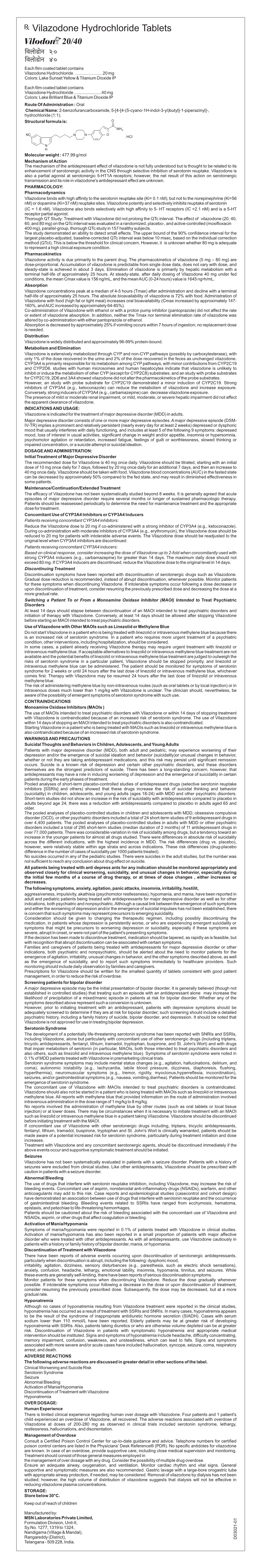
D03021-01 Vilazodone Leaflet.Cdr
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Vortioxetine (Trintellix) Or Vilazodone (Viibryd)
Clinical Policy: Polyserotonergic Antidepressants- Vortioxetine (Trintellix) or Vilazodone (Viibryd) Reference Number: AZ.CP.PMN.20 Effective Date: 06.17 Last Review Date: 07.20 Line of Business: Arizona Medicaid Revision Log See Important Reminder at the end of this policy for important regulatory and legal information. Description Vortioxetine (Trintellix®) and Vilazodone (Viibryd®) are antidepressants that enhance serotoninergic activity via multiple mechanisms FDA approved indications Trintellix and Viibryd are indicated for the treatment of major depressive disorder. Policy/Criteria Provider must submit documentation (such as office chart notes, lab results or other clinical information) supporting that member has met all approval criteria. It is the policy of Arizona Complete Health Trintellix and Viibryd are medically necessary when the following criteria are met: I. Initial Approval Criteria A. Depression (must meet all): 1. Diagnosis of major depressive disorder (MDD); 2. For Trintellix- age ≥ 18 years and for Viibryd- age ≥ 12 years; 3. Failure of a ≥ 8 week trial of one SSRI at up to maximally indicated doses unless contraindicated or clinically significant adverse effects are experienced; 4. Failure of a ≥ 8 week trial of one SNRI at up to maximally indicated doses unless contraindicated or clinically significant adverse effects are experienced; 5. Failure of one SSRI or SNRI used adjunctively with one of the following: bupropion, mirtazapine, or tricyclic antidepressant (TCA) unless contraindicated 6. Dose of Trintellix does not exceed 20 mg/day (1 tablet/day) or dose of Viibryd does not exceed 40 mg/day (1 tablet/day). Approval duration: 12 months B. Other diagnoses/indications 1. Refer to the off-label use policy for the relevant line of business if diagnosis is NOT specifically listed under section III (Diagnoses/Indications for which coverage is NOT authorized): AZ.CP.PMN.53 for Arizona Medicaid. -

(Viibryd©) Vilazodone
3/28/2013 ANTIDEPRESSANT UPDATE: What’s New? The Cardiac Debate The Efficacy Debate ?Pharmacogenomics? WHAT’S NEW Rex S. Lott, Pharm.D., BCPP Professor, ISU College of Pharmacy Short Answer???? Mental Health Clinical Pharmacist, Boise VAMC Clinical Associate Professor, University of Washington, School of Medicine, Department of Psychiatry & Behavioral Sciences Vilazodone (Viibryd ©) Vilazodone - Dosing • Initiate at 10 mg/day X 7days, then 20 • SSRI with partial agonist activity at 5HT 1A mg/day X 7 days receptors. • Target dose = 40 mg/day • Pharmacology of buspirone “built in” • Reduce dose by 50% if co-medication with • CYP3A4 Substrate potent CYP3A4 inhibitors (ketoconazole, • No clinically significant CYP inhibition some macrolide antibiotics) • QD dosing – 25 hour half-life 1 3/28/2013 Ketamine Vilazodone – Pluses / Minuses • NMDA Receptor Antagonist • Potential Pluses: – Less sexual dysfunction than other SSRI’s? • THEORY: – Enhanced anti-anxiety activity (NOT FDA – NMDA Antagonism ↑ Glutamate release labeled for anxiety)? (?compensatory?) • Potential Minuses: Still an SSRI – Stimulation of AMPA glutamate receptors, AND – Repair / regeneration of glutamate-related – GI side effects circuits. – Sleep disturbance – Cost Ketamine Ketamine – Relevant PK • T = ~ 2.5 hours • IV Sub-anesthetic doses 1/2 – 0.5 mg/kg IV infused over ~40 min • Distribution T 1/2 = ~ 10 min – One study of repeated doses (6) • Hepatic Metabolism: CYP 450 • RAPID (hours) remission of depression – 2B6, 3A4 symptoms in treatment-resistant patients – 2C9 (minor) -

