Ars Medica Volume 9, Number 1, Fall 2012
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Songs by Artist
Reil Entertainment Songs by Artist Karaoke by Artist Title Title &, Caitlin Will 12 Gauge Address In The Stars Dunkie Butt 10 Cc 12 Stones Donna We Are One Dreadlock Holiday 19 Somethin' Im Mandy Fly Me Mark Wills I'm Not In Love 1910 Fruitgum Co Rubber Bullets 1, 2, 3 Redlight Things We Do For Love Simon Says Wall Street Shuffle 1910 Fruitgum Co. 10 Years 1,2,3 Redlight Through The Iris Simon Says Wasteland 1975 10, 000 Maniacs Chocolate These Are The Days City 10,000 Maniacs Love Me Because Of The Night Sex... Because The Night Sex.... More Than This Sound These Are The Days The Sound Trouble Me UGH! 10,000 Maniacs Wvocal 1975, The Because The Night Chocolate 100 Proof Aged In Soul Sex Somebody's Been Sleeping The City 10Cc 1Barenaked Ladies Dreadlock Holiday Be My Yoko Ono I'm Not In Love Brian Wilson (2000 Version) We Do For Love Call And Answer 11) Enid OS Get In Line (Duet Version) 112 Get In Line (Solo Version) Come See Me It's All Been Done Cupid Jane Dance With Me Never Is Enough It's Over Now Old Apartment, The Only You One Week Peaches & Cream Shoe Box Peaches And Cream Straw Hat U Already Know What A Good Boy Song List Generator® Printed 11/21/2017 Page 1 of 486 Licensed to Greg Reil Reil Entertainment Songs by Artist Karaoke by Artist Title Title 1Barenaked Ladies 20 Fingers When I Fall Short Dick Man 1Beatles, The 2AM Club Come Together Not Your Boyfriend Day Tripper 2Pac Good Day Sunshine California Love (Original Version) Help! 3 Degrees I Saw Her Standing There When Will I See You Again Love Me Do Woman In Love Nowhere Man 3 Dog Night P.S. -

Songs by Title Karaoke Night with the Patman
Songs By Title Karaoke Night with the Patman Title Versions Title Versions 10 Years 3 Libras Wasteland SC Perfect Circle SI 10,000 Maniacs 3 Of Hearts Because The Night SC Love Is Enough SC Candy Everybody Wants DK 30 Seconds To Mars More Than This SC Kill SC These Are The Days SC 311 Trouble Me SC All Mixed Up SC 100 Proof Aged In Soul Don't Tread On Me SC Somebody's Been Sleeping SC Down SC 10CC Love Song SC I'm Not In Love DK You Wouldn't Believe SC Things We Do For Love SC 38 Special 112 Back Where You Belong SI Come See Me SC Caught Up In You SC Dance With Me SC Hold On Loosely AH It's Over Now SC If I'd Been The One SC Only You SC Rockin' Onto The Night SC Peaches And Cream SC Second Chance SC U Already Know SC Teacher, Teacher SC 12 Gauge Wild Eyed Southern Boys SC Dunkie Butt SC 3LW 1910 Fruitgum Co. No More (Baby I'm A Do Right) SC 1, 2, 3 Redlight SC 3T Simon Says DK Anything SC 1975 Tease Me SC The Sound SI 4 Non Blondes 2 Live Crew What's Up DK Doo Wah Diddy SC 4 P.M. Me So Horny SC Lay Down Your Love SC We Want Some Pussy SC Sukiyaki DK 2 Pac 4 Runner California Love (Original Version) SC Ripples SC Changes SC That Was Him SC Thugz Mansion SC 42nd Street 20 Fingers 42nd Street Song SC Short Dick Man SC We're In The Money SC 3 Doors Down 5 Seconds Of Summer Away From The Sun SC Amnesia SI Be Like That SC She Looks So Perfect SI Behind Those Eyes SC 5 Stairsteps Duck & Run SC Ooh Child SC Here By Me CB 50 Cent Here Without You CB Disco Inferno SC Kryptonite SC If I Can't SC Let Me Go SC In Da Club HT Live For Today SC P.I.M.P. -

