Staying Healthy During a Mouse Plague
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Q Fever in Small Ruminants and Its Public Health Importance
Journal of Dairy & Veterinary Sciences ISSN: 2573-2196 Review Article Dairy and Vet Sci J Volume 9 Issue 1 - January 2019 Copyright © All rights are reserved by Tolera Tagesu Tucho DOI: 10.19080/JDVS.2019.09.555752 Q Fever in Small Ruminants and its Public Health Importance Tolera Tagesu* School of Veterinary Medicine, Jimma University, Ethiopia Submission: December 01, 2018; Published: January 11, 2019 *Corresponding author: Tolera Tagesu Tucho, School of Veterinary Medicine, Jimma University, Jimma Oromia, Ethiopia Abstract Query fever is caused by Coxiella burnetii, it’s a worldwide zoonotic infectious disease where domestic small ruminants are the main reservoirs for human infections. Coxiella burnetii, is a Gram-negative obligate intracellular bacterium, adapted to thrive within the phagolysosome of the phagocyte. Humans become infected primarily by inhaling aerosols that are contaminated with C. burnetii. Ingestion (particularly drinking raw milk) and person-to-person transmission are minor routes. Animals shed the bacterium in urine and feces, and in very high concentrations in birth by-products. The bacterium persists in the environment in a resistant spore-like form which may become airborne and transported long distances by the wind. It is considered primarily as occupational disease of workers in close contact with farm animals or processing their be commenced immediately whenever Q fever is suspected. To prevent both the introduction and spread of Q fever infection, preventive measures shouldproducts, be however,implemented it may including occur also immunization in persons without with currently direct contact. available Doxycycline vaccines drugof domestic is the first small line ruminant of treatment animals for Q and fever. -

Zoonotic Diseases of Public Health Importance
ZOONOTIC DISEASES OF PUBLIC HEALTH IMPORTANCE ZOONOSIS DIVISION NATIONAL INSTITUTE OF COMMUNICABLE DISEASES (DIRECTORATE GENERAL OF HEALTH SERVICES) 22 – SHAM NATH MARG, DELHI – 110 054 2005 List of contributors: Dr. Shiv Lal, Addl. DG & Director Dr. Veena Mittal, Joint Director & HOD, Zoonosis Division Dr. Dipesh Bhattacharya, Joint Director, Zoonosis Division Dr. U.V.S. Rana, Joint Director, Zoonosis Division Dr. Mala Chhabra, Deputy Director, Zoonosis Division FOREWORD Several zoonotic diseases are major public health problems not only in India but also in different parts of the world. Some of them have been plaguing mankind from time immemorial and some have emerged as major problems in recent times. Diseases like plague, Japanese encephalitis, leishmaniasis, rabies, leptospirosis and dengue fever etc. have been major public health concerns in India and are considered important because of large human morbidity and mortality from these diseases. During 1994 India had an outbreak of plague in man in Surat (Gujarat) and Beed (Maharashtra) after a lapse of around 3 decades. Again after 8 years in 2002, an outbreak of pneumonic plague occurred in Himachal Pradesh followed by outbreak of bubonic plague in 2004 in Uttaranchal. Japanese encephalitis has emerged as a major problem in several states and every year several outbreaks of Japanese encephalitis are reported from different parts of the country. Resurgence of Kala-azar in mid seventies in Bihar, West Bengal and Jharkhand still continues to be a major public health concern. Efforts are being made to initiate kala-azar elimination programme by the year 2010. Rabies continues to be an important killer in the country. -
Biannual Communicable Disease Surveillance Report #2
BIANNUAL COMMUNICABLE DISEASE SURVEILLANCE REPORT #2 An overview of the public health nurse surveillance of THE TOWN communicable diseases in Grafton, MA, Jan 1 – Dec 31, 2020. 