Wills Eye Manual 3Ed.Pdb
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ocular Injury; Hazard to Society: a Case Series
Quest Journals Journal of Medical and Dental Science Research Volume 7~ Issue 8 (2020) pp: 34-44 ISSN(Online) : 2394-076X ISSN (Print):2394-0751 www.questjournals.org Research Paper Ocular Injury; Hazard to Society: A Case Series Dr Rashmi kujur1, Dr Pallavi. M.P2, Dr Harshita Dubey3, Dr Varsha4 1Dept. of ophthalmology, Madhav dispensary JAH, GRMC, Gwalior, Madhyapradesh. 2Senior girls hostel, GRMC, Gwalior, Madhyapradesh. 3Senior girls hostel, GRMC, Gwalior, Madhyapradesh. 4Senior girls hostel, GRMC, Gwalior,Madhyapradesh. Corresponding Author: Dr.Pallavi.M.P ABSTRACT Purpose: To describe various types of ocular trauma due to different modes of injuryoccured on the same day Design: Prospective interventional study (case series) Materials & Methods: A series of cases of ocular trauma in different age group on the same day. Results: Five patients of ocular trauma were studied & managed. All five patients were males. Out of 5 cases, 3 cases had open globe injury and 2 cases had closed globe injury. Three out of five patients required surgical intervention while 2 patients were managed with medical therapy. Conclusion: This study describes the types and characteristics of ocular trauma presenting in eye department. The frequency of ocular trauma is common in males. Eye injuries resulting from ocular trauma pose a frequent threat to vision the world over. While afocussed history and prompt ocular examination are essential to immediate management, patient educationregarding safety precautions and risk reduction help to prevent future recurrences. KEYWORDS: Ocular morbidity, Ocular Injury, globe rupture, iridodialysis, fire cracker injury, hyphema, Road Traffic accident (RTA), loss of vision. Received 05 December, 2020; Accepted 20 December, 2020 © The author(s) 2020. -

Anesthesia for Eye Surgery
Anesthesia for Eye Surgery Having a surgery can be stressful. We would like to provide you the following information to help you prepare for your eye surgery. Eye surgeries are typically done under topical or local anesthesia with or without mild sedation. Topical Anesthesia This is administered via special eye drops by a preoperative nurse. Local Anesthesia This is administered via injection by an ophthalmologist. Your ophthalmologist will inject local anesthesia to the eye that is to undergo the operation. During the injection, you will be lightly sedated. In the operating room During the procedure it is very important that you remain still. This is a very delicate surgery; any abrupt movement can hinder a surgeon’s performance. If you have any concerns during the surgery, such as pain, urge to cough or itching, please let us know immediately. Typically, patients are not heavily sedated for this type of procedure. Therefore, it is normal for patients to feel pressure around their eyes, but not pain. In order to maintain surgical sterility, your face and body will be covered with a sterile drape. You will be given supplemental oxygen to breathe. An anesthesia clinician will continue to monitor your vital signs for the duration of the procedure. The length of the procedure usually ranges from 10 minutes to 30 minutes. In the recovery room After surgery, you will be brought to the recovery room. A recovery room nurse will continue to monitor your vital signs for the next 20 to 30 minutes. It is important that you do not drive or operate any machinery for the next 24 hours. -

