute of Development Studies. Abdullah, Abu A. (2000) Social Change and ‘Modernisation‘; In: Rounaq Jahan (ed.) Bangladesh: Promise and Performance (London, UK: Zed Books; and Dhaka, Bangladesh: The University Press), Chapter 5. Abdullah, Mohammad (ed.) (2004) Technologies on Livestock and Fisheries for Poverty Alleviation in SAARC Countries; Dhaka, Bangladesh: SAARC Agricultural Information Centre (SAIC). Abdullah, S. T.; Mullineux, A. W.; Fielding, A.; and W. Spanjers (2004) Intra-household resource allocation and bargaining power of the women using micro-credit in Bangladesh; Birmingham, UK: University of Birmingham, Department of Economics Discussion Paper, No. -

Preliminary Voters' List Bgmea Election 2011
PRELIMINARY VOTERS' LIST BGMEA ELECTION 2011 - 2012 Bangladesh Garment Manufacturers & Exporters Association (BGMEA) BGMEA Complex, 23/1 Panthapath Link Road, Karwan Bazar, Dhaka-1215 Tel: 8802-8115751, Fax: 8802-8113951, Email: [email protected] ZONE : DHAKA Md. Hamidul Haque Khan Mohd. Idris Shakur 4 Star Fashions Ltd. (Reg. 3081) 4 You Clothing Ltd. (Reg. 2914) 385/1, East Rampura, (6th Floor) 367/1, Senpara Parbata(4th & 5th Fl) Rampura, Dhaka-1219 Mirpur, Dhaka-1216 TIN: 003-201-0502 Voter ID # 1 TIN: 107-200-8479 Voter ID # 2 Lt. ABM Abdullah (Retd) ATM Shamsuzzaman 4A Yarn Dyeing Ltd. (Reg. 4121) 4S-Park Style Ltd. (Reg. 4598) 139, Outer Circular Road Plot # 152/9, Road # 9/2, Block - B, Section # 12 Moghbazar, Dhaka-1217 Mirpur, Dhaka-1216 TIN: 003-201-7819 Voter ID # 3 TIN: 003-201-9566 Voter ID # 4 Monowara Begum Md. Mahbubul Alam A & A Fashion Sweaters Ltd. (Reg. 3968) A & A Trousers Ltd. (Reg. 4671) Naljani (Wireless Gate) House # B-109 (Duplex), Road # 8, New DOHS Sadar, Gazipur Mohakhali, Dhaka-1206 TIN: 003-201-6041 Voter ID # 5 TIN: 042-200-8587 Voter ID # 6 N.M. Habibur Rahman Anwar Hossain Chowdhury A & H Enterprises Ltd. (Reg. 2190) A J Fashions Ltd. (Reg. 3236) 93, Motijheel C/A, (2nd floor) 2, Monipuripara (4th Floor) Motijheel, Dhaka-1000 Tejgaon, Dhaka-1215 TIN: 002-200-3819 Voter ID # 7 TIN: 002-201-3329 Voter ID # 8 Md. Golam Mortuza Waris Mohiuddin Ahamad Bhuiyan A One Dress Makers Ltd. (Reg. 4179) A Plus Industries Ltd. (Reg. 4221) 1703, Rayerbag, Dania 30, Dilu Road, New Eskaton Shampur, Dhaka-1236 Eskaton, Dhaka TIN: 010-200-1143 Voter ID # 9 TIN: 006-200-3231 Voter ID # 10 Saifuddin Ahmed Bhuiyan Md. -

Dhaka-Zone-2013-2014.Pdf
