6. Refractive Errors .Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sightsavers Policy on Recycled Spectacles
DRAFT POSITION PAPER ADJUSTABLE SPECTACLES Position statement There are an estimated 670 million cases of blindness or vision impairment (153 million people with impaired far visioni and 517 million people with impaired near visionii) simply because they are unable to access an appropriate eye examination and spectacles. Far vision impairment alone costs $269billion a year in lost productivity.iii The massive volume of cases, and consequent scale of disability and economic impact caused by uncorrected refractive error (URE) has lead to various attempts to provide short-cut refractive care. Adjustable spectacles, with the optical power either set in an eye examination or self-adjusted, have been promoted by several companies and organizations as a potential solution.iv IAPB recognises the good intentions behind these short-cuts and spectacle technology but advises that its members and other parties engaged in promoting eye health should exercise caution with or avoid adjustable spectacles at this time. In deciding whether and how to use adjustable spectacles in future, the following areas should be considered. Considerations Sustainability It is critical that refractive services are provided in a manner that contributes to affordable, high quality eye care for all patients irrespective of social standing. Isolated provision of spectacles is detrimental to the human resources and service delivery systems that are necessary for sustainable eye care services, and so should be avoided whenever possible. • Adjustable spectacles that are affordable, comfortable, cosmetically acceptable and optically accurate may have a role contributing to sustainability when used by trained personnel within the recognised service delivery system of the jurisdiction • Adjustable spectacles used in a way (e.g. -
Binocular Vision Disorders Prescribing Guidelines
Prescribing for Preverbal Children Valerie M. Kattouf O.D. FAAO, FCOVD Illinois College of Optometry Associate Professor Prescribing for Preverbal Children Issues to consider: Age Visual Function Refractive Error Norms Amblyogenic Risk Factors Birth History Family History Developmental History Emmetropization A process presumed to be operative in producing a greater frequency of occurrence of emmetropia than would be expected in terms of chance distribution, as may be explained by postulating that a mechanism coordinates the formation and the development of the various components of the human eye which contribute to the total refractive power Emmetropization Passive process = nature and genetics 60% chance of myopia if 2 parents myopic (Ciuffrieda) Active process = mediated by blur and visual system compensates for blur Refractive Error Norms Highest rate of emmetropization – 1st 12-17 months Hyperopia Average refractive error in infants = +2 D > 1.50 diopters hyperopia at 5 years old – often remain hyperopic Refractive Error Norms Myopia 25% of infants are myopic Myopic Newborns (Scharf) @ 7 years 54% still myopic @ 7 years 46% emmetropic @ 7 years no hyperopia Refractive Error Norms Astigmatism Against the rule astigmatism more prevalent switches to with-the-rule with development At 3 1/2 years old astigmatism is at adult levels INFANT REFRACTION NORMS AGE SPHERE CYL 0-1mo -0.90+/-3.17 -2.02+/-1.43 2-3mo -0.47+/-2.28 -2.02+/-1.17 4-6mo -0.00+/-1.31 -2.20+/-1.15 6-9mo +0.50+/-0.99 -2.20+/-1.15 9-12mo +0.60+/-1.30 -1.64+/-0.62 -

Introduction the Human
Physics 1CL ·OPTICAL INSTRUMENTS AND THE EYE SPRING 2010 Introduction Most of the subject material in this lab can be found in Chapter 25 of Serway and Faughn. In this lab, you will make images of images using lenses and the optical bench (Experiment A). IT IS IMPERATIVE THAT YOU READ CHAPTER 25 BEFORE COMING TO LAB! You will study your own eye as an optical instrument and measure the distance on your retina from the fovea to the “blind spot” (Experiment B). You will also study a model of the eye, and examine the ability of the lens to bring an object into focus at different distances. You will examine how an abnormal eyeball causes blurred vision and how to correct this (Experiment C). There is only one station with the model of the human eye. Whenever that station becomes available, take a few minutes at that station to perform Experiment C. The Human Eye The figure shows a cross section of a human eye. Light is refracted at the surface of the cornea, and is refracted again as it passes through the “crystalline” lens. In a normal eye, light is perfectly focused on the receptors in the retina where signals are generated in nerve fibers and transmitted to the brain. An inverted image is formed on the retina, but the brain “expects” this as normal and is wired to recognize this as normal. Unless you are studying details of the function of the eye, we can consider it to be a single lens (where the focal length can be varied), and a fixed distance from the lens to the retina where we would prefer to make sharply focused images. -