Table of Contents
Leadership Development Program Project Abstracts Table of Contents LDP XXII, CLASS OF 2020 GRADUATES Name/Society/Project Page John J. Chen, MD, PhD 1 North American Neuro-Ophthalmology Society Project: The Neuro-Ophthalmology career path: misconceptions and barriers to recruitment Jeremy D. Clark, MD 2 Kentucky Academy of Eye Physicians and Surgeons Project: The Web of Innovation: Silent Auction Benefitting Political Action funds in Kentucky Gennifer J. Greebel, MD 3 New York State Ophthalmological Society Project: Inspiring Professional Aspirations in Adolescents with Low Vision Mark A. Greiner, MD 4 Eye Bank Association of America Project: Revisiting Eye Banking Medical Standards To Accommodate Emerging Technologies Jennifer F. Jordan, MD 5 North Carolina Society of Eye Physicians and Surgeons Project: Advocacy Exposure for North Carolina Ophthalmologists in Training Kapil G. Kapoor, MD 6 Virginia Society of Eye Physicians and Surgeons Project: Unwrapping Virginia Bill 506B Erin Lichtenstein, MD 7 Maine Society of Eye Physicians and Surgeons Project: Bringing Ophthalmology Residents to Maine Jennifer L. Lindsey, MD 8 Association of Veterans Affairs Ophthalmologists Project: Illuminating the Path to Advocacy for Veterans Affairs Ophthalmologists Donald A. Morris, DO 9 American Osteopathic College of Ophthalmology Project: Single Accreditation of Ophthalmology residencies is here. What is the next step? Lisa Nijm, MD, JD 10 Women in Ophthalmology Project: Implementing a Clinical Trials Training Program to Increase Diversity of Primary Investigators Involved in Ophthalmic Research LDP XXII, CLASS OF 2020 GRADUATES (cont’d) Name/Society/Project Page Roma P. Patel, MD, MBA 11 California Academy of Eye Physicians and Surgeons Project: Increasing Membership Value to our CAEPS Members Jelena Potic, MD, PhD 12 European Society of Ophthalmology Project: Harmonization of Surgical Skills Standards for Young Ophthalmologists across Europe Pradeep Y. -

Laser Vision Correction Surgery
Patient Information Laser Vision Correction 1 Contents What is Laser Vision Correction? 3 What are the benefits? 3 Who is suitable for laser vision correction? 4 What are the alternatives? 5 Vision correction surgery alternatives 5 Alternative laser procedures 5 Continuing in glasses or contact lenses 5 How is Laser Vision Correction performed? 6 LASIK 6 Surface laser treatments 6 SMILE 6 What are the risks? 7 Loss of vision 7 Additional surgery 7 Risks of contact lens wear 7 What are the side effects? 8 Vision 8 Eye comfort 8 Eye Appearance 8 Will laser vision correction affect my future eye health care? 8 How can I reduce the risk of problems? 9 How much does laser vision correction cost? 9 2 What is Laser Vision Correction? Modern surgical lasers are able to alter the curvature and focusing power of the front surface of the eye (the cornea) very accurately to correct short sight (myopia), long sight (hyperopia), and astigmatism. Three types of procedure are commonly used in If you are suitable for laser vision correction, your the UK: LASIK, surface laser treatments (PRK, surgeon will discuss which type of procedure is the LASEK, TransPRK) and SMILE. Risks and benefits are best option for you. similar, and all these procedures normally produce very good results in the right patients. Differences between these laser vision correction procedures are explained below. What are the benefits? For most patients, vision after laser correction is similar to vision in contact lenses before surgery, without the potential discomfort and limitations on activity. Glasses may still be required for some activities after Short sight and astigmatism normally stabilize in treatment, particularly for reading in older patients. -

New Horizons Forum
Speeding the development of new therapies and diagnostics for glaucoma patients New Horizons Forum Friday, February 9, 2018 Palace Hotel, San Francisco, CA © Aerie Pharmaceuticals, Inc. Irvine, CA 92614 Follow the meeting on Twitter: #Glaucoma360 MLR-0002 Glaucoma Research Foundation thanks the following sponsors WELCOME for their generous support of Glaucoma 360 PLATINUM It is our sincere pleasure to welcome you to the 7th Annual Glaucoma 360: New Horizons Forum, hosted by Glaucoma Research Foundation. This important meeting provides a unique opportunity to bring together leaders in medicine, science, industry, venture capital, and the FDA to discuss emerging ideas in glaucoma and encourage collaboration to accelerate their development for clinical use. Since its establishment in 2012, this annual forum continues to grow and provide the ultimate opportunity to highlight important advances and facilitate networking between these essential groups. As a result, there are now more effective therapies and diagnostic tools in clinical practice today to help doctors manage the disease more effectively. But, unmet medical needs remain in glaucoma. Glaucoma Research Foundation is resolute in its mission to preserve vision and continue its role as a catalyst in the advancement of research towards new treatments and a cure. SILVER Glaucoma 360 would not be possible without the generous and selfless contributions of so many including: members of our Advisory Board, Program and Steering Committees who have volunteered their time to build an outstanding agenda; our dedicated sponsors who have helped to underwrite this event; our speakers, presenters, and panelists who are ready to share their expertise and unique perspectives; our attendees; the support of our Board of Directors and staff at Glaucoma Research Foundation; and the hard working team at The Palace Hotel. -