Spring Records Discography 4700 Series
Spring Records Discography 4700 series SPR 4701 - The Sounds Of Simon - JOE SIMON [1971] To Lay Down Beside You/I Can’t See Nobody/Most Of All/No More Me/Your Time To Cry//Help Me Make It Through The Night/My Woman, My Woman, My Wife/I Love You More (Than Anything)/Georgia Blue/All My Hard Times 5700 series SPR 5702 - Drowning In The Sea Of Love - JOE SIMON [1972] Drowning In The Sea Of Love/Glad To Be Your Lover/Something You Can Do Today/I Found My Dad/The Mirror Don’t Lie//Ole Night Owl/You Are Everything/If/Let Me Be The One (The One Who Loves You)/Pool Of Bad Luck SPR 5703 - Millie Jackson - MILLIE JACKSON [1972] If This Is Love/I Ain’t Giving Up/I Miss You Baby/A Child Of God (It’s Hard To Believe)/Ask Me What You Want//My Man, A Sweet Man/You’re The Joy Of My Life/I Gotta Get Away (From My Own Self)/I Just Can’t Stand It/Strange Things SPR 5704 - The Power Of Joe Simon - JOE SIMON [1973] Drowning In The Sea Of Love/Georgia Blue/Help Me Make It Through The Night/Power Of Love/Step By Step/Talk Don’t Bother Me/To Lay Down Beside You/Trouble In My Home/You Are The One/Your Time To Cry [*] SPR 5705 - Simon Country - JOE SIMON [1973] Do You Know What It’s Like To Be Lonesome?/Five Hundred Miles/Woman Without Love/You Don’t Know Me/To Get To You//Before The Next Teardrop Falls/Someone To Give My Love To/Good Things/Kiss An Angel Good Mornin’ SPR 5706 - It Hurts So Good - MILLIE JACKSON [1973] Breakaway/Close My Eyes/Don’t Send Nobody Else/Good To The Very Last Drop/Help Yourself/Hurts So Good/Hypocrisy/I Cry/Love Doctor/Now That You Got -

Songs by Title
Karaoke Song Book Songs by Title Title Artist Title Artist #1 Nelly 18 And Life Skid Row #1 Crush Garbage 18 'til I Die Adams, Bryan #Dream Lennon, John 18 Yellow Roses Darin, Bobby (doo Wop) That Thing Parody 19 2000 Gorillaz (I Hate) Everything About You Three Days Grace 19 2000 Gorrilaz (I Would Do) Anything For Love Meatloaf 19 Somethin' Mark Wills (If You're Not In It For Love) I'm Outta Here Twain, Shania 19 Somethin' Wills, Mark (I'm Not Your) Steppin' Stone Monkees, The 19 SOMETHING WILLS,MARK (Now & Then) There's A Fool Such As I Presley, Elvis 192000 Gorillaz (Our Love) Don't Throw It All Away Andy Gibb 1969 Stegall, Keith (Sitting On The) Dock Of The Bay Redding, Otis 1979 Smashing Pumpkins (Theme From) The Monkees Monkees, The 1982 Randy Travis (you Drive Me) Crazy Britney Spears 1982 Travis, Randy (Your Love Has Lifted Me) Higher And Higher Coolidge, Rita 1985 BOWLING FOR SOUP 03 Bonnie & Clyde Jay Z & Beyonce 1985 Bowling For Soup 03 Bonnie & Clyde Jay Z & Beyonce Knowles 1985 BOWLING FOR SOUP '03 Bonnie & Clyde Jay Z & Beyonce Knowles 1985 Bowling For Soup 03 Bonnie And Clyde Jay Z & Beyonce 1999 Prince 1 2 3 Estefan, Gloria 1999 Prince & Revolution 1 Thing Amerie 1999 Wilkinsons, The 1, 2, 3, 4, Sumpin' New Coolio 19Th Nervous Breakdown Rolling Stones, The 1,2 STEP CIARA & M. ELLIOTT 2 Become 1 Jewel 10 Days Late Third Eye Blind 2 Become 1 Spice Girls 10 Min Sorry We've Stopped Taking Requests 2 Become 1 Spice Girls, The 10 Min The Karaoke Show Is Over 2 Become One SPICE GIRLS 10 Min Welcome To Karaoke Show 2 Faced Louise 10 Out Of 10 Louchie Lou 2 Find U Jewel 10 Rounds With Jose Cuervo Byrd, Tracy 2 For The Show Trooper 10 Seconds Down Sugar Ray 2 Legit 2 Quit Hammer, M.C. -

Songs by Title
Songs by Title Title Artist Versions Title Artist Versions #1 Crush Garbage SC 1999 Prince PI SC #Selfie Chainsmokers SS 2 Become 1 Spice Girls DK MM SC (Can't Stop) Giving You Up Kylie Minogue SF 2 Hearts Kylie Minogue MR (Don't Take Her) She's All I Tracy Byrd MM 2 Minutes To Midnight Iron Maiden SF Got 2 Stars Camp Rock DI (I Don't Know Why) But I Clarence Frogman Henry MM 2 Step DJ Unk PH Do 2000 Miles Pretenders, The ZO (I'll Never Be) Maria Sandra SF 21 Guns Green Day QH SF Magdalena 21 Questions (Feat. Nate 50 Cent SC (Take Me Home) Country Toots & The Maytals SC Dogg) Roads 21st Century Breakdown Green Day MR SF (This Ain't) No Thinkin' Trace Adkins MM Thing 21st Century Christmas Cliff Richard MR + 1 Martin Solveig SF 21st Century Girl Willow Smith SF '03 Bonnie & Clyde (Feat. Jay-Z SC 22 Lily Allen SF Beyonce) Taylor Swift MR SF ZP 1, 2 Step Ciara BH SC SF SI 23 (Feat. Miley Cyrus, Wiz Mike Will Made-It PH SP Khalifa And Juicy J) 10 Days Late Third Eye Blind SC 24 Hours At A Time Marshall Tucker Band SG 10 Million People Example SF 24 Hours From Tulsa Gene Pitney MM 10 Minutes Until The Utilities UT 24-7 Kevon Edmonds SC Karaoke Starts (5 Min 24K Magic Bruno Mars MR SF Track) 24's Richgirl & Bun B PH 10 Seconds Jazmine Sullivan PH 25 Miles Edwin Starr SC 10,000 Promises Backstreet Boys BS 25 Minutes To Go Johnny Cash SF 100 Percent Cowboy Jason Meadows PH 25 Or 6 To 4 Chicago BS PI SC 100 Years Five For Fighting SC 26 Cents Wilkinsons, The MM SC SF 100% Chance Of Rain Gary Morris SC 26 Miles Four Preps, The SA 100% Pure Love Crystal Waters PI SC 29 Nights Danni Leigh SC 10000 Nights Alphabeat MR SF 29 Palms Robert Plant SC SF 10th Avenue Freeze Out Bruce Springsteen SG 3 Britney Spears CB MR PH 1-2-3 Gloria Estefan BS SC QH SF Len Barry DK 3 AM Matchbox 20 MM SC 1-2-3 Redlight 1910 Fruitgum Co. -

Songs by Artist
