Cannabinoid Antagonist Drug Discrimination in Nonhuman Primates
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

S41467-020-19780-Z.Pdf
ARTICLE https://doi.org/10.1038/s41467-020-19780-z OPEN Endocannabinoid signaling regulates the reinforcing and psychostimulant effects of ketamine in mice Wei Xu1,3, Hongchun Li1,3, Liang Wang1, Jiamei Zhang1, Chunqi Liu1, Xuemei Wan1, Xiaochong Liu1, Yiming Hu1, ✉ Qiyao Fang1, Yuanyuan Xiao1, Qian Bu1, Hongbo Wang2, Jingwei Tian2, Yinglan Zhao1 & Xiaobo Cen 1 The abuse potential of ketamine limits its clinical application, but the precise mechanism remains largely unclear. Here we discovered that ketamine significantly remodels the 1234567890():,; endocannabinoid-related lipidome and activates 2-arachidonoylglycerol (2-AG) signaling in the dorsal striatum (caudate nucleus and putamen, CPu) of mice. Elevated 2-AG in the CPu is essential for the psychostimulant and reinforcing effects of ketamine, whereas blockade of the cannabinoid CB1 receptor, a predominant 2-AG receptor, attenuates ketamine-induced remodeling of neuronal dendrite structure and neurobehaviors. Ketamine represses the transcription of the monoacylglycerol lipase (MAGL) gene by promoting the expression of PRDM5, a negative transcription factor of the MAGL gene, leading to increased 2-AG pro- duction. Genetic overexpression of MAGL or silencing of PRDM5 expression in the CPu robustly reduces 2-AG production and ketamine effects. Collectively, endocannabinoid signaling plays a critical role in mediating the psychostimulant and reinforcing properties of ketamine. 1 National Chengdu Center for Safety Evaluation of Drugs, State Key Laboratory of Biotherapy/Collaborative Innovation Center for Biotherapy, West China Hospital, Sichuan University, 610041 Chengdu, People’s Republic of China. 2 Ministry of Education, Collaborative Innovation Center of Advanced Drug Delivery System and Biotech Drugs in Universities of Shandong, Yantai University, 264005 Yantai, People’s Republic of China. -

British Journal of Nutrition (2009), 101, 457–464 Doi:10.1017/S0007114508024008 Q the Authors 2008
Downloaded from https://www.cambridge.org/core British Journal of Nutrition (2009), 101, 457–464 doi:10.1017/S0007114508024008 q The Authors 2008 Administration of a dietary supplement (N-oleyl-phosphatidylethanolamine . IP address: and epigallocatechin-3-gallate formula) enhances compliance with diet in healthy overweight subjects: a randomized controlled trial 170.106.35.93 Mariangela Rondanelli1,2*, Annalisa Opizzi1,2, Sebastiano Bruno Solerte3, Rosita Trotti4, Catherine Klersy5 6 , on and Roberta Cazzola 29 Sep 2021 at 01:44:33 1Section of Human Nutrition and Dietetics, Department of Applied Health Sciences, Faculty of Medicine, University of Pavia, Pavia, Italy 2Endocrinology and Nutrition Unit, ASP, II.AA.RR, University of Pavia, ‘Istituto Santa Margherita’, Pavia, Italy 3Department of Internal Medicine, Geriatrics and Gerontologic Clinic, University of Pavia, ‘Istituto Santa Margherita’, Pavia, Italy 4Laboratory of Biochemical Chemistry, Neurological Institute ‘C. Mondino’, IRCCS, Pavia, Italy , subject to the Cambridge Core terms of use, available at 5Service of Biometry and Clinical Epidemiology, Fondazione IRCCS ‘Policlinico San Matteo’, Pavia, Italy 6Department of Preclinical Sciences ‘LITA Vialba’, Faculty of Medicine, University of Milan, Milan, Italy (Received 21 February 2008 – Revised 29 April 2008 – Accepted 20 May 2008 – First published online 1 July 2008) Many studies have found that N-oleyl-ethanolamine (NOE), a metabolite of N-oleyl-phosphatidylethanolamine (NOPE), and epigallocatechin-3- gallate (EGCG) inhibit food intake. The main aim of this study was to evaluate the efficacy of 2 months of administration of an oily NOPE– EGCG complex (85 mg NOPE and 50 mg EGCG per capsule) and its effect on compliance with diet in healthy, overweight people. -