Analysis of Tear Film Spatial Instability for Pediatric Myopia Under Treatment
www.nature.com/scientificreports OPEN Analysis of tear flm spatial instability for pediatric myopia under treatment Wan‑Hua Cho, Po‑Chiung Fang, Hun‑Ju Yu, Pei‑Wen Lin, Hsiu‑Mei Huang & Ming‑Tse Kuo * In Taiwan, the prevalence of myopia in children between 6 and 18 years old is over 80%, and high myopia accounts for over 20%, which turned out to be in the leading place worldwide. Orthokeratology and low-dose atropine are proven treatments to reduce myopia progression, though the potential corneal disturbances remain an issue in young populations. The alteration of the tear flm is widely discussed but there is no consensus to date, so we aim to investigate the tear flm spatial instability in children with myopia control using atropine or orthokeratology. Thirty-eight treatment-naïve participants and 126 myopic children under treatments were enrolled. The ocular surface homeostasis, spatial distribution of tear break-up, and high-order aberrations (HOAs) of the corneal surface were assessed. We found out that myopic children treated with either atropine or orthokeratology showed ocular surface homeostasis similar to that in treatment-naïve children. Nevertheless, children treated with orthokeratology presented higher HOAs (p < 0.00001) and a tendency of the frst tear break-up zone at the inner half of the cornea (p = 0.04). This unique spatial instability of the tear flm associated with myopia treatment might provide a more focused way of monitoring the pediatric tear flm instability. Many studies have revealed diferences in the prevalence of myopia across diferent regions and ethnicities, and the increased rate of myopia is most prominent in Asian/Pacifc children1,2. -
Relationship Between Lenticular Power and Refractive Error in Children with Hyperopia
Clinical Ophthalmology Dovepress open access to scientific and medical research Open Access Full Text Article ORIGINAL RESEARCH Relationship between lenticular power and refractive error in children with hyperopia Takeshi Tomomatsu Objectives: To evaluate the contribution of axial length, and lenticular and corneal power to Shinjiro Kono the spherical equivalent refractive error in children with hyperopia between 3 and 13 years of Shogo Arimura age, using noncontact optical biometry. Yoko Tomomatsu Methods: There were 62 children between 3 and 13 years of age with hyperopia (+2 diopters Takehiro Matsumura [D] or more) who underwent automated refraction measurement with cycloplegia, to measure Yuji Takihara spherical equivalent refractive error and corneal power. Axial length was measured using an optic biometer that does not require contact with the cornea. The refractive power of the lens Masaru Inatani was calculated using the Sanders-Retzlaff-Kraff formula. Single regression analysis was used Yoshihiro Takamura to evaluate the correlation among the optical parameters. For personal use only. Department of Ophthalmology, Results: There was a significant positive correlation between age and axial length P( = 0.0014); Faculty of Medical Sciences, University of Fukui, Fukuiken, Japan however, the degree of hyperopia did not decrease with aging (P = 0.59). There was a significant negative correlation between age and the refractive power of the lens (P = 0.0001) but not that of the cornea (P = 0.43). A significant negative correlation was observed between the degree of hyperopia and lenticular power (P , 0.0001). Conclusion: Although this study is small scale and cross sectional, the analysis, using noncontact biometry, showed that lenticular power was negatively correlated with refractive error and age, indicating that lower lens power may contribute to the degree of hyperopia. -

Refractive Errors a Closer Look
2011-2012 refractive errors a closer look WHAT ARE REFRACTIVE ERRORS? WHAT ARE THE DIFFERENT TYPES OF REFRACTIVE ERRORS? In order for our eyes to be able to see, light rays must be bent or refracted by the cornea and the lens MYOPIA (NEARSIGHTEDNESS) so they can focus on the retina, the layer of light- sensitive cells lining the back of the eye. A myopic eye is longer than normal or has a cornea that is too steep. As a result, light rays focus in front of The retina receives the picture formed by these light the retina instead of on it. Close objects look clear but rays and sends the image to the brain through the distant objects appear blurred. optic nerve. Myopia is inherited and is often discovered in children A refractive error means that due to its shape, your when they are between ages eight and 12 years old. eye doesn’t refract the light properly, so the image you During the teenage years, when the body grows see is blurred. Although refractive errors are called rapidly, myopia may become worse. Between the eye disorders, they are not diseases. ages of 20 and 40, there is usually little change. If the myopia is mild, it is called low myopia. Severe myopia is known as high myopia. Lens Retina Cornea Lens Retina Cornea Light rays Light is focused onto the retina Light rays Light is focused In a normal eye, the cornea and lens focus light rays on in front of the retina the retina. In myopia, the eye is too long or the cornea is too steep. -