PRELIMINARY VOTERS' LIST BGMEA ELECTION 2013-2014 Bangladesh Garment Manufacturers & Exporters Association (BGMEA) BGMEA Complex, 23/1 Panthapath Link Road, Karwan Bazar, Dhaka-1215 Tel: +88-02-8140310-20, Fax: +88-02-8140322-23, Email: [email protected] ZONE : DHAKA (TOTAL : 2506) Md. Hamidul Haque Khan Mohd. Idris Shakur 4 Star Fashions Ltd. (Reg. 3081) 4 You Clothing Ltd. (Reg. 2914) 385/1, East Rampura, (6th Floor) 367/1, Senpara Parbota, Section # 10 Rampura, Dhaka-1219 Mirpur, Dhaka-1216 TIN: 003-201-0502 TIN: 107-200-8479 Abdullah Hil Rakib ATM Shamsuzzaman 4A Yarn Dyeing Ltd. (Reg. 4121) 4S-Park Style Ltd. (Reg. 4598) House # 10, Road # 14, Sector # 01 Plot # 152/9, Road # 9/2, Block - B, Section # 12 Uttara, Dhaka-1230 Mirpur, Dhaka-1216 TIN: 003-201-7819 TIN: 003-201-9566 Monowara Begum Md. Mahbubul Alam A & A Fashion Sweaters Ltd. (Reg. 3968) A & A Trousers Ltd. (Reg. 4671) Naljani (Wireless Gate) House # B-109 (Duplex), Road # 8, New DOHS Sadar, Gazipur Mohakhali, Dhaka-1206 TIN: 003-201-6041 TIN: 042-200-8587 N.M. Habibur Rahman Anwar Hossain Chowdhury A & H Enterprises Ltd. (Reg. 2190) A J Fashions Ltd. (Reg. 3236) 93, Motijheel C/A, (2nd floor) 2, Monipuripara (4th Floor) Motijheel, Dhaka-1000 Tejgaon, Dhaka-1215 TIN: 002-200-3819 TIN: 002-201-3329 Md. Golam Mortuza Waris Mohiuddin Ahamad Bhuiyan A One Dress Makers Ltd. (Reg. 4179) A Plus Industries Ltd. (Reg. 4221) 1703, Rayerbag, Dania 26, Eskaton Shampur, Dhaka-1236 Garden Road, Dhaka TIN: 010-200-1143 TIN: 006-200-3231 Saifuddin Ahmed Bhuiyan Al-Haj Amjad Ali Bhuiyan A Plus Sweater (Reg. -

Sl. No. Name of the Investor IA. No. 1 AFZALUR RAHMAN 3 2 DR. AFAZUDDIN AHMED 5 3 M. RAHMAT ALI 12 4 ANWAR RAHIM 13 5 M. ASHRAF HUSAIN 14 6 AZHARUL ISLAM 15 7 MD
Sl. No. Name of the Investor IA. No. 1 AFZALUR RAHMAN 3 2 DR. AFAZUDDIN AHMED 5 3 M. RAHMAT ALI 12 4 ANWAR RAHIM 13 5 M. ASHRAF HUSAIN 14 6 AZHARUL ISLAM 15 7 MD. SHAMSUL ALAM 17 8 SK FAZLUL HAQUE 22 9 MD. AKRAM HUSSAIN 28 10 MONZURUR RAHMAN 31 11 ANISUL BARI CHOWDHURY 32 12 NOOR-UL-HAQ FARUK 33 13 SYED SHAHIDUZZAMAN 40 14 DELAWAR HOSSAIN 41 15 MRS. SURAIYA RAHMAN 42 16 PROF. MD. FAZLUL KARIM AKH. 51 17 N. A. AL-MASOOD 55 18 ABDUL BARIK CHOUDHURY 60 19 MRS. HOSNE ARA BEGAM 63 20 SHAMEENA NASRIN 68 21 MRS. AKTARI BEGUM 85 22 ROWSHAN ARA RAHMAN 87 23 A. M. M. HABIBUR RAHMAN. 