2020OF GRAFTON Grafton Biannual Communicable Disease Surveillance Report #2, 2020 Defining Case Classifications for Communicable Diseases In the U.S., the States mandate the reporting of certain diseases by law or by regulation. The diseases that are reportable to state and local health departments differ from state to state; however, certain diseases are considered nationally notifiable diseases. The list of nationally notifiable diseases is updated annually. The Centers for Disease Control and Prevention (CDC), in collaboration with the Council of State and Territorial Epidemiologists (CSTE), publishes case definitions for public health surveillance for the nationally notifiable diseases. These case definitions provide uniform criteria for reporting cases and are case specific. The case status for most diseases is determined as follows: • A confirmed case is one in which the clinical case description is met and the laboratory confirmation requirement is met. A case may also be considered confirmed if it is linked to a laboratory-confirmed case. Certain diseases may not include laboratory findings as testing is not available. • A probable case is one in which the clinical case description is met and there is supportive or presumptive laboratory results consistent with the diagnosis but, it does not meet the laboratory confirmed criteria. • A suspect case is one in which the clinical case description is met. • A revoked case is one in which neither the suspect, probable, nor confirmed case definition is met. A significant amount of information gathering must be collected for many diseases before a case classification is final. -

61% of All Human Pathogens Are Zoonotic (Passed from Animals to Humans), and Many Are Transmitted Through Inhaling Dust Particles Or Contact with Animal Wastes
Zoonotic Diseases Fast Facts: 61% of all human pathogens are zoonotic (passed from animals to humans), and many are transmitted through inhaling dust particles or contact with animal wastes. Some of the diseases we can get from our pets may be fatal if they go undetected or undiagnosed. All are serious threats to human health, but can usually be avoided by observing a few precautions, the most effective of which is washing your hands after touching animals or their wastes. Regular visits to the veterinarian for prevention, diagnosis, and treatment of zoonotic diseases will help limit disease in your pet. Source: http://www.cdc.gov/healthypets/ Some common zoonotic diseases humans can get through their pets: Zoonotic Disease & its Effect on How Contact is Made Humans Bartonellosis (cat scratch disease) – an Bartonella bacteria are transferred to humans through infection from the bacteria Bartonella a bite or scratch. Do not play with stray cats, and henselae that causes fever and swollen keep your cat free of fleas. Always wash hands after lymph nodes. handling your cat. Capnocytophaga infection – an Capnocytophaga canimorsus is the main human infection caused by bacteria that can pathogen associated with being licked or bitten by an develop into septicemia, meningitis, infected dog and may present a problem for those and endocarditis. who are immunosuppressed. Cellulitis – a disease occurring when Bacterial organisms from the Pasteurella species live bacteria such as Pasteurella multocida in the mouths of most cats, as well as a significant cause a potentially serious infection of number of dogs and other animals. These bacteria the skin. -

Enteric Infections Due to Campylobacter, Yersinia, Salmonella, and Shigella*
Bulletin of the World Health Organization, 58 (4): 519-537 (1980) Enteric infections due to Campylobacter, Yersinia, Salmonella, and Shigella* WHO SCIENTIFIC WORKING GROUP1 This report reviews the available information on the clinical features, pathogenesis, bacteriology, and epidemiology ofCampylobacter jejuni and Yersinia enterocolitica, both of which have recently been recognized as important causes of enteric infection. In the fields of salmonellosis and shigellosis, important new epidemiological and relatedfindings that have implications for the control of these infections are described. Priority research activities in each ofthese areas are outlined. Of the organisms discussed in this article, Campylobacter jejuni and Yersinia entero- colitica have only recently been recognized as important causes of enteric infection, and accordingly the available knowledge on these pathogens is reviewed in full. In the better- known fields of salmonellosis (including typhoid fever) and shigellosis, the review is limited to new and important information that has implications for their control.! REVIEW OF RECENT KNOWLEDGE Campylobacterjejuni In the last few years, C.jejuni (previously called 'related vibrios') has emerged as an important cause of acute diarrhoeal disease. Although this organism was suspected of being a cause ofacute enteritis in man as early as 1954, it was not until 1972, in Belgium, that it was first shown to be a relatively common cause of diarrhoea. Since then, workers in Australia, Canada, Netherlands, Sweden, United Kingdom, and the United States of America have reported its isolation from 5-14% of diarrhoea cases and less than 1 % of asymptomatic persons. Most of the information given below is based on conclusions drawn from these studies in developed countries. -