NDA/BLA Multi-Disciplinary Review and Evaluation NDA 022567/S021 Viibryd (Vilazodone Hydrochloride)
NDA/BLA Multi-disciplinary Review and Evaluation NDA 022567/s021 Viibryd (vilazodone hydrochloride) NDA/BLA Multi-Disciplinary Review and Evaluation Application Type Efficacy Supplement Application Number(s) NDA 22567/s021 Priority or Standard Priority Submit Date(s) 08/01/2019 Received Date(s) 08/01/2019 PDUFA Goal Date 02/01/2020 Division/Office Division of Psychiatry (DP)/Office of Neuroscience Review Completion Date 1/31/2020 Established/Proper Name Vilazodone hydrochloride (Proposed) Trade Name Viibryd Pharmacologic Class Selective Serotonin Reuptake Inhibitor Code name N/A Applicant Allergan Sales, LLC Dosage form 10 mg, 20 mg, and 40 mg tablets Applicant proposed Dosing 20 mg to 40 mg once daily with food Regimen Applicant Proposed Major Depressive Disorder (MDD) Indication(s)/Population(s) Applicant Proposed 370143000 SNOMED CT Indication Disease Term for each Proposed Indication Recommendation on Approval Regulatory Action Recommended Major Depressive Disorder (MDD) in adults Indication(s)/Population(s) (if applicable) Recommended SNOMED 370143000 CT Indication Disease Term for each Indication (if applicable) Recommended Dosing 20 mg to 40 mg once daily with food Regimen 1 Version date: July 7, 2019 Reference ID: 4555170 NDA/BLA Multi-disciplinary Review and Evaluation NDA 022567/s021 Viibryd (vilazodone hydrochloride) Table of Contents Table of Tables ................................................................................................................................ 4 Table of Figures .............................................................................................................................. -
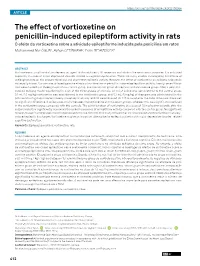
The Effect of Vortioxetine on Penicillin-Induced Epileptiform
https://doi.org/10.1590/0004-282X20190064 ARTICLE The effect of vortioxetine on penicillin-induced epileptiform activity in rats O efeito da vortioxetina sobre a atividade epileptiforme induzida pela penicilina em ratos Muhammed Nur ÖGÜN1, Ayhan ÇETİNKAYA2, Ersin BEYAZÇİÇEK3 ABSTRACT Vortioxetine is a multimodal antidepressant agent that modulates 5-HT receptors and inhibits the serotonin transporter. It is indicated especially in cases of major depressive disorder related to cognitive dysfunction. There are many studies investigating the effects of antidepressants on the seizure threshold and short-term epileptic activity. However, the effect of vortioxetine on epileptic seizures is not exactly known. Our aim was to investigate the effects of vortioxetine on penicillin-induced epileptiform activity. Twenty-seven Wistar rats were divided into three groups: sham-control group, positive control group (diazepam), and vortioxetine group. After a penicillin- induced epilepsy model was formed in each of the three groups of animals, 0.1 ml of saline was administered to the control group, 0.1 ml (10 mg/kg) vortioxetine was administered in the vortioxetine group, and 0.1 mL (5 mg/kg) of diazepam was administered in the positive control group, intraperitoneally. The epileptic activity records were obtained for 120 minutes after the onset of seizure. There was no significant difference in spike wave activity between the vortioxetine and diazepam groups, whereas this was significantly reduced in the vortioxetine group compared with the controls. The administration of vortioxetine at a dose of 10 mg/kg immediately after the seizure induction significantly decreased the spike frequencies of epileptiform activity compared with the control group. -
Prescriber's Guide to Using 3 New Antidepressants W