99 24 MISBAHUL MANNAN 121 25 MD. ABDUL AZIM CHOUDHURY 122 26 ABDUR RAZZAQUE CHOUDHURY 123 27 ABDUL MANNAN CHOWDHURY 127 28 MRS. SALMA AZIZ 129 29 M. SYEDUR RAHMAN 134 30 MRS. TAHERA RAHMAN CHOWDHURY 138 31 SYED ABDUS SALIQUE 159 32 ABDUS SALAM CHOWDHURY 164 33 FAROOK RASHID CHOUDHURY 173 34 MRS. ZOHRA CHOUDHURY 174 35 MD. MUEED HOSSAIN 194 36 JAHANARA RASHID 197 37 GOURANGA CHANDRA BHAKTA 211 38 SYED SHIBLY AHMED 215 39 RANJAN RAHMAN CHOUDHURY 216 40 MRS. ROWSHAN ARA MAHMOOD 218 41 MD. YASIN 221 42 SIRAJUL ISLAM CHOUDHURY 228 43 ABDUL MOMIN CHOUDHURY 253 44 MISS. HASINA BARIK CHOU. 256 45 ROKEYA CHOUDHURY 258 46 MISS. ROKSANA BARIK CHOU. 259 47 KAISER REZA CHOWDHURY 267 48 ABDUL MAJID CHOWDHURY 268 Page 1 of 111 ICB Head Office, Dhaka 49 MD. MASHFU-UR-RAHMAN 281 50 BEGUM MONOWARA 282 51 MS. -

Fractional Amount 2016
Golden Harvest Agro Industries Limited Fractional Amount for the year 2016 SL NO BOID Name of Shareholders Father's Name Amount 1 1201470044336095 MARZIA NASIR PROFESSOR MD. NASIR ULLAH 44.79 2 1201500034231501 NASRIN MUKTI MD. JALAL UDDIN 24.88 3 1201510016962894 REZAUL KARIM ABDU ROOF MOZUMDER 44.79 4 1201510029138605 ABUL HOSSAIN BHUIYA ABDUL GOFRAN 4.97 5 1201510029138648 ABUL HOSSAIN BHUIYA ABDUL GOFRAN 44.79 6 1201510035815269 MOHAMMED AKASH BODIZZAMAN 29.86 7 1201510036675109 MD. MASUD RANA MD.NAZRUL ISLAM 44.79 8 1201510038139922 ABUL KALAM HASHEM PATHAN 29.86 9 1201510044398724 HOSSAIN MIZI LADU MIA MIZI 44.79 10 1201530000013044 MR.NURUL ISLAM LATE ABDUL KHALEQ 44.79 11 1201560016298087 DOULAT HOSSAIN Ali Akber 24.88 12 1201570033490844 SULTAN AHAMMED KABIR AHAMED 44.79 13 1201580032065584 FARHANA YASMIN A.M. NISAR 44.79 14 1201580035363838 H.M.NAZMUL HUDA MD.AOWLAD HOSSAIN 44.79 15 1201590019393230 MOHD. SHOWKAT HOSSAIN LATE SALEH ZAHUR 14.93 16 1201600016782519 MOMINUL HOQUE AMINUL HOQUE 24.88 17 1201690017551287 ABDUL KADIR Md.Badsha Dhali 44.79 18 1201690019361299 JASHIM UDDIN Abdul Khalek Bapari 44.79 19 1201690045091551 SHAIKH AKBER Shaikh Munsur 44.79 20 1201690045091584 SHAMSUDDIN AHMED Khadem Hossain 44.79 21 1201700027830908 MD. ASLAM Jabbar Bepari 24.88 22 1201720032202568 MR.SHORF ABUL HOSSAIN 44.79 23 1201720032202592 AOPO MIAH HARRON MIAH 44.79 24 1201770044923476 12332-TAREM OZAIR AHMED N. AHMED 24.88 25 1201780030382351 NEAMOT ULLAH SALA UDDIN 24.88 26 1201820045023657 SILVIA LEONI SARKER MARSAL RINKU SARKER 29.86 27 1201820047994003 MD.GOLAM KIBRIA MD.NAZIMUDDIN 29.86 28 1201830006857761 ARIFUR RAHMAN MAHMUD Md. -
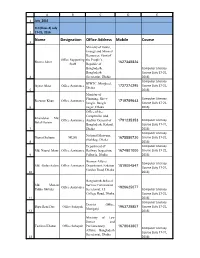
Name Designation Office Address Mobile Course