Traumatic Retinal Detachment Br J Ophthalmol: First Published As 10.1136/Bjo.75.1.18 on 1 January 1991
18 BritishJournalofOphthalmology, 1991,75, 18-21 Traumatic retinal detachment Br J Ophthalmol: first published as 10.1136/bjo.75.1.18 on 1 January 1991. Downloaded from P B Johnston Abstract trauma is a well recognised cause of rhegmato- Seventy-seven patients developed retinal genous retinal detachment, which was reported breaks following an episode of ocular con- by Eagling' to affect 4-6% of such injuries. The tusion, and 65 (84.4%) of these developed characteristics of postcontusion retinal detach- rhegmatogenous retinal detachment. Surgical ments were described by Cox et all and the treatment successfully restored or maintained mechanism ofbreak formation was elucidated by retinal apposition in 74 (96-1%) of the eyes. Delori et all who studied the effect of high speed Thirty-six (46-8%) eyes recovered visual acuity projectiles on enucleated pig eyes. Experimental of6/9orbetter. Ofthe retinal breaks recognised evidence indicates that retinal breaks form at the dialysis at the ora serrata was observed in 49 time of ocular impact. However, clinical reports eyes, of which 28 were situated at the lower show considerable delay in the diagnosis of temporal quadrant. Seventeen eyes had post-traumatic retinal detachment. For example, irregular breaks arising within necrotic retina Cox et all reported that only 30% of post- at the site of scleral impact. Twenty-four traumatic retinal detachments were diagnosed (31.2%) patients had retinal break or retinal within one month of injury, and Ross4 found detachment diagnosed within 24 hours ofinjury 40% in a similar period. and 49 (63-6%) within six weeks. Immediate The following study is of a series of patients retinal detachment was a feature of necrotic who developed retinal breaks or retinal detach- retinal breaks, while inferior oral dialyses led ment after ocular contusion. -

Vertical Perspective Medical Assistance Program
Kansas Vertical Perspective Medical Assistance Program December 2006 Provider Bulletin Number 688 General Providers Emergent and Nonemergent Diagnosis Code List Attached is a list of diagnosis codes and whether the Kansas Medical Assistance Program (KMAP) considers the code to be emergent or nonemergent. Providers are responsible for validating whether a particular diagnosis code is covered by KMAP under the beneficiary’s benefit plan and that all program requirements are met. This list does not imply or guarantee payment for listed diagnosis codes. Information about the Kansas Medical Assistance Program as well as provider manuals and other publications are on the KMAP Web site at https://www.kmap-state-ks.us. If you have any questions, please contact the KMAP Customer Service Center at 1-800-933-6593 (in-state providers) or (785) 274-5990 between 7:30 a.m. and 5:30 p.m., Monday through Friday. EDS is the fiscal agent and administrator of the Kansas Medical Assistance Program for the Kansas Health Policy Authority. Page 1 of 347 Emergency Indicators as noted by KMAP: N – Never considered emergent S – Sometimes considered emergent (through supporting medical documentation) Y – Always considered emergent Diagnosis Emergency Diagnosis Code Description Code Indicator 0010 Cholera due to Vibrio Cholerae S 0011 Cholera due to Vibrio Cholerae El Tor S 0019 Unspecified Cholera S 019 Late Effects of Tuberculosis N 0020 Typhoid Fever S 0021 Paratyphoid Fever A S 0022 Paratyphoid Fever B S 0023 Paratyphoid Fever C S 024 Glanders Y 025 Melioidosis -
Root Eye Dictionary a "Layman's Explanation" of the Eye and Common Eye Problems
Welcome! This is the free PDF version of this book. Feel free to share and e-mail it to your friends. If you find this book useful, please support this project by buying the printed version at Amazon.com. Here is the link: http://www.rooteyedictionary.com/printversion Timothy Root, M.D. Root Eye Dictionary A "Layman's Explanation" of the eye and common eye problems Written and Illustrated by Timothy Root, M.D. www.RootEyeDictionary.com 1 Contents: Introduction The Dictionary, A-Z Extra Stuff - Abbreviations - Other Books by Dr. Root 2 Intro 3 INTRODUCTION Greetings and welcome to the Root Eye Dictionary. Inside these pages you will find an alphabetical listing of common eye diseases and visual problems I treat on a day-to-day basis. Ophthalmology is a field riddled with confusing concepts and nomenclature, so I figured a layman's dictionary might help you "decode" the medical jargon. Hopefully, this explanatory approach helps remove some of the mystery behind eye disease. With this book, you should be able to: 1. Look up any eye "diagnosis" you or your family has been given 2. Know why you are getting eye "tests" 3. Look up the ingredients of your eye drops. As you read any particular topic, you will see that some words are underlined. An underlined word means that I've written another entry for that particular topic. You can flip to that section if you'd like further explanation, though I've attempted to make each entry understandable on its own merit. I'm hoping this approach allows you to learn more about the eye without getting bogged down with minutia .. -