VILAZODONE • LEVOMILNACIPRAN • VORTIOXETINE Prescriber’s guide to using 3 new antidepressants How do they work? What makes them different? And which patients might benefit most from taking them? Ahmed Z. Elmaadawi, MD Narendra Singh, MD ith a prevalence >17%, depression is one of the most common Jagadeesh Reddy, MD, MPH mental disorders in the United States and the second leading Adjunct Clinical Assistant Professors W 1,2 cause of disability worldwide. For decades, primary care and mental Suhayl Joseph Nasr, MD health providers have used selective serotonin reuptake inhibitors (SSRIs) Volunteer Clinical Professor as first-line treatment for depression—yet the remission rate after the first Department of Psychiatry trial of an antidepressant is <30%, and continues to decline after a first Indiana University School of Medicine- antidepressant failure.3 South Bend Campus South Bend, Indiana That is why clinicians continue to seek effective treatments for depres- sion—ones that will provide quick and sustainable remission—and why Disclosures Drs. Elmaadawi, Singh, and Reddy report no financial scientists and pharmaceutical manufacturers have been competing to relationships with any company whose products develop more effective antidepressant medications. are mentioned in this article or with manufacturers of competing products. Dr. Nasr is a member of the In the past 4 years, the FDA has approved 3 antidepressants— speakers’ bureau for Forest Pharmaceuticals and Takeda vilazodone, levomilnacipran, and vortioxetine—with the hope of Pharmaceutical Company Limited and H. Lundbeck A/S. increasing options for patients who suffer from major depression. These 3 antidepressants differ in their mechanisms of action from other available antidepressants, and all have been shown to have acceptable safety and tolerability profiles. -
![MEDICATION GUIDE VIIBRYD [Vī-Brid] (Vilazodone Hydrochloride)](https://docslib.b-cdn.net/cover/2602/medication-guide-viibryd-v%C4%AB-brid-vilazodone-hydrochloride-1482602.webp)
MEDICATION GUIDE VIIBRYD [Vī-Brid] (Vilazodone Hydrochloride)
MEDICATION GUIDE VIIBRYD [vī-brid] (vilazodone hydrochloride) Tablets Read this Medication Guide carefully before you start taking VIIBRYD and each time you get a refill. There may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or your treatment. What is the most important information I should know about VIIBRYD? VIIBRYD and other antidepressant medicines may cause serious side effects. Call your healthcare provider right away if you have any of the following symptoms, or call 911 if there is an emergency: 1. Suicidal thoughts or actions: • VIIBRYD and other antidepressant medicines may increase suicidal thoughts or actions in some people 24 years of age and younger, especially within the first few months of treatment or when the dose is changed. • Depression or other serious mental illnesses are the most important causes of suicidal thoughts or actions. • Watch for these changes and call your healthcare provider right away if you notice: • New or sudden changes in mood, behavior, actions, thoughts, or feelings, especially if severe. • Pay particular attention to such changes when VIIBRYD is started or when the dose is changed. • Keep all follow-up visits with your healthcare provider and call between visits if you are worried about symptoms. Call your healthcare provider right away if you have any of the following symptoms, especially if they are new, worse, or worry you: • attempts to commit suicide • acting on dangerous impulses • acting aggressive or violent • thoughts about suicide or dying • new or worse depression • new or worse anxiety or panic attacks • feeling agitated, restless, angry or irritable • trouble sleeping • an increase in activity or talking more than what is normal for you (mania) • other unusual changes in behavior or mood 2. -