A B C D E 1 July_2016 CLC(Class-4) July 2 17-21, 2016 Name Designation Office Address Mobile Course 3 Ministry of Power, Energy and Mineral Resources, Govt of Office Supporting the People’s Resma Akter 1627348824 Staff Republic of Bangladesh, Computer Literacy Bangladesh Course (July 17-21, 4 Secretariat, Dhaka 2016) Computer Literacy BIWTC, Motijheel, Ayasa Akter Office Assistance 1727274295 Course (July 17-21, Dhaka 5 2016) Ministry of Planning, She-e- Computer Literacy Rezanur Khan Office Assistance 1719789643 bangla, Bangla Course (July 17-21, 6 nagar, Dhaka 2016) Office of the Comptroller and Khandakar Md. Office Assistance Auditor General of 1791235353 Computer Literacy Belal Hosain Bangladesh, Kakrail, Course (July 17-21, 7 Dhaka 2016) Computer Literacy National Museum, Nusrat Sultana MLSS 1675550730 Course (July 17-21, Shahbag, Dhaka 8 2016) Department of Computer Literacy Md. Nazrul Islam Office Assistance Railway Inspection, 1674801000 Course (July 17-21, 9 Fulbaria, Dhaka 2016) Women Affairs Computer Literacy Md. Abdus Salam Office Assistance Department, Eskaton 1819004547 Course (July 17-21, Garden Road, Dhaka 10 2016) Bangladesh Judicial Md. Mohsin Service Commission Office Assistance 1926625077 Uddin Shikder Secretariat, 15 Computer Literacy College Road, Dhaka Course (July 17-21, 11 2016) Computer Literacy District Office, Dipu Rani Das Office Sohayok 1963728857 Course (July 17-21, Musiganj 12 2016) Ministry of Law Justice and Taslima Khatun Office Sohayok Parliamentary 1678043807 Computer Literacy Affairs, Bangladesh Course (July 17-21, Secretariat, Dhaka 13 2016) A B C D E Computer Literacy Sakera Akter Office Assistance BCS Tax Academy 1980279636 Course (July 17-21, 14 2016) Labour Department, Computer Literacy Md. -
Voter List of the College of General Practitioners of Bangladesh
FELLOW LIST OF BANGLADESH COLLEGE OF GENERAL PRACTITIONERS Voter No. Name & Address Voter No. Name & Address F-1. Dr. Alhaj Md. Manirul Alam F-9. Dr. Md. Nurul Islam DEAD 64/2, R. K. Mission Road 3, D.I.T. Market Gopibagh 1st floor Dhaka. Narayangonj. Mob: 01 Mob: 01711524436 F-2. Dr. A. H. Akhand F-10. Dr. S. M. Mobarak Hossain DEAD House # 119/F, Road # 1 Noapara Surgical Clinic Banani Hospital Road, Noapara Dhaka. Jessore. Mob: 01 Mob: 01 F-3. Dr. M. A. Wahid F-11. Dr. Sailhamong Chowdhury House # 75, Road # 11/A Christian Hospital Apt. # B2 Chandraghona Dhanmondi R/A P.O. Chandraghona Dhaka. Dist. Rangamati. Mob: 01 Mob: 01 F-4. Dr. Md. Habibur Rahman F-12. Dr. Md. Shafiqur Rahman 42, Cantonment R/A 574/B, Nayatola Dhaka Cantonment Modhubagh Dhaka. Dhaka. Mob: 01711525448 Mob: 01 F-5. Dr. S. A. Mahmood F-13. Dr. Samir Uddin Ahmed 125, Gulshan Avenue