Salmonella Is One of the Most Common Foodborne Infections
Salmonellosis is one of the most common foodborne infections in the United States, resulting in an estimated 1.2 million human cases and $365 million in direct medical costs annually (2011 estimates). Signs and Symptoms When Salmonella bacteria are ingested, they pass through a person’s stomach and colonize the small and large intestine. There, the bacteria invade the intestinal mucosa and proliferate. The bacteria can invade the lymphoid tissues of the gastrointestinal tract and spread to the bloodstream. Dissemination to the bloodstream depends on host factors and virulence of the Salmonella strain and occurs in less than 5% of infections. If the infection spreads to the bloodstream, any organ can become infected (e.g., liver, gallbladder, bones, or meninges). The incubation period for salmonellosis is approximately 12–72 hours, but it can be longer. Salmonella gastroenteritis is characterized by the sudden onset of • diarrhea (sometime blood-tinged), • abdominal cramps • fever, and • occasionally nausea and vomiting. Illness usually lasts 4–7 days. If the infection spreads to the bloodstream and distant organs, the illness increases in duration and severity and will usually include signs and symptoms related to the organ affected. A small proportion of persons infected with Salmonella develop reactive arthritis as a long-term sequela of the infection. Diagnosis Multiple diseases can cause fever, diarrhea, and abdominal cramps. Therefore, salmonellosis cannot be diagnosed on the basis of symptoms alone. To diagnose salmonellosis, the bacterium is usually isolated in the laboratory from the patient's stool. The genus Salmonella is identified by using a series of biochemical tests. Subtyping (e.g., serotyping, pulsed field gel electrophoresis, and other tests) and antimicrobial susceptibility testing of Salmonella isolates are important adjuncts to the diagnostic testing of patients. -
CHAPTER 4 Infectious Disease
CHAPTER 4 Infectious Disease 99 | Massachusetts State Health Assessment Infectious Disease This chapter provides information on preventing and controlling infectious diseases, and related trends, disparities, and resources in the Commonwealth of Massachusetts. It addresses the following infectious disease topic areas: • Foodborne Diseases • Healthcare-Associated Infections • Sexually Transmitted Infections • Human Immunodeficiency Virus • Viral Hepatitis • Tuberculosis • Vectorborne Diseases • Immunization • Selected Resources, Services, and Programs Chapter Data Highlights • Over 4,200 confirmed cases of foodborne disease in 2015 • HIV infections decreased by 31% from 2005 to 2014 • In 2015, hepatitis C case rates were 26 and 10 times higher, respectively, among White non-Hispanics compared to Asian non-Hispanics and Black non-Hispanics • In 2016, 190 cases of TB were reported in Massachusetts • Tickborne babesiosis increased 15% from 2015 to 2016 • Influenza and pneumonia ranked in the top ten leading causes of death among Massachusetts residents in 2014 100 | Massachusetts State Health Assessment Overview Infectious diseases have been causing human illness and death since the dawn of human existence. The effective prevention and control of these diseases is one of the major reasons for increases in life expectancy. In 1701, Massachusetts passed legislation requiring the isolation of the sick “for better preventing the spread of infection.”190 Since then, Massachusetts has led the nation in infection prevention and control. For example, Massachusetts was the only state to achieve a score of 10 out of 10 in Health Security Ranking which includes reducing healthcare-associated infections (HAIs), biosafety training in public health laboratories, public health funding commitment, national health security preparedness, public health accreditation, flu vaccination rates, climate change readiness,afety as well as a biosafety professional on staff and emergency health care access. -