The Selective Reversible FAAH Inhibitor, SSR411298, Restores The
www.nature.com/scientificreports OPEN The selective reversible FAAH inhibitor, SSR411298, restores the development of maladaptive Received: 22 September 2017 Accepted: 26 January 2018 behaviors to acute and chronic Published: xx xx xxxx stress in rodents Guy Griebel1, Jeanne Stemmelin2, Mati Lopez-Grancha3, Valérie Fauchey3, Franck Slowinski4, Philippe Pichat5, Gihad Dargazanli4, Ahmed Abouabdellah4, Caroline Cohen6 & Olivier E. Bergis7 Enhancing endogenous cannabinoid (eCB) signaling has been considered as a potential strategy for the treatment of stress-related conditions. Fatty acid amide hydrolase (FAAH) represents the primary degradation enzyme of the eCB anandamide (AEA), oleoylethanolamide (OEA) and palmitoylethanolamide (PEA). This study describes a potent reversible FAAH inhibitor, SSR411298. The drug acts as a selective inhibitor of FAAH, which potently increases hippocampal levels of AEA, OEA and PEA in mice. Despite elevating eCB levels, SSR411298 did not mimic the interoceptive state or produce the behavioral side-efects (memory defcit and motor impairment) evoked by direct-acting cannabinoids. When SSR411298 was tested in models of anxiety, it only exerted clear anxiolytic-like efects under highly aversive conditions following exposure to a traumatic event, such as in the mouse defense test battery and social defeat procedure. Results from experiments in models of depression showed that SSR411298 produced robust antidepressant-like activity in the rat forced-swimming test and in the mouse chronic mild stress model, restoring notably the development of inadequate coping responses to chronic stress. This preclinical profle positions SSR411298 as a promising drug candidate to treat diseases such as post-traumatic stress disorder, which involves the development of maladaptive behaviors. Te endocannabinoid (eCB) system is formed by two G protein-coupled receptors, CB1 and CB2, and their main transmitters, N-arachidonoylethanolamine (anandamide; AEA) and 2-arachidonoyglycerol (2-AG)1. -

Bioactivation Pathways of the Cb1r Antagonist Rimonabant
DMD Fast Forward. Published on July 6, 2011 as DOI: 10.1124/dmd.111.039412 DMDThis Fast article Forward. has not been Published copyedited and on formatted. July 6, The2011 final as version doi:10.1124/dmd.111.039412 may differ from this version. DMD #39412 Bioactivation Pathways of the CB1r Antagonist Rimonabant Downloaded from Moa Andresen Bergström, Emre M. Isin, Neal Castagnoli Jr., and Claire E. Milne dmd.aspetjournals.org CVGI iMED DMPK, AstraZeneca R&D Mölndal, Sweden (M.A.B., E.M.I., C.E.M.); Department of Chemistry, Virginia Tech, and Virginia College of Osteopathic Medicine, Blacksburg, VA 24061 (N.C.) at ASPET Journals on October 1, 2021 1 Copyright 2011 by the American Society for Pharmacology and Experimental Therapeutics. DMD Fast Forward. Published on July 6, 2011 as DOI: 10.1124/dmd.111.039412 This article has not been copyedited and formatted. The final version may differ from this version. DMD #39412 Running Title: Bioactivation Pathways of the CB1r Antagonist Rimonabant Corresponding Author: Dr. Moa Andresen Bergström, CVGI iMED DMPK, AstraZeneca R&D Mölndal, SE-431 83 Mölndal, Sweden. Tel.: +46317762551, Fax.: +46317763760, E-mail: [email protected]. Number of Text Pages: 18 Downloaded from Number of Tables: 2 Number of Figures: 6 dmd.aspetjournals.org Number of Schemes: 3 Number of References: 40 Number of Words in Abstract: 227 at ASPET Journals on October 1, 2021 Number of Words in Introduction: 604 Number of Words in Discussion: 1500 List of Nonstandard Abbreviations: ADRs, adverse drug reactions; BFC, 7-benzyloxy-4- trifluoromethylcoumarin; CYP, cytochrome P450; HFC, 7-hydroxy-4- (trifluoromethyl)coumarin; HLMs, human liver microsomes; IADRs, idiosyncratic adverse drug reactions; KCN, potassium cyanide; LC, liquid chromatography; LSC, liquid scintillation counting; MS, mass spectrometry; RAD, radiochemical detection; RLMs, rat liver microsomes; TDI, time-dependent inhibition 2 DMD Fast Forward. -