Basunia Patty Gulshan-2 P.O. Dinajpur Dhaka. Dist. Dinajpur. Mob: 02-8828052 Mob: 01 F-6. Dr. Sarwar Alam Chowdhury F-14. Dr. Md. Reaz Uddin Medical Director Amir Mansion Medicare Services Ltd. Bank Road Lalkhan Bazar Kulaura Chittagong. Dist. Moulvibazar. Mob: 01 Mob: 01 F-7. Dr. Md. Abdur Rahim Khan F-15. Dr. Mazir Uddin Ahmed 13, Shurendranath Road DEAD Miah Fazil Ehist Shoshtitalapara Ambarkhana P.O. & Dist. Jessore. Sylhet. Mob: 01 Mob: 01 F-8. Dr. Shahida Rahman F-16. Dr. Md. Imtiaz Ali Member, Governing Body, BCGP 17, Elephant Road Rangs Water Front, Apt. # B-0 Balleria, Flat # 3/A House # 01, Road # 15 Dhaka. -

FINAL VOTERS' LIST BGMEA ELECTION 2013-2014 Bangladesh
FINAL VOTERS' LIST BGMEA ELECTION 2013-2014 Bangladesh Garment Manufacturers & Exporters Association (BGMEA) BGMEA Complex, 23/1 Panthapath Link Road, Karwan Bazar, Dhaka-1215 Tel: +88-02-8140310-20, Fax: +88-02-8140322-23, Email: [email protected] ZONE : DHAKA (TOTAL : 2592) Md. Hamidul Haque Khan Mohd. Idris Shakur 4 Star Fashions Ltd. (Reg. 3081) 4 You Clothing Ltd. (Reg. 2914) 385/1, East Rampura, (6th Floor) 367/1, Senpara Parbota, Section # 10 Rampura, Dhaka-1219 Mirpur, Dhaka-1216 TIN: 003-201-0502 Voter ID # : 1 TIN: 107-200-8479 Voter ID # : 2 Abdullah Hil Rakib ATM Shamsuzzaman 4A Yarn Dyeing Ltd. (Reg. 4121) 4S-Park Style Ltd. (Reg. 4598) House # 10, Road # 14, Sector # 01 Plot # 152/9, Road # 9/2, Block - B, Section # 12 Uttara, Dhaka-1230 Mirpur, Dhaka-1216 TIN: 003-201-7819 Voter ID # : 3 TIN: 003-201-9566 Voter ID # : 4 Kamran Sadique Monowara Begum 786 Garments & Textiles. (Reg. 674) A & A Fashion Sweaters Ltd. (Reg. 3968) 127, Azimpur Road Naljani (Wireless Gate) Lalbagh, Dhaka Sadar, Gazipur TIN: 450-300-2251 Voter ID # : 5 TIN: 003-201-6041 Voter ID # : 6 Md. Mahbubul Alam N.M. Habibur Rahman A & A Trousers Ltd. (Reg. 4671) A & H Enterprises Ltd. (Reg. 2190) House # B-109 (Duplex), Road # 8, New DOHS 93, Motijheel C/A, (2nd floor) Mohakhali, Dhaka-1206 Motijheel, Dhaka-1000 TIN: 042-200-8587 Voter ID # : 7 TIN: 002-200-3819 Voter ID # : 8 Anwar Hossain Chowdhury Md. Golam Mortuza Waris A J Fashions Ltd. (Reg. 3236) A One Dress Makers Ltd. (Reg. 4179) 2, Monipuripara (4th Floor) 1703, Rayerbag, Dania Tejgaon, Dhaka-1215 Shampur, Dhaka-1236 TIN: 002-201-3329 Voter ID # : 9 TIN: 010-200-1143 Voter ID # : 10 Mohiuddin Ahamad Bhuiyan Saifuddin Ahmed Bhuiyan A Plus Industries Ltd. -

Provisional Voter List for CGB Election (2015-2016)