Fever, Malaise and Arthralgia: Brucellosis Or Salmonellosis in The
Original Investigation / Özgün Araştırma DOI: 10.5578/ced.202045 • J Pediatr Inf 2020;14(3):e106-e110 Fever, Malaise and Arthralgia: Brucellosis or Salmonellosis in the Differential Diagnosis in an Endemic Area Ateş, Halsizlik ve Artralji: Endemik Bir Bölgede Ayırıcı Tanıda Bruselloz ve Salmonelloz Başak Yıldız Atikan1(İD), Gülhadiye Avcu1(İD) 1 Clinic of Pediatric Infectious Diseases, Balikesir Ataturk City Hospital, Balikesir, Turkey Cite this article as: Yıldız Atikan B, Avcu G. Fever, malaise and arthralgia: brucellosis or salmonellosis in the differential diagnosis in an endemic area. J Pediatr Inf 2020;14(3):e106-e110. Abstract Öz Objective: Brucellosis and salmonellosis are both infectious, zoonotic Giriş: Bruselloz ve salmonelloz ülkemizde endemik olarak görülen en- and endemic diseases in Turkey. In this study, we aimed to report a group feksiyöz ve zoonotik hastalıklardır. Bu çalışmada hastanemize ateş, hal- of pediatric patients admitted to the hospital with fever, malaise and ar- sizlik ve eklem ağrısı yakınması ile başvuran ve bu iki hastalık açısından thralgia and diagnosed with either of the diseases. tetkik edilerek biri ile tanı almış pediatrik olgular geriye dönük olarak Material and Methods: We retrospectively analysed hospital records for incelenmesi amaçlanmıştır. gender, age, consumption of raw milk products, laboratory results, organ Gereç ve Yöntemler: Hastaların yaş, cinsiyet, çiğ süt ve süt ürünü tü- involvement, treatment choices and course of the disease. ketim öyküleri, klinik ve laboratuvar bulguları, organ tutuluşları, tedavi Results: Out of a total of 36 children, 30 were diagnosed with brucellosis uygulamaları ve prognozları retrospektif olarak değerlendirilerek sunul- and 6 with salmonellosis in two years. A total of 20 patients of 30 cases muştur. -

2017 Summary
KENT COUNTY HEALTH DEPARTMENT EPI FOCUS 2017 Communicable Disease Summary Contents Introduction What are reportable diseases? ................................................................................................................................................... 2 Michigan Disease Surveillance System (MDSS) ........................................................................................................................... 2 Gastrointestinal illnesses Campylobacter ............................................................................................................................................................................ 4 Shigellosis ....................................................................................................................................................................................5 Giardiasis .....................................................................................................................................................................................5 Salmonellosis .............................................................................................................................................................................. 6 Sexually Transmitted Infections HIV/AIDS .................................................................................................................................................................................... 7 Chlamydia ................................................................................................................................................................................... -
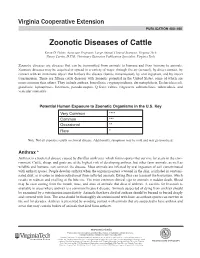
Zoonotic Diseases of Cattle Kevin D
PUBLICATION 400-460 Zoonotic Diseases of Cattle Kevin D. Pelzer, Associate Professor, Large Animal Clinical Sciences, Virginia Tech Nancy Currin, D.V.M., Veterinary Extension Publication Specialist, Virginia Tech Zoonotic diseases are diseases that can be transmitted from animals to humans and from humans to animals. Zoonotic diseases may be acquired or spread in a variety of ways: through the air (aerosol), by direct contact, by contact with an inanimate object that harbors the disease (fomite transmission), by oral ingestion, and by insect transmission. There are fifteen cattle diseases with zoonotic potential in the United States, some of which are more common than