Toxicology Solutions
Toxicology Solutions Contents Biochip Array Technology Overview 04 Benefits 05 Testing Process 06 The Evidence Series 08 Evidence+ 10 Evidence 12 Evidence Investigator 14 Evidence MultiSTAT 16 Matrices 18 Test Menu 20 Customisable Test Menu 24 Catalogue Numbers 26 ELISA 28 Cross Reactivity 30 Technical Support 37 Ordering Information 38 Introduction Randox Toxicology aim to minimise laboratory workflow constraints whilst maximising the scope of quality drug detection. We are the primary manufacturer of Biochip Array Technology, ELISAs, and automated systems for forensic, clinical and workplace toxicology. Biochip Array Technology Moving away from traditional single analyte assays, Biochip Array Technology (BAT) boasts cutting-edge multiplex testing capabilities providing rapid and accurate drug detection from a single sample. Based on ELISA principles, the Biochip is a solid state device with discrete test regions onto which antibodies, specific to different drug compounds, are immobilised and stabilised. Competitive chemiluminescent immunoassays are then employed, offering a highly sensitive screen. Designed to work across a wide variety of matrices, this revolutionary multi- analyte testing platform allows toxicologists to achieve a complete immunoassay profile from the initial screening phase. Offering the most advanced screening technology on the market, Randox Toxicology has transformed the landscape of drugs of abuse (DoA) testing. Our unrivalled toxicology test menu is capable of detecting over 500 drugs and drug metabolites. 4 Benefits Simultaneous detection Multiplex testing facilitates simultaneous screening of various drugs and drug metabolites from a single sample. Accurate testing Biochip Array Technology has a proven high standard of accurate test results with CVs typically <10%. Small sample volume As little as 6μl of sample produces a complete immunoassay profile, leaving more for confirmatory testing. -

Potential Cannabis Antagonists for Marijuana Intoxication
Central Journal of Pharmacology & Clinical Toxicology Bringing Excellence in Open Access Review Article *Corresponding author Matthew Kagan, M.D., Cedars-Sinai Medical Center, 8730 Alden Drive, Los Angeles, CA 90048, USA, Tel: 310- Potential Cannabis Antagonists 423-3465; Fax: 310.423.8397; Email: Matthew.Kagan@ cshs.org Submitted: 11 October 2018 for Marijuana Intoxication Accepted: 23 October 2018 William W. Ishak, Jonathan Dang, Steven Clevenger, Shaina Published: 25 October 2018 Ganjian, Samantha Cohen, and Matthew Kagan* ISSN: 2333-7079 Cedars-Sinai Medical Center, USA Copyright © 2018 Kagan et al. Abstract OPEN ACCESS Keywords Cannabis use is on the rise leading to the need to address the medical, psychosocial, • Cannabis and economic effects of cannabis intoxication. While effective agents have not yet been • Cannabinoids implemented for the treatment of acute marijuana intoxication, a number of compounds • Antagonist continue to hold promise for treatment of cannabinoid intoxication. Potential therapeutic • Marijuana agents are reviewed with advantages and side effects. Three agents appear to merit • Intoxication further inquiry; most notably Cannabidiol with some evidence of antipsychotic activity • THC and in addition Virodhamine and Tetrahydrocannabivarin with a similar mixed receptor profile. Given the results of this research, continued development of agents acting on cannabinoid receptors with and without peripheral selectivity may lead to an effective treatment for acute cannabinoid intoxication. Much work still remains to develop strategies that will interrupt and reverse the effects of acute marijuana intoxication. ABBREVIATIONS Therapeutic uses of cannabis include chronic pain, loss of appetite, spasticity, and chemotherapy-associated nausea and CBD: Cannabidiol; CBG: Cannabigerol; THCV: vomiting [8]. Recreational cannabis use is on the rise with more Tetrahydrocannabivarin; THC: Tetrahydrocannabinol states approving its use and it is viewed as no different from INTRODUCTION recreational use of alcohol or tobacco [9]. -