73K October 2013 Songs by Artist 73K October 2013 Title Title Title +44 2 Chainz & Chris Brown 3 Doors Down When Your Heart Stops Countdown Let Me Go Beating 2 Evisa Live For Today 10 Years Oh La La La Loser Beautiful 2 Live Crew Road I'm On, The Through The Iris Do Wah Diddy Diddy When I'm Gone Wasteland Me So Horny When You're Young 10,000 Maniacs We Want Some P---Y! 3 Doors Down & Bob Seger Because The Night 2 Pac Landing In London Candy Everybody Wants California Love 3 Of A Kind Like The Weather Changes Baby Cakes More Than This Dear Mama 3 Of Hearts These Are The Days How Do You Want It Arizona Rain Trouble Me Thugz Mansion Love Is Enough 100 Proof Aged In Soul Until The End Of Time 30 Seconds To Mars Somebody's Been Sleeping 2 Pac & Eminem Closer To The Edge 10cc One Day At A Time Kill, The Donna 2 Pac & Eric Williams Kings And Queens Dreadlock Holiday Do For Love 311 I'm Mandy 2 Pac & Notorious Big All Mixed Up I'm Not In Love Runnin' Amber Rubber Bullets 2 Pistols & Ray J Beyond The Gray Sky Things We Do For Love, The You Know Me Creatures (For A While) Wall Street Shuffle 2 Pistols & T Pain & Tay Dizm Don't Tread On Me We Do For Love She Got It Down 112 2 Unlimited First Straw Come See Me No Limits Hey You Cupid 20 Fingers I'll Be Here Awhile Dance With Me Short Dick Man Love Song It's Over Now 21 Demands You Wouldn't Believe Only You Give Me A Minute 38 Special Peaches & Cream 21st Century Girls Back Where You Belong Right Here For You 21St Century Girls Caught Up In You U Already Know 3 Colours Red Hold On Loosely 112 & Ludacris Beautiful Day If I'd Been The One Hot & Wet 3 Days Grace Rockin' Into The Night 12 Gauge Home Second Chance Dunkie Butt Just Like You Teacher, Teacher 12 Stones 3 Doors Down Wild Eyed Southern Boys Crash Away From The Sun 3LW Far Away Be Like That I Do (Wanna Get Close To We Are One Behind Those Eyes You) 1910 Fruitgum Co. -

Songs by Artist
Sound Master Entertianment Songs by Artist smedenver.com Title Title Title .38 Special 2Pac 4 Him Caught Up In You California Love (Original Version) For Future Generations Hold On Loosely Changes 4 Non Blondes If I'd Been The One Dear Mama What's Up Rockin' Onto The Night Thugz Mansion 4 P.M. Second Chance Until The End Of Time Lay Down Your Love Wild Eyed Southern Boys 2Pac & Eminem Sukiyaki 10 Years One Day At A Time 4 Runner Beautiful 2Pac & Notorious B.I.G. Cain's Blood Through The Iris Runnin' Ripples 100 Proof Aged In Soul 3 Doors Down That Was Him (This Is Now) Somebody's Been Sleeping Away From The Sun 4 Seasons 10000 Maniacs Be Like That Rag Doll Because The Night Citizen Soldier 42nd Street Candy Everybody Wants Duck & Run 42nd Street More Than This Here Without You Lullaby Of Broadway These Are Days It's Not My Time We're In The Money Trouble Me Kryptonite 5 Stairsteps 10CC Landing In London Ooh Child Let Me Be Myself I'm Not In Love 50 Cent We Do For Love Let Me Go 21 Questions 112 Loser Disco Inferno Come See Me Road I'm On When I'm Gone In Da Club Dance With Me P.I.M.P. It's Over Now When You're Young 3 Of Hearts Wanksta Only You What Up Gangsta Arizona Rain Peaches & Cream Window Shopper Love Is Enough Right Here For You 50 Cent & Eminem 112 & Ludacris 30 Seconds To Mars Patiently Waiting Kill Hot & Wet 50 Cent & Nate Dogg 112 & Super Cat 311 21 Questions All Mixed Up Na Na Na 50 Cent & Olivia 12 Gauge Amber Beyond The Grey Sky Best Friend Dunkie Butt 5th Dimension 12 Stones Creatures (For A While) Down Aquarius (Let The Sun Shine In) Far Away First Straw AquariusLet The Sun Shine In 1910 Fruitgum Co. -