Cme Reviewarticle
Volume 58, Number 2 OBSTETRICAL AND GYNECOLOGICAL SURVEY Copyright © 2003 by Lippincott Williams & Wilkins, Inc. CME REVIEWARTICLE 5 CHIEF EDITOR’S NOTE: This article is part of a series of continuing education activities in this Journal through which a total of 36 AMA/PRA category 1 credit hours can be earned in 2003. Instructions for how CME credits can be earned appear on the last page of the Table of Contents. Ocular Changes in Pregnancy Robert B. Dinn, BS,* Alon Harris, MSc, PhD† and Peter S. Marcus, MD‡ *Fourth Year Medical Student, Indiana University School of Medicine; †Professor, Glaucoma Research and Diagnostic Center, Departments of Ophthalmology and Physiology, Indiana University School of Medicine; and ‡Assistant Clinical Professor, Department of Obstetrics and Gynecology, Indiana University School of Medicine, Indianapolis, Indiana Visual changes in pregnancy are common, and many are specifically associated with the preg- nancy itself. Serous retinal detachments and blindness occur more frequently during preeclampsia and often subside postpartum. Pregnant women are at increased risk for the progression of preexisting proliferative diabetic retinopathy, and diabetic women should see an ophthalmologist before pregnancy or early in the first trimester. The results of refractive eye surgery before, during, or immediately after pregnancy are unpredictable, and refractive surgery should be postponed until there is a stable postpartum refraction. A decreased tolerance to contact lenses also is common during pregnancy; therefore, it is advisable to fit contact lenses postpartum. Furthermore, preg- nancy is associated with a decreased intraocular pressure in healthy eyes, and the effects of glaucoma medications on the fetus and breast-fed infant are largely unknown. -
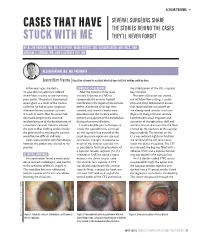
Cases That Have Stuck with Me
OCULAR TRAUMA s SEVERAL SURGEONS SHARE CASES THAT HAVE THE STORIES BEHIND THE CASES STUCK WITH ME THEY’LL NEVER FORGET BY ALLON BARSAM, MD, MA, FRCOPHTH; MARK KONTOS, MD; SOOSAN JACOB, MD, FRCS, DNB; MICHAEL E. SNYDER, MD; AND ELIZABETH YEU, MD ALLON BARSAM, MD, MA, FRCOPHTH Severe Blunt Trauma | A positive outcome for a patient who had been told that nothing could be done. A few years ago, I treated a SURGICAL PROCEDURE the stabilization of the IOL –capsular 41-year-old man who had suffered After the creation of the main bag complex. severe blunt trauma to one eye many incision, I injected an OVD to Phacoemulsification was carried years earlier. The patient experienced tamponade the anterior hyaloid out with low flow settings. I used a severe glare as a result of the trauma, membrane in the region of the zonular stop-and-chop technique to ensure such that he had to wear sunglasses defect. A cohesive OVD was then that minimal force was placed on whenever he was outdoors or even injected, and three iris hooks were the already weak zonular structures in a well-lit room. Also, his vision had placed to keep the iris back and to (Figure 2). Using a Simcoe cannula, decreased progressively since the prevent propagation of the iridodialysis I performed manual irrigation and incident because of the development of during phacoemulsification. aspiration of the epinuclear shell and a traumatic cataract. Doctors advised I used a double-pass technique to soft lens matter to ensure that the force the patient that nothing could remedy create the capsulorhexis, centered exerted on the contents of the capsular the glare and that treating the cataract on the capsular bag instead of the bag was gentle. -