others. They include anthrax, brucellosis, cryptosporidiosis, dermatophilosis, Escherichia coli, giardiasis, leptospirosis, listeriosis, pseudocowpox, Q fever, rabies, ringworm, salmonellosis, tuberculosis, and vesicular stomatitis. Potential Human Exposure to Zoonotic Organisms in the U.S. Key Very Common **** Common *** Occasional ** Rare * Note: Not all exposure results in clinical disease. Additionally, symptoms may be mild and may go unnoticed. Anthrax * Anthrax is a bacterial disease caused by Bacillus anthracis, which forms spores that survive for years in the envi- ronment. Cattle, sheep, and goats are at the highest risk of developing anthrax, but other farm animals, as well as wildlife and humans, can contract the disease. Most animals are infected by oral ingestion of soil contaminated with anthrax spores. People develop anthrax when the organism enters a wound in the skin, is inhaled in contami- nated dust, or is eaten in undercooked meat from infected animals. Biting flies can transmit the bacterium, which results in redness and swelling at the bite site. -

Salmonellosis Fact Sheet
Salmonellosis Fact Sheet 1. What is salmonellosis? Salmonellosis is an infection caused by salmonella bacteria that generally affects the intestinal tract, and occasionally the bloodstream and other organs. It is one of the more common causes of bacterial gastroenteritis (diarrhea and/or vomiting) with approximately 2,000 cases reported annually in Pennsylvania and 40,000 cases reported annually in the United States. Since many milder cases are not diagnosed or reported, the actual number of infections may be thirty or more times greater. Most cases occur in the summer months, and are seen as single cases, clusters or outbreaks. 2. Who gets salmonellosis? - Any person can become infected with salmonella, but it is diagnosed more often in infants and children. The rate of diagnosed infections in children less than five years old is higher than the rate in all other persons. Young children, the elderly, and immunocompromised persons are the most likely to have severe disease. Approximately 400 persons die each year in the United States from acute salmonellosis. 3. How do people become infected by salmonella? People generally become infected by salmonella by either eating or drinking contaminated food or water, by contact with infected people or animals, or through contact with contaminated environmental sources. Salmonella bacteria live in the intestinal tracts of humans and other animals, including birds. These bacteria are usually transmitted to humans by eating foods contaminated with feces. Contaminated foods usually look and smell normal. Contaminated foods are often of animal origin, such as beef, poultry, milk, or eggs, but any food, including vegetables, may become contaminated. -

Zoonotic Diseases
ZOONOTIC DISEASES Jim Kazmierczak, State Public Health Veterinarian Wisconsin Division of Public Health, January 2014 At a Glance • Importance of zoonoses • Pets & immunocompromised persons • Therapy animal considerations • Brucella canis • Reptile-associated salmonellosis • Cat scratch disease • Lymphocytic Choriomeningitis Virus Veterinarian’s Oath “Being admitted to the profession of veterinary medicine, I solemnly swear to use my scientific knowledge and skills for the benefit of society through the protection of animal health, the relief of animal suffering, the conservation of livestock resources, the promotion of public health and the advancement of medical knowledge….” Why Zoonoses ? . Approx. 50% of known human pathogens are zoonotic . Of the 156 pathogens associated with emerging diseases, 73% are zoonotic (WHO data) . Pathogens often recognized in animals before being noted in humans . Most weaponizable pathogens are zoonotic agents More Recent Concerns . Xenotransplantation – live cells, tissues, or organs from a nonhuman animal source . Increased import/ownership of exotic pets More Recent Concerns (2) . Increasing use of therapy animals – contact with frail patients . More persons living who are immunodeficient Increasing numbers of immune compromised persons In USA: 3.6% of population is immunocompromised from HIV, cancer, and organ transplants. ~ 40–50% of households with an HIV+ person have pets or: “So much for One Health” • 71% of MDs never or almost never ask HIV/AIDS patients about pet ownership and animal contact