Physicochemical Properties of Lecithin-Based Nanoemulsions Obtained by Spontaneous Emulsification Or High-Pressure Homogenization
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nuclear Magnetic Resonance Spin Lattice Relaxation in Lecithin Reverse Micelles
Biosci., Vol. 4, Number 4, December 1982, pp. 449-454. © Printed in India. 31 [ P] -Nuclear magnetic resonance spin lattice relaxation in lecithin reverse micelles V. V. KUMAR, P. T. MANOHARAN and P. RAGHUNATHAN Department of Chemistry, Indian Institute of Technology, Kanpur 208 016 Regional Sophisticated Instrumentation Centre, Indian Institute of Technology, Madras 600 036 MS received 25 March 1982; revised 5 June 1982 31 Abstract. [ P] -Nuclear magnetic resonance (NMR) spin lattice relaxation times (T1) have been measured for lecithin-nonpolar solvent-water as a function of added water for three solvents, namely, benzene, carbon tetrachloride and cyclohexane. In benzene and carbon 31 tetrachloride systems, where spherical reverse micelles are formed, [ P]-NMR T1, values 31 increase linearly with added water. However, in cyclohexane, the trends in the [ P]-T1 values indicate very different micellisation processes. Even at the lowest concentration of added 31 water, the [ P]-T1 values in this solvent are substantially larger than the corresponding values in benzene and carbon tetrachloride, which is attributed to the intramolecular chlorine- phosphate interaction being the weakest in cyclohexane. At a higher water content of six 31 mols of water per mol of lecithin in cyclohexane solvent, the [ Ρ]-T1 values show a sharp decrease indicating a sudden change in