Manitowoc Kennel Club Friday, April 2, 2021
Manitowoc Kennel Club Friday, April 2, 2021 Group Results Sporting Spaniels (English Cocker) 27 BB/G1 GCHP CH K'mander Dawnglow Arnage. SR89298901 Retrievers (Chesapeake Bay) 25 BB/G2 GCHG CH Sandbar's Hardcore Hank MH. SR81693507 Setters (English) 26 BB/G3 GCH CH Ciara N' Honeygait Belle Of The Ball. SS07012602 Retrievers (Golden) 37 BB/G4 GCHG CH Futura Lime Me Entertain You CGC. SR86361206 Hound Whippets 18 1/W/BB/BW/G1 Woods Runner One And Only. HP56111307 Beagles (15 Inch) 11 BB/G2 GCHB CH Everwind's Living The Dream. HP55226602 Rhodesian Ridgebacks 32 BB/G3 GCHS CH Hilltop's Enchanting Circe of Dykumos. HP57068004 Afghan Hounds 7 BB/G4 GCHG CH Taji Better Man Mazshalna CGC. HP45099607 Working Great Danes 26 BB/G1 GCHG CH Landmark-Divine Acres Kiss Myself I'm So Pretty. WS56877803 Samoyeds 34 BB/G2 GCHG CH Sammantic Speed Of Life. WS59323801 Bernese Mountain Dogs 33 BB/G3 GCH CH Bernergardens Look To The Stars BN RI. WS62005402 Doberman Pinschers 46 BB/G4 GCHB CH Kandu's Glamour Puss V Mytoys. WS61064602 Terrier Australian Terriers 15 BB/G1 GCHS CH Temora Steal My Heart CA TKN. RN29651902 Border Terriers 12 BB/G2 GCHS CH Meadowlake High Times. RN31451901 American Staffordshire Terriers 19 BB/G3 CH Corralitos Tracking The Storm. RN33989402 Glen of Imaal Terriers 23 BB/G4 GCH CH Abberann Midnight Rider Of Glendalough. RN31978502 Toy Affenpinschers 7 BB/G1/BIS GCHS CH Point Dexter V. Tani Kazari. TS40341801 Papillons 17 BB/G2 GCHG CH Wingssong This Could Be Love. TS32017001 Maltese 7 BB/G3 GCHS CH Martin's Time Bomb Puff. -

Songs by Artist
Songs by Artist Title Title (Hed) Planet Earth 2 Live Crew Bartender We Want Some Pussy Blackout 2 Pistols Other Side She Got It +44 You Know Me When Your Heart Stops Beating 20 Fingers 10 Years Short Dick Man Beautiful 21 Demands Through The Iris Give Me A Minute Wasteland 3 Doors Down 10,000 Maniacs Away From The Sun Because The Night Be Like That Candy Everybody Wants Behind Those Eyes More Than This Better Life, The These Are The Days Citizen Soldier Trouble Me Duck & Run 100 Proof Aged In Soul Every Time You Go Somebody's Been Sleeping Here By Me 10CC Here Without You I'm Not In Love It's Not My Time Things We Do For Love, The Kryptonite 112 Landing In London Come See Me Let Me Be Myself Cupid Let Me Go Dance With Me Live For Today Hot & Wet Loser It's Over Now Road I'm On, The Na Na Na So I Need You Peaches & Cream Train Right Here For You When I'm Gone U Already Know When You're Young 12 Gauge 3 Of Hearts Dunkie Butt Arizona Rain 12 Stones Love Is Enough Far Away 30 Seconds To Mars Way I Fell, The Closer To The Edge We Are One Kill, The 