Provisional Voter List for CGB Election (2015-2016) Life Member Sl Batch# Cadet# Full Name 1 01 73 OFn. M Waliullah 2 01 79 OFn. Abul Hashem 3 01 80 OFn. Mohammed Ruhul Matin 4 01 81 OFn. Fazlul Haq 5 01 85 OFn. Anwar Masood 6 01 98 OFn. Harunur Rashid 7 02 134 OFn. Khaled Amirul Karim 8 02 140 OFn. Md. Delwar Hossain 9 02 144 OFn. Quamruzzaman Mahmood 10 02 146 OFn. Akhter Imam 11 02 148 OFn. Zaglur Rahman Khan 12 02 155 OFn. Brig. Gen. (Retd) Zahed Latif 13 02 156 OFn. Syed Shahabudin Ahmed 14 03 198 OFn. Tamjid H Basunia 15 03 207 OFn. Abdul Malek 16 03 209 OFn. Mohammad Mujib Ul Huq 17 03 210 OFn. K Nasiruddin Ahmed 18 03 213 OFn. Muazzem Hossain Khan 19 03 214 OFn. Mohammad Saifuddin 20 03 219 OFn. Fazlur Rahman 21 03 220 OFn. Comdr. Abu Zaher Nizam 22 04 131 OFn. Chowdhury Fakhruzzaman 23 04 14 OFn. Mirza Emdadul Huq 24 04 269 OFn. Quazi Kamaluddin 25 04 272 OFn. C M Mohsin 26 04 274 OFn. Md. Shariatullah 27 04 280 OFn. Nasiruddin Ahmad 28 04 285 Ofn. Maj Gen Amsa Amin 29 04 29 OFn. Syed Rashid Ali Kazmi 30 04 32 OFn. M. Kamal Hayat 31 04 36 OFn. Mostafa Kamal Uddin Page 1 of 34 Provisional Voter List for CGB Election (2015-2016) Life Member Sl Batch# Cadet# Full Name 32 04 37 OFn. Abdullah Mohibuddin 33 04 38 OFn. Hayat Hussain 34 04 55 OFn. Obaidur Rahman Khan 35 04 57 OFn. -

Appellate Jurisdiction
Appellate Jurisdiction Daily Supplementary List Of Cases For Hearing On Wednesday, 28th of July, 2021 CONTENT SL COURT PAGE BENCHES TIME NO. ROOM NO. NO. HON'BLE JUSTICE RAJESH BINDAL , CHIEF JUSTICE (ACTING) 1 HON'BLE JUSTICE I. P. MUKERJI On 28-07-2021 1 (Larger 1 HON'BLE JUSTICE HARISH TANDON At 11:00 AM Bench) HON'BLE JUSTICE SOUMEN SEN HON'BLE JUSTICE SUBRATA TALUKDAR HON'BLE JUSTICE RAJESH BINDAL , CHIEF 1 On 28-07-2021 2 JUSTICE (ACTING) 3 DB-I At 11:00 AM HON'BLE JUSTICE RAJARSHI BHARADWAJ HON'BLE JUSTICE I. P. MUKERJI 3 On 28-07-2021 3 5 HON'BLE JUSTICE ARINDAM MUKHERJEE DB-II HON'BLE JUSTICE HARISH TANDON 28 On 28-07-2021 4 9 HON'BLE JUSTICE BIBEK CHAUDHURI DB-III At 11:00 AM HON'BLE JUSTICE SOUMEN SEN 16 2 -07-2021 5 For 9 65 HON'BLE JUSTICE SUBHASIS DASGUPTA DB - V At 12:55 PM HON'BLE JUSTICE SOUMEN SEN 16 On 28-07-2021 6 66 HON'BLE JUSTICE HIRANMAY BHATTACHARYYA DB - V At 11:00 AM HON'BLE JUSTICE SUBRATA TALUKDAR 11 On 28-07-2021 7 74 HON'BLE JUSTICE JAY SENGUPTA DB-VI At 11:00 AM HON'BLE JUSTICE TAPABRATA CHAKRABORTY 30 On 28-07-2021 8 81 HON'BLE JUSTICE SUBHASIS DASGUPTA DB-VII At 11:00 AM HON'BLE JUSTICE ARINDAM SINHA 4 On 28-07-2021 9 87 HON'BLE JUSTICE SAUGATA BHATTACHARYYA DB - VIII