Eleventh Edition
SUPPLEMENT TO April 15, 2009 A JOBSON PUBLICATION www.revoptom.com Eleventh Edition Joseph W. Sowka, O.D., FAAO, Dipl. Andrew S. Gurwood, O.D., FAAO, Dipl. Alan G. Kabat, O.D., FAAO Supported by an unrestricted grant from Alcon, Inc. 001_ro0409_handbook 4/2/09 9:42 AM Page 4 TABLE OF CONTENTS Eyelids & Adnexa Conjunctiva & Sclera Cornea Uvea & Glaucoma Viitreous & Retiina Neuro-Ophthalmic Disease Oculosystemic Disease EYELIDS & ADNEXA VITREOUS & RETINA Blow-Out Fracture................................................ 6 Asteroid Hyalosis ................................................33 Acquired Ptosis ................................................... 7 Retinal Arterial Macroaneurysm............................34 Acquired Entropion ............................................. 9 Retinal Emboli.....................................................36 Verruca & Papilloma............................................11 Hypertensive Retinopathy.....................................37 Idiopathic Juxtafoveal Retinal Telangiectasia...........39 CONJUNCTIVA & SCLERA Ocular Ischemic Syndrome...................................40 Scleral Melt ........................................................13 Retinal Artery Occlusion ......................................42 Giant Papillary Conjunctivitis................................14 Conjunctival Lymphoma .......................................15 NEURO-OPHTHALMIC DISEASE Blue Sclera .........................................................17 Dorsal Midbrain Syndrome ..................................45 -

Interesting and Artistic 1 2 3 Grand Prize Winner
s BEST OF 2018: PHOTO CONTEST 1 s SERGEI LUZHETSKIY, MD DANIEL DE SOUZA A Dog’s Cataract COSTA, MD s 2 A Spontaneous Displacement of the Lens WINNER GRAND PRIZE WINNER s PATRIK RAJS Gramophone Record 3 in the Eye INTERESTING AND ARTISTIC YONG s WINNERS OF KAM, MD Anterior CRST’S ANNUAL Segment Dysgenesis 2018 PHOTO CONTEST INTERESTING AND ARTISTIC 1 This is an image of an inherited cataract in a dog. 2 This photo is of the eye of a 46-year-old woman who presented with displacement of the lens into the anterior 4 chamber with no history of ocular trauma. 3 This photo is of the eye of a patient with presbyopia who underwent laser cataract surgery. A multifocal IOL was captured GRAND with a combination of two vintage Zeiss and Pentax lenses. WINNER PRIZE RARE AND UNUSUAL WINNER s This photo shows the eye of a newborn patient with DANIEL 4 increased IOP; a diffusely edematous, hazy, and enlarged DE SOUZA cornea; and an absent Schlemm canal and trabecular COSTA, MD meshwork on surgical exploration, consistent with severe A Prominent anterior segment dysgenesis. Symblepharon 5 The eye of this 5-year-old girl has epidermolysis bullosa and serious ocular manifestations of this condition. Biomicroscopy examination revealed the presence of 5 6 symblepharon in both eyes. The ocular complication was so severe that it deformed the palpebral anatomy. Significant keratoglobus in the eye of this patient with s AARON S. WANG, MD 6 Fish Tank Down Syndrome, who frequently rubs his eyes. This picture RARE AND UNUSUAL was taken just prior to corneal transplantation.