NIDA - Director's Report - May 2004
NIDA - Director's Report - May 2004 Home > Publications > Director's Reports Director's Report to the National Advisory Council on Drug Abuse - May, 2004 Index Report Index Research Findings Report for February, 2004 Basic Research Report for Behavioral Research September, 2003 Treatment Research and Development Report for May, Research on AIDS and Other Medical Consequences of Drug 2003 Abuse - AIDS Research Report for February, Research on AIDS and Other Medical Consequences of Drug 2003 Abuse - Non-AIDS Medical Consequences of Drug Abuse Report for Epidemiology and Etiology Research September, 2002 Prevention Research Report for May, 2002 Services Research Report for February, Intramural Research 2002 Program Activities Report for September, 2001 Extramural Policy and Review Activities Report for May, 2001 Congressional Affairs Report for February, 2001 International Activities Report for September, 2000 Meetings and Conferences Report for May, 2000 Media and Education Activities Report for February, 2000 Planned Meetings Report for September, 1999 Publications Report for May, 1999 Staff Highlights Report for February, 1999 Grantee Honors Report for September, 1998 Report for May, 1998 Report for February, 1998 Report for September, 1997 Report for May, 1997 Report for February, 1997 https://archives.drugabuse.gov/DirReports/DirRep504/Default.html[11/17/16, 10:22:07 PM] NIDA - Director's Report - May 2004 Report from September, 1996 Report from May, 1996 Report from February, 1996 Report from September, 1995 Report from May, 1995 Report from February, 1995 NACDA Legislation Archive Home | Accessibility | Privacy | FOIA (NIH) | Current NIDA Home Page The National Institute on Drug Abuse (NIDA) is part of the National Institutes of Health (NIH) , a component of the U.S. -
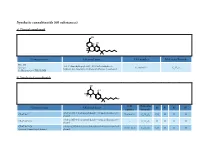
Synthetic Cannabinoids (60 Substances) A) Classical Cannabinoid
Synthetic cannabinoids (60 substances) a) Classical cannabinoid OH H OH H O Common name Chemical name CAS number Molecular Formula HU-210 3-(1,1’-dimethylheptyl)-6aR,7,10,10aR-tetrahydro-1- Synonym: 112830-95-2 C H O hydroxy-6,6-dimethyl-6H-dibenzo[b,d]pyran-9-methanol 25 38 3 11-Hydroxy-Δ-8-THC-DMH b) Nonclassical cannabinoids OH OH R2 R3 R4 R1 CAS Molecular Common name Chemical name R1 R2 R3 R4 number Formula rel-2[(1 S,3 R)-3- hydroxycyclohexyl]- 5- (2- methyloctan- 2- yl) CP-47,497 70434-82-1 C H O CH H H H phenol 21 34 2 3 rel-2[(1 S,3 R)-3- hydroxycyclohexyl]- 5- (2- methylheptan- 2- yl) CP-47,497-C6 - C H O H H H H phenol 20 32 2 CP-47,497-C8 rel-2- [(1 S,3 R)-3- hydroxycyclohexyl]- 5- (2- methylnonan- 2- yl) 70434-92-3 C H O C H H H H Synonym: Cannabicyclohexanol phenol 22 36 2 2 5 CAS Molecular Common name Chemical name R1 R2 R3 R4 number Formula rel-2[(1 S,3 R)-3- hydroxycyclohexyl]- 5- (2- methyldecan- 2- yl) CP-47,497-C9 - C H O C H H H H phenol 23 38 2 3 7 rel-2- ((1 R,2 R,5 R)-5- hydroxy- 2- (3- hydroxypropyl)cyclohexyl)- 3-hydroxy CP-55,940 83003-12-7 C H O CH H H 5-(2- methyloctan- 2- yl)phenol 24 40 3 3 propyl rel-2- [(1 S,3 R)-3- hydroxy-5,5-dimethylcyclohexyl]- 5- (2- Dimethyl CP-47,497-C8 - C H O C H CH CH H methylnonan-2- yl)phenol 24 40 2 2 5 3 3 c) Aminoalkylindoles i) Naphthoylindoles 1' R R3' R2' O N CAS Molecular Common name Chemical name R1’ R2’ R3’ number Formula [1-[(1- methyl- 2- piperidinyl)methyl]- 1 H-indol- 3- yl]- 1- 1-methyl-2- AM-1220 137642-54-7 C H N O H H naphthalenyl-methanone 26 26 2 piperidinyl -