At 11:00 AM HON'BLE JUSTICE ARIJIT BANERJEE 32 On 28-07-2021 10 98 HON'BLE JUSTICE SUVRA GHOSH DB - IX At 11:00 AM 8 On 28-07-2021 11 HON'BLE JUSTICE DEBANGSU BASAK 126 SB II At 11:00 AM 42 On 28-07-2021 12 HON'BLE JUSTICE SHIVAKANT PRASAD 150 SB - III At 11:00 AM 13 On 28-07-2021 13 HON'BLE JUSTICE RAJASEKHAR MANTHA 154 SB - IV At 11:00 AM HON'BLE JUSTICE SABYASACHI 7 On 28-07-2021 14 184 BHATTACHARYYA SB - V At 11:00 AM 26 On 28-07-2021 15 HON'BLE JUSTICE SHEKHAR B. -
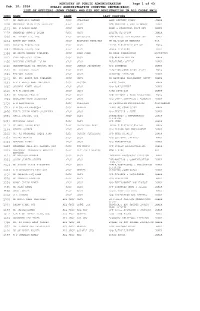
Who Did Not Registra
MINISTRY OF PUBLIC ADMINISTRATION Page 1 of 43 Feb. 10, 2016 PUBLIC ADMINISTRATION COMPUTER CENTRE(PACC) LIST OF OFFICERS (ADMN CADRE) WHO DID NOT REGISTRATION IN ALL CADRE PMIS IDNO NAME RANK LAST POSTING 1041 MD MAHFUZUR RAHMAN SECY CHAIRMAN LAND REFORMS BOARD DHAKA 1096 MOHAMMAD MOINUDDIN ABDULLAH SECY SECY M/O HOUSING & PUBLIC WORKS DHAKA 1171 DR. M ASLAM ALAM SECY SECY BANK & FINANCIAL INST DIV DHAKA 1229 KHANDKER ANWRUL ISLAM SECY SECY BRIDGE DIVISION DHAKA 1230 MD EBADOT ALI, NDC SECY OSD(SECY) M/O PUBLIC ADMINISTRATION DHAKA 1264 BARUN DEV MITRA SECY ECONOMIC MINISTER UN MISSION IN NEWYORK USA 1355 SURAIYA BEGUM, NDC SECY SECY PRIME MINISTER`S OFFICE DHAKA 1381 MONOWAR ISLAM, NDC SECY SECY POWER DIVISION DHAKA 1394 MD ABDUL MANNAN HOWLADER SECY HIGH COMM BD HIGH COMMISSION MAURITIUS 1431 SYED MONJURUL ISLAM SECY SECY M/O HEALTH AND FW DHAKA 1456 BHUIYAN SHAFIQUL ISLAM SECY SECY PRESIDENTS OFFICE DHAKA 1520 HEDAYETULLAH AL MAMOON, NDC SECY SENIOR SECRETARY M/O COMMERCE DHAKA 1521 MD. SIRAZUL ISLAM SECY SECY ELECTION COMMISSION SECTT DHAKA 1569 TARIQUL ISLAM SECY SECY PLANNING DIVISION DHAKA 1571 DR. MD. ABDUR ROB HOWLADER SECY SECY BD NATIONAL PARLIAMENT SECTT DHAKA 1603 A K M ABDUL AWAL MAZUMDER SECY RECTOR BPATC SAVAR DHAKA 1605 SHYAMAL KANTI GHOSH SECY SECY M/O AGRICULTURE DHAKA 1610 M A N SIDDIQUE SECY SECY ROAD DIVISION DHAKA 1653 MD HUMAYUN KHALID SECY SECY M/O PRIMARY & MASS EDUCATION DHAKA 1709 KHURSHED ALAM CHOWDHURY SECY SECY M/O CIVIL AVIATION & TOURISM DHAKA 1710 A M BADRUDDUJA SECY CHAIRMAN BD PETROLIUM CORPORATION CHITTAGONG 1733 S M GHULAM FAROOQUE SECY MEMBER PLANNING COMMISSION DHAKA 1876 FARID UDDIN AHMED CHOWDHURY SECY SECY M/O TEXTILE & JUTE DHAKA 1986 KANIZ FATEMA, NDC SECY SECY STATISTICS & INFORMATICS DHAKA DIVISION 2007 MUSHFEKA IKFAT SECY SECY M/O FOOD DHAKA 2113 MD ABUL KALAM AZAD SECY PRINCIPAL SECY PRIME MINISTER`S OFFICE DHAKA 2148 MIKAIL SHIPAR SECY SECY M/O LABOUR AND EMPLOYMENT DHAKA 2232 DR.