Treatment of Pellucid Marginal Degeneration 1Abdelsattar N Farrag, 2Ahmed a Hussein, 3Shiji Ummar
IJKECD Treatment10.5005/jp-journals-10025-1148 of Pellucid Marginal Degeneration REVIEW ARTICLE Treatment of Pellucid Marginal Degeneration 1Abdelsattar N Farrag, 2Ahmed A Hussein, 3Shiji Ummar ABSTRACT Although PMD classically has been affecting the infe- Purpose: To summarize the recent trends in the treatment rior cornea, superior PMD has also been reported, and we of pellucid marginal degeneration (PMD) based on available should consider it in the differential diagnosis of superior published data. corneal ectasia.7 The ectasia in PMD causes progressive Method and literature search: A PubMed search was con- diminution of both uncorrected and corrected visual ducted with combinations not limited to the following search acuity as a result of high against-the-rule astigmatism.1,2 terms: Pellucid marginal degeneration, Corneal ectasia, The condition is most commonly affecting males Corneal collagen cross-linking (CXL), Intracorneal ring seg- ments (ICRS), Contact lens, Keratoplasty in corneal ectasia. and usually presents between the 2nd and 5th decades 3,8 A review of the search results was performed and relevant of life. articles to the topic were included. The PMD can be diagnosed classically by slit-lamp Summary: Ophthalmologists have got a wide array of thera- examination, which shows a clear band of inferior corneal peutic modalities for the management of PMD. However, the key thinning extending from 4 to 8 o’clock. There is typically to optimal treatment is careful clinical assessment of patients a 1 to 2 mm of uninvolved normal cornea. The maximum and their visual requirements and tailoring the treatment to point of protrusion in PMD occurs in the area superior individual patients. -

CHAMP Brochure
To learn more about this study, please contact: Myopia can keep your child from seeing the full picture. Who is eligible to participate in the CHAMP study? To pre-qualify for this study, your child must: • Be 3 to 17 years of age • Have been diagnosed with myopia Further screening questions will be asked prior to scheduling an appointment. Learn more about CHAMP – the study of an investigational eye drop being evaluated to slow the progression of nearsightedness (myopia) in children. 21Dec2017_V1_CP-NVK002-0001_Brochure_English What will happen during the CHAMP study? • Your child will receive one drop of study medication into each eye once daily at bedtime for 4 years. • Your child’s total study participation will last approximately 4 years. • During this time, you will attend clinic visits every 3 months to receive study medication. • Every 6 months the doctor will monitor your child’s myopia closely. Your child’s eyewear prescription, the length of his or her eyes, visual function, and eye What is myopia? health will be assessed. Why should my child participate in the CHAMP study? Myopia, commonly known as “nearsightedness,” is when the eye grows too long and light does not focus accurately Myopia is increasing at an alarming rate worldwide. on the retina. This causes distant objects to appear blurry. Identifying a way to control myopia progression is a key step Typically, myopia increases during school years. Higher towards preserving eye sight and preventing serious eye myopia results in the need for thicker glasses and increases disease. By participating in this study, you and your child the risk of certain eye diseases, such as glaucoma and retinal become an important part of this effort. -
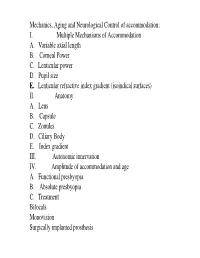
I. Multiple Mechanisms of Accommodation A. Variable Axial Length B
Mechanics, Aging and Neurological Control of accommodation: I. Multiple Mechanisms of Accommodation A. Variable axial length B. Corneal Power C. Lenticular power D. Pupil size E. Lenticular refractive index gradient (isoindical surfaces) II. Anatomy A. Lens B. Capsule C. Zonules D. Ciliary Body E. Index gradient III. Autonomic innervation IV. Amplitude of accommodation and age A. Functional presbyopia B. Absolute presbyopia C. Treatment Bifocals Monovision Surgically implanted prosthesis Course title - (VS217) Oculomotor functions and neurology Instructor - Clifton Schor GSI: James O’Shea, Michael Oliver & Aleks Polosukhina Schedule of lectures, exams and laboratories : Lecture hours 10-11:30 Tu Th; 5 min break at 11:00 Labs Friday the first 3 weeks Examination Schedule : Quizes: January 29; February 28 Midterm: February 14: Final March 13 Power point lecture slides are available on a CD Resources: text books, reader , website, handouts Class Website: Reader. Website http://schorlab.berkeley.edu Click courses 117 class page name VS117 password Hering,1 First Week: read chapters 16-18 See lecture outline in syllabus Labs begin this Friday, January 25 Course Goals Near Response - Current developments in optometry Myopia control – environmental, surgical, pharmaceutical and genetic Presbyopia treatment – amelioration and prosthetic treatment Developmental disorders (amblyopia and strabismus) Reading disorders Ergonomics- computers and sports vision Virtual reality and personal computer eye-ware Neurology screening- Primary care gate keeper neurology, systemic, endocrines, metabolic, muscular skeletal systems. Mechanics, Aging and Neurological Control of accommodation : I. Five Mechanisms of Accommodation A. Variable axial length B. Corneal Power and astigmatism C. Lenticular power D. Pupil size & Aberrations E. Lenticular refractive index gradient (isoindical surfaces) II. -