Antiobesity and Anti-Inflammation Effects of Hakka Stir-Fried Tea Of
food & nutrition research ORIGINAL ARTICLE Antiobesity and anti-inflammation effects of Hakka stir-fried tea of different storage years on high-fat diet-induced obese mice model via activating the AMPK/ACC/CPT1 pathway Qiuhua Li1, Xingfei Lai1, Lingli Sun1, Junxi Cao1, Caijin Ling1, Wenji Zhang1, Limin Xiang1, Ruohong Chen1, Dongli Li2* and Shili Sun1* 1Tea Research Institute, Guangdong Academy of Agricultural Sciences/Guangdong Provincial Key Laboratory of Tea Plant Resources Innovation & Utilization, Guangzhou, China; 2School of Biotechnology and Health Sciences, Wuyi University, Jiangmen, China Popular scientific summary • We confirmed that HT treatment significantly reduced body weight and fat accumulation in major organs in high-fat diet-induced obese mice. • The effects of HT appear to be mediated by the activation of AMPK/ACC/CPT-1 pathway and further inhibiting lipogenesis. • Our findings suggest that HT may be used as a potential dietary strategy for preventing obesity and related metabolic disorder diseases. Abstract Background: As a typical representative of metabolic syndrome, obesity is also one of the extremely danger- ous factors of cardiovascular diseases. Thus, the prevention and treatment of obesity has gradually become a global campaign. There have been many reports that green tea is effective in preventing obesity, but as a kind of green tea with regional characteristics, there have been no reports that Hakka stir-fried tea (HT) of different storage years has a weight loss effect. Aims: The aim was to investigate the effect of HT in diet-induced obese mice. Methods: The mice were divided into five groups as follows: the control group received normal diet; the obese model group received high-fat diet; and HT2003, HT2008, and HT2015 groups, after the induction of obesity via a high-fat diet, received HT of different storage years treatment for 6 weeks, respectively. -

Grunddokument 2
The cellular processing of the endocannabinoid anandamide and its pharmacological manipulation Lina Thors Department of Pharmacology and Clinical Neuroscience SE-901 87 Umeå, Sweden Umeå 2009 1 Copyright©Lina Thors ISBN: 978-91-7264-732-9 ISSN: 0346-6612 Printed by: Print & Media Umeå, Sweden 2009 2 Abstract Anandamide (arachidonoyl ethanolamide, AEA) and 2-arachidonoyl glycerol (2-AG) exert most of their actions by binding to cannabinoid receptors. The effects of the endocannabinoids are short-lived due to rapid cellular accumulation and metabolism, for AEA, primarily by the enzymes fatty acid amide hydrolase (FAAH). This has led to the hypothesis that by inhibition of the cellular processing of AEA, beneficial effects in conditions such as pain and inflammation can be enhanced. The overall aim of the present thesis has been to examine the mechanisms involved in the cellular processing of AEA and how they can be influenced pharmacologically by both synthetic natural compounds. Liposomes, artificial membranes, were used in paper I to study the membrane retention of AEA. The AEA retention mimicked the early properties of AEA accumulation, such as temperature- dependency and saturability. In paper II, FAAH was blocked by a selective inhibitor, URB597, and reduced the accumulation of AEA into RBL2H3 basophilic leukaemia cells by approximately half. Treating intact cells with the tyrosine kinase inhibitor genistein, an isoflavone found in soy plants and known to disrupt caveolae-related endocytosis, reduced the AEA accumulation by half, but in combination with URB597 no further decrease was seen. Further on, the effects of genistein upon uptake were secondary to inhibition of FAAH. -