1910 Fruitgum Co. Kings And Queens 1, 2, 3 Red Light This Is War Simon Says Up In The Air (Explicit) 2 Chainz Yesterday Birthday Song (Explicit) 311 I'm Different (Explicit) All Mixed Up Spend It Amber 2 Live Crew Beyond The Grey Sky Doo Wah Diddy Creatures (For A While) Me So Horny Don't Tread On Me Song List Generator® Printed 5/12/2021 Page 1 of 334 Licensed to Chris Avis Songs by Artist Title Title 311 4Him First Straw Sacred Hideaway Hey You Where There Is Faith I'll Be Here Awhile Who You Are Love Song 5 Stairsteps, The You Wouldn't Believe O-O-H Child 38 Special 50 Cent Back Where You Belong 21 Questions Caught Up In You Baby By Me Hold On Loosely Best Friend If I'd Been The One Candy Shop Rockin' Into The Night Disco Inferno Second Chance Hustler's Ambition Teacher, Teacher If I Can't Wild-Eyed Southern Boys In Da Club 3LW Just A Lil' Bit I Do (Wanna Get Close To You) Outlaw No More (Baby I'ma Do Right) Outta Control Playas Gon' Play Outta Control (Remix Version) 3OH!3 P.I.M.P. -

2 Records Aug 15 2021
Sept 2, 2021 Latest additions indicated by asterisk (*) C * ? & THE MYSTERIANS 99 TEARS / MIDNIGHT HOUR 10 CC I'M NOT IN LOVE/CHANNEL SWIMMER 1910 FRUITGUM CO, SIMON SAYS REFLECTIONS FROM THE LOOKING GLASS 1910 FRUITGUM CO. SIMON SAYS/REFLECTIONS FROM THE LOOKING GLASS 2 R 1910 FRUITGUM CO. INDIAN GIVER / POW WOW 3 SHARPES QUARTET LES MY LOVE WAS NOT TRUE LOVE/BELLE ST. JOHN R 49TH PARALLEL NOW THAT I'M A MAN / TALK TO ME R 6 CYLINDER AIN'T NOBODY HERE BUT US CHICKENS / STRONG WOMAN.... 6 CYLINDER AIN'T NOBODY HERE BUT US CHICKENS / STRONG WOMAN'S LOVE 8TH DAY IF I COULD SEE THE LIGHT / IF I COULD SEE THE LIGHT (INST) 9 LAFALCE BROTHERS MARIA, MARIA, MARIA/THE DEVIL'S HIGHWAY A TASTE OF HONEY SUKAYAKI / DON'T YOU LEAD ME ON A*TEENS DANCING QUEEN / MAMMA MIA A*TEENS DANCING QUEEN / MAMMA MIA AARON LEE ONLY HUMAN / EMPTY HEART A * ABBA KNOWING ME KNOWING YOU / HAPPY HAWAII A * ABBA MONEY MONEY MONEY / CRAZY WORLD ABBOTT GREGORY SHAKE YOU DOWN / WAIT UNTIL TOMORROW ABBOTT RUSS SPACE INVADERS MEET PURPLE PEOPLE EATER/COUNTRY COOPERMAN ABC ALL OF MY HEART / OVERTURE ABC ALL OF MY HEART / OVERTURE ABC THAT WAS THEN BUT THIS IS NOW / VERTIGO ABC THE LOOK OF LOVE / THE LOOK OF LOVE ABDUL PAULA MY LOVE IS FOR REAL / SAY I LOVE YOU ABDUL PAULA I DIDN'T SAY I LOVE YOU/MY LOVE IS FOR REAL ABDUL PAULA IT'S JUST THE WAY YOU LOVE ME/DUB MIX . PICTURE SLEEVE ABDUL PAULA THE PROMISE OF A NEW DAY/THE PROMISE OF A NEW DAY ABDUL PAULA VIBEOLOGY/VIBEOLOGY ABRAMS MISS MILL VALLEY/THE HAPPIEST DAY OF MY LIFE ABRAMSON RONNEY NEVER SEEM TO GET ALONG WITHOUT YOU/TIME -
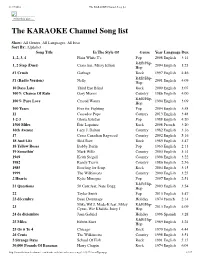
The KARAOKE Channel Song List