Kiyomi Shinohara, Orestis Efthimiou, Edoardo G Ostinelli, Anneka Tomlinson, John R Geddes, Andrew a Nierenberg, Henricus G Ruhe, Toshi A
COMPARATIVE EFFICACY AND ACCEPTABILITY OF ANTIDEPRESSANTS IN THE LONG-TERM TREATMENT OF MAJOR DEPRESSION: PROTOCOL FOR A SYSTEMATIC REVIEW AND NETWORK META-ANALYSIS Kiyomi Shinohara, Orestis Efthimiou, Edoardo G Ostinelli, Anneka Tomlinson, John R Geddes, Andrew A Nierenberg, Henricus G Ruhe, Toshi A. Furukawa, Andrea Cipriani, Supplementary Appendix 1 Appendix 1: Search Strategies A. Ovid MEDLINE(R) and In-Process & Other Non-Indexed Citations 1 depressive disorder/ or depressive disorder, major/ or dysthymic disorder/ or Adjustment Disorders/ or Mood Disorders/ or Affective Symptoms/ 2 (depress* or dysthymi* or adjustment disorder* or mood disorder* or "affective disorder" or "affective symptoms").tw,kw,kf. 3 or/1-2 4 Amitriptyline/ or Bupropion/ or Citalopram/ or CLOMIPRAMINE/ or Desvenlafaxine Succinate/ or Duloxetine Hydrochloride/ or Citalopram/ or FLUOXETINE/ or Fluvoxamine/ or PAROXETINE/ or SERTRALINE/ or TRAZODONE/ or Venlafaxine Hydrochloride/ or Vilazodone Hydrochloride/ 5 (agomelatine or amitriptyline or bupropion or citalopram or clomipramine or desvenlafaxine or duloxetine or escitalopram or fluoxetine or fluvoxamine or levomilnacipran or milnacipran or mirtazapine or nefazodone or paroxetine or reboxetine or sertraline or trazodone or venlafaxine or vilazodone or vortioxetine).tw,kw,kf. 6 or/4-5 7 exp clinical trial/ 8 exp randomized controlled trials/ 9 exp double-blind method/ 10 exp single-blind method/ 11 exp cross-over studies/ 12 randomized controlled trial.pt. 13 clinical trial.pt. 14 controlled clinical trial.pt. 15 (clinic* adj2 trial).mp. 16 (random* adj5 control* adj5 trial*).mp. 17 (crossover or cross-over).mp. 18 ((singl* or double* or trebl* or tripl*) adj (blind* or mask*)).mp. 19 randomi*.mp. 20 (random* adj5 (assign* or allocat* or assort* or reciev*)).mp. -

1 Supplemental Figure 1: Illustration of Time-Varying
Supplemental Material Table of Contents Supplemental Table 1: List of classes and medications. Supplemental Table 2: Association between benzodiazepines and mortality in patients initiating hemodialysis (n=69,368) between 2013‐2014 stratified by age, sex, race, and opioid co‐dispensing. Supplemental Figure 1: Illustration of time‐varying exposure to benzodiazepine or opioid claims for one person. Several sensitivity analyses were performed wherein person‐day exposure was extended to +7 days, +14 days, and +28 days beyond the outlined periods above. 1 Supplemental Table 1: List of classes and medications. Class Medications Short‐acting benzodiazepines Alprazolam, estazolam, lorazepam, midazolam, oxazepam, temazepam, and triazolam Long‐acting benzodiazepines chlordiazepoxide, clobazam, clonazepam, clorazepate, diazepam, flurazepam Opioids alfentanil, buprenorphine, butorphanol, codeine, dihydrocodeine, fentanyl, hydrocodone, hydromorphine, meperidine, methadone, morphine, nalbuphine, nucynta, oxycodone, oxymorphone, pentazocine, propoxyphene, remifentanil, sufentanil, tapentadol, talwin, tramadol, carfentanil, pethidine, and etorphine Antidepressants citalopram, escitalopram, fluoxetine, fluvozamine, paroxetine, sertraline; desvenlafaxine, duloxetine, levomilnacipran, milnacipran, venlafaxine; vilazodone, vortioxetine; nefazodone, trazodone; atomoxetine, reboxetine, teniloxazine, viloxazine; bupropion; amitriptyline, amitriptylinoxide, clomipramine, desipramine, dibenzepin, dimetacrine, dosulepin, doxepin, imipramine, lofepramine, melitracen, -