The Endocannabinoid System and Psychiatric Disorders
Experimental Neurology 224 (2010) 3–14 Contents lists available at ScienceDirect Experimental Neurology journal homepage: www.elsevier.com/locate/yexnr Review The endocannabinoid system and psychiatric disorders Daniela Parolaro a,b,⁎, Natalia Realini a, Daniela Vigano a,b, Cinzia Guidali a, Tiziana Rubino a a DBSF and Neuroscience Center, University of Insubria, Via A. da Giussano 10, 21052 Busto Arsizio (Varese), Italy b Zardi-Gori Foundation, via P.Cossa 1, Milan, Italy article info abstract Available online 29 March 2010 The present review summarizes the latest information on the role and the pharmacological modulation of the endocannabinoid system in mood disorders and its potential implication in psychotic disorders such as Keywords: schizophrenia. Endocannabinoid system Reduced functionality might be considered a predisposing factor for major depression, so boosting Depression endocannabinoid tone might be a useful alternative therapeutic approach for depressive disorders. The Anxiety picture regarding endocannabinoids and anxiety is more complicated since either too much or too little Schizophrenia anandamide can lead to anxiety states. However, a small rise in its level in specific brain areas might be beneficial for the response to a stressful situation and therefore to tone down anxiety. This effect might be achieved with low doses of cannabinoid indirect agonists, such as blockers of the degradative pathway (i.e. FAAH) or re-uptake inhibitors. Moreover several lines of experimental and clinical evidence point to a dysregulation of the endocanna- binoid system in schizophrenia. The high anandamide levels found in schizophrenic patients, negatively correlated with psychotic symptoms, point to a protective role, whereas the role of 2-arachidonoyl glycerol is still unclear. -

NIH Public Access Author Manuscript Neuropharmacology
NIH Public Access Author Manuscript Neuropharmacology. Author manuscript; available in PMC 2009 January 1. NIH-PA Author ManuscriptPublished NIH-PA Author Manuscript in final edited NIH-PA Author Manuscript form as: Neuropharmacology. 2008 January ; 54(1): 129±140. The endogenous cannabinoid anandamide has effects on motivation and anxiety that are revealed by fatty acid amide hydrolase (FAAH) inhibition Maria Schermaa,b, Julie Medaliea, Walter Frattab, Subramanian K. Vadivelc, Alexandros Makriyannisc, Daniele Piomellid, Eva Mikicse, Jozsef Hallere, Sevil Yasarf, Gianluigi Tandag, and Steven R. Goldberga,* aPreclinical Pharmacology Section, Behavioral Neuroscience Research Branch, Intramural Research Program, National Institute on Drug Abuse, National Institutes of Health, Department of Health and Human Services, Baltimore, MD 21224, USA bB.B. Brodie Department of Neuroscience, University of Cagliari, Italy cCenter for Drug Discovery, Northeastern University, Boston, MA, USA dDepartment of Pharmacology, University of California, Irvine, USA eInstitute of Experimental Medicine, Hungarian Academy of Sciences, Budapest, Hungary fDivision of Geriatric Medicine and Gerontology, Department of Medicine, Johns Hopkins University School of Medicine, Baltimore, MD 21224, USA gPsychobiology Section, Medications Discovery Research Branch, Intramural Research Program, National Institute on Drug Abuse, National Institutes of Health, Department of Health and Human Services, Baltimore, MD 21224, USA Summary Converging evidence suggests that the endocannabinoid system is an important constituent of neuronal substrates involved in brain reward processes and emotional responses to stress. Here, we evaluated motivational effects of intravenously administered anandamide, an endogenous ligand for cannabinoid-CB1 receptors, in Sprague-Dawley rats, using a place-conditioning procedure in which drugs abused by humans generally produce conditioned place preferences (reward). Anandamide (0.03 to 3mg/kg intravenous) produced neither conditioned place preferences nor aversions.