11/17/2016 The KARAOKE Channel Song list Print this List ... The KARAOKE Channel Song list Show: All Genres, All Languages, All Eras Sort By: Alphabet Song Title In The Style Of Genre Year Language Dur. 1, 2, 3, 4 Plain White T's Pop 2008 English 3:14 R&B/Hip- 1, 2 Step (Duet) Ciara feat. Missy Elliott 2004 English 3:23 Hop #1 Crush Garbage Rock 1997 English 4:46 R&B/Hip- #1 (Radio Version) Nelly 2001 English 4:09 Hop 10 Days Late Third Eye Blind Rock 2000 English 3:07 100% Chance Of Rain Gary Morris Country 1986 English 4:00 R&B/Hip- 100% Pure Love Crystal Waters 1994 English 3:09 Hop 100 Years Five for Fighting Pop 2004 English 3:58 11 Cassadee Pope Country 2013 English 3:48 1-2-3 Gloria Estefan Pop 1988 English 4:20 1500 Miles Éric Lapointe Rock 2008 French 3:20 16th Avenue Lacy J. Dalton Country 1982 English 3:16 17 Cross Canadian Ragweed Country 2002 English 5:16 18 And Life Skid Row Rock 1989 English 3:47 18 Yellow Roses Bobby Darin Pop 1963 English 2:13 19 Somethin' Mark Wills Country 2003 English 3:14 1969 Keith Stegall Country 1996 English 3:22 1982 Randy Travis Country 1986 English 2:56 1985 Bowling for Soup Rock 2004 English 3:15 1999 The Wilkinsons Country 2000 English 3:25 2 Hearts Kylie Minogue Pop 2007 English 2:51 R&B/Hip- 21 Questions 50 Cent feat. Nate Dogg 2003 English 3:54 Hop 22 Taylor Swift Pop 2013 English 3:47 23 décembre Beau Dommage Holiday 1974 French 2:14 Mike WiLL Made-It feat. -

Songs by Title
Sound Master Entertianment Songs by Title smedenver.com Title Artist Title Artist #1 Nelly Spice Girls #1 Crush Garbage 2 In The Morning New Kids On The (Cable Car) Over My Head Fray Block (I Love You) What Can I Say Jerry Reed 2 Step Unk (I Wanna Hear) A Cheatin' Song Anita Cochran & 20 Good Reasons Thirsty Merc Conway Twitty 21 Questions 50 Cent (If You're Wondering If I Want Weezer 50 Cent & Nate Dogg You To) I Want You To 24 7 Kevon Edmonds (It's Been You) Right Down The Gerry Rafferty 24 Hours From Tulsa Gene Pitney Line 24's T.I. (I've Had) The Time Of My Life Bill Medley & Jennifer 25 Miles Edwin Starr Warnes 25 Or 6 To 4 Chicago (Just Like) Romeo & Juliet Reflections 26 Cents Wilkinsons (My Friends Are Gonna Be) Merle Haggard 29 Nights Danni Leigh Strangers 29 Palms Robert Plant (Reach Up For The) Sunrise Duran Duran 3 Britney Spears (Sittin' On) The Dock Of The Bay Michael Bolton 30 Days In The Hole Humble Pie Otis Redding 30,000 Pounds Of Bananas Harry Chapin (There's Gotta Be) More To Life Stacie Orrico 32 Flavors Alana Davis (When You Feel Like You're In Carl Smith Love) Don't Just Stand There 3am Matchbox Twenty (Who Discovered) America Ozomatli 4 + 20 Crosby, Stills, Nash & Young (You Never Can Tell) C'est La Emmylou Harris Vie 4 Ever Lil Mo & Fabolous (You Want To) Make A Memory Bon Jovi 4 In The Morning Gwen Stefani '03 Bonnie & Clyde Jay-Z & Beyonce 4 Minutes Avant 1, 2 Step Ciara & Missy Elliott 4 To 1 In Atlanta Tracy Byrd 1, 2, 3, 4 (I Love You) Plain White T's 409 Beach Boys 1,000 Faces Randy Montana 42nd Street 42nd Street 10 Days Late Third Eye Blind 45 Shinedown 100 Years Five For Fighting 455 Rocket Kathy Mattea 100% Chance Of Rain Gary Morris 4am Our Lady Peace 100% Pure Love Crystal Waters 5 Miles To Empty Brownstone 10th Ave.