Providers | Medications for Depression
Medications for Depression Antidepressants alter the concentrations of one or more key neurotransmitters in the brain, namely norepinephrine, serotonin, and dopamine. As depression may be a presenting symptom of a mixed manic episode, it is important to adequately screen patients with depressive symptoms to determine if they are at risk of bipolar disorder. All patients should also be monitored with regards to mental status for depression, suicidal ideation, anxiety, social functioning, mania, panic attacks, or other unusual changes in behavior. All antidepressants carry a black box warning of increased risk of suicidal thinking and behavior in children and adolescents, particularly in the first few months of therapy. MAOIs are contraindicated with all other classes of antidepressants and should not be used in combination. Common side effects often improve within the first two weeks of treatment. A low starting dose might help increase tolerance and adherence. DRUG CATEGORY MEDICATION COMMON SIDE EFFECTS MONITORING PARAMETERS ADDITIONAL COMMENTS Selective Serotonin .Citalopram (IR, Liq)* .GI: effects are common (nausea, xerostomia, diarrhea) .Weight and BMI .Comparable to TCAs in efficacy, but are markedly safer and better tolerated Reuptake Inhibitors .Escitalopram (IR, Liq) .Sexual dysfunction: in both men & women .Signs/symptoms of serotonin syndrome .SSRIs differ from each other with respect to their degree of selectivity for the serotonin (SSRIs) .Fluoxetine (IR, Liq ) .Hematologic: Impaired platelet aggregation/bleeding .Electrolytes, -

Currently Prescribed Psychotropic Medications
CURRENTLY PRESCRIBED PSYCHOTROPIC MEDICATIONS Schizophrenia Depression Anxiety Disorders 1st generation antipsychotics: Tricyclics: Atarax (hydroxyzine) Haldol (haloperidol), *Anafranil (clomipramine) Ativan (lorazepam) Haldol Decanoate Asendin (amoxapine) BuSpar (buspirone) Loxitane (loxapine) Elavil (amitriptyline) *Inderal (propranolol) Mellaril (thioridazine) Norpramin (desipramine) Keppra (levetiracetam) Navane (thiothixene) Pamelor (nortriptyline) *Klonopin (clonazepam) Prolixin (fluphenazine), Prolixin Sinequan (doxepin) Librium (chlordiazepoxide) Decanoate Spravato (esketamine) Serax (oxazepam) Stelazine (trifluoperazine) Surmontil (trimipramine) Thorazine (chlorpromazine) *Tenormin (atenolol) Tofranil (imipramine) MEDICATIONS PSYCHOTROPIC PRESCRIBED CURRENTLY Trilafon (perphenazine) Tranxene (clorazepate) Vivactil (protriptyline) Valium (diazepam) 2nd generation antipsychotics: Zulresso (brexanolone) Vistaril (hydroxyzine) Abilify (aripiprazole) Aristada (aripiprazole) SSRIs: Xanax (alprazolam) Caplyta (lumateperone) Celexa (citalopram) *Antidepressants, especially SSRIs, are also used in the treatment of anxiety. Clozaril (clozapine) Lexapro (escitalopram) Fanapt (iloperidone) *Luvox (fluvoxamine) Geodon (ziprasidone) Paxil (paroxetine) Stimulants (used in the treatment of ADD/ADHD) Invega (paliperidone) Prozac (fluoxetine) Invega Sustenna Zoloft (sertraline) Adderall (amphetamine and Perseris (Risperidone injectable) dextroamphetamine) Latuda (lurasidone) MAOIs: Azstarys(dexmethylphenidate Rexulti (brexpiprazole) Emsam (selegiline) -

Picquestion of the Week:10/22/12