Practical Tips for Managing Myopia
MYOPIA MANAGEMENT Practical tips for managing myopia Michael Morton This article presents a summary of Online Education Coordinator: practical approaches to diagnosing Brien Holden Vision myopia, myopia management Institute, Sydney, Australia. (with particular attention to low resource settings), reviewing myopia progression, and collecting data for myopia management programmes. Ling Lee Research Officer/ Optometrist: Part 1 Diagnosing and prescribing Brien Holden Vision Institute, Sydney, for myopia Australia. While myopia might be initially detected by a patient EDGARDO CONTRERAS, COURTESY OF IAPB (e.g. reporting distance blur), or an adult observing Refraction is the first step. MEXICO behaviour changes in a child (e.g. squinting or • Monocular estimate method (MEM) retinoscopy. viewing things closer than expected), myopia is generally An objective method to determine a child’s diagnosed by an eye care professional. accommodative (near focussing) status at near. Priya Morjaria Equipment Retinoscopy should be conducted with a near target. Research Fellow: Accommodative facility. A subjective method to Department of The minimum required equipment to diagnose myopia • Clinical Research, and assess progression includes: assess accommodation function (ability of eye to London School focus at near). A high-contrast distance visual acuity (VA) chart (e.g., of Hygiene and • • Subjective phorias. A subjective method to Tropical Medicine, Snellen, logMAR, E, or LEA) determine whether the eyes prefer to converge in or International Centre • A room or space where the viewing distance for VA diverge out, at distance and near. for Eye Health, is at least 3m/10ft. The chart should be well lit and • Vergence reserves. A subjective method that London, UK. calibrated for the working distance measures the eyes’ ability to converge in and • Occluder (ideally with pinhole occluder) diverge out. -

Presbyopia Presbyopia Is a Common Type of Vision Disorder That Occurs As You Age
National Eye Institute Eye Institute National Institutes Institutes of Health of Health Presbyopia Presbyopia is a common type of vision disorder that occurs as you age. It is often referred to as the aging eye condition. Presbyopia results in the inability to focus up close, a problem associated with refraction in the eye. What is presbyopia? Presbyopia is a common type of vision disorder that occurs as you age. It is often referred to as the aging eye condition. Presbyopia results in the inability to focus up close, a problem associated with refraction in the eye. Can I have presbyopia and another type of refractive error at the same time? Yes. It is common to have presbyopia and another type of refractive error at the same time. There are several other types of refractive errors: myopia (nearsightedness), hyperopia (farsightedness), and astigmatism. An individual may have one type of refractive error in one eye and a different type of refractive error in the other. Presbyopia 1 What is refraction? Refraction is the bending of light as it passes through one object to another. Vision occurs when light rays are bent (refracted) by the cornea and lens. The light is then focused directly on the retina, which is a light-sensitive tissue at the back of the eye. The retina converts the light-rays into messages that are sent through the optic nerve to the brain. The brain interprets these messages into the images we see. How does presbyopia occur? Presbyopia happens naturally in people as they age. The eye is not able to focus light directly on to the retina due to the hardening of the natural lens. -

The Definition and Classification of Dry Eye Disease
DEWS Definition and Classification The Definition and Classification of Dry Eye Disease: Report of the Definition and Classification Subcommittee of the International Dry E y e W ork Shop (2 0 0 7 ) ABSTRACT The aim of the DEWS Definition and Classifica- I. INTRODUCTION tion Subcommittee was to provide a contemporary definition he Definition and Classification Subcommittee of dry eye disease, supported within a comprehensive clas- reviewed previous definitions and classification sification framework. A new definition of dry eye was devel- T schemes for dry eye, as well as the current clinical oped to reflect current understanding of the disease, and the and basic science literature that has increased and clarified committee recommended a three-part classification system. knowledge of the factors that characteriz e and contribute to The first part is etiopathogenic and illustrates the multiple dry eye. Based on its findings, the Subcommittee presents causes of dry eye. The second is mechanistic and shows how herein an updated definition of dry eye and classifications each cause of dry eye may act through a common pathway. based on etiology, mechanisms, and severity of disease. It is stressed that any form of dry eye can interact with and exacerbate other forms of dry eye, as part of a vicious circle. II. GOALS OF THE DEFINITION AND Finally, a scheme is presented, based on the severity of the CLASSIFICATION SUBCOMMITTEE dry eye disease, which is expected to provide a rational basis The goals of the DEWS Definition and Classification for therapy. These guidelines are not intended to override the Subcommittee were to develop a contemporary definition of clinical assessment and judgment of an expert clinician in dry eye disease and to develop a three-part classification of individual cases, but they should prove helpful in the conduct dry eye, based on etiology, mechanisms, and disease stage.