Lake Erie, New York PIC QUESTION OF THE WEEK: 10/22/12 Q: What is the current recommendation for switching from citalopram to Viibryd (vilazodone)? A: Vilazodone (Viibryd), a new oral antidepressant in the same class at nefazodone (Serzone), received FDA-approval in January 2011 for the treatment of major depressive disorder (MDD) in adults. Vilazodone inhibits reuptake of serotonin with partial 5-HT1A receptor agonist activity; however, its antidepressant effect is attributed to its SSRI properties. Like nefazodone, vilazodone is metabolized by CYP 3A4 into an active metabolite known as meta-chlorophenylpiperazine (mCPP). This metabolite has a high affinity for a number of serotonin receptors, including 5-HT2C where it functions mostly as an agonist throughout the CNS. Stimulation of 5-HT2C under normal circumstances will initially produce some degree of anxiety, restlessness, and dysphoria; however, continued use seems to produce a paradoxical effect and have resultant antianxiety effects. SSRIs including citalopram typically have an antagonist effect at 5-HT2C resulting in receptor up-regulation; therefore, discontinuation of a SSRI and addition of Viibryd, results in both loss of 5- HT2C antagonism and additive agonist effects. The effect is profound dysphoria and anxiety. These effects will taper off with continued use, but a careful titration schedule needs to be in place to mediate the effects at the initiation of vilazodone therapy. Currently, no recommendations are available on switching from an SSRI to vilazodone, so nefazodone recommendations are concluded to provide the most probable recommendations for vilazodone. It is recommended to taper off the citalopram over 2-4 weeks depending on the current dose and complete a seven day washout period (based on a half-life of 35 hours). -

Clinical Utility of Vilazodone for the Treatment of Adults with Major Depressive Disorder and Theoretical Implications for Future Clinical Use
Neuropsychiatric Disease and Treatment Dovepress open access to scientific and medical research Open Access Full Text Article REVIEW Clinical utility of vilazodone for the treatment of adults with major depressive disorder and theoretical implications for future clinical use Mandeep Singh Background: Vilazodone is the latest approved antidepressant available in the United States. Thomas L Schwartz Its dual mechanism of action combines the inhibition of serotonin transporters while simultane- ously partially agonizing serotonin-1a (5-HT1A) receptors. This combined activity results in SUNY Upstate Medical University, Psychiatry Department, Syracuse, serotonin facilitation across the brain’s serotonergic pathways, which has been termed by the NY, USA authors as that of a serotonin partial agonist and reuptake inhibitor, or SPARI. Objective: The authors to review laboratory, animal model data, and human trial data to synthesize a working theory regarding the mechanism of antidepressant action of this agent and regarding its potential for additional indications. Methods: A MEDLINE and Internet search was conducted and the resultant evidence reviewed. Results: Vilazodone has randomized, controlled empirical data which has garnered it an approval for treating major depressive disorder. It combines two well-known pharmacodynamic mechanisms of serotonergic action into a novel agent. Although no head-to-head studies against other antidepressants are published, the efficacy data for vilazodone appears comparable to other known antidepressants, with associated gastrointestinal side effects similar to serotonin selective reuptake inhibitor and serotonin norepinephrine reuptake inhibitor antidepressants, but potentially with a lower incidence of sexual side effects and weight gain. Discussion: As a new option for the treatment of major depressive disorder, vilazodone, due to its unique SPARI mechanism of action, may hold promise for patients who cannot tolerate or have not responded to previous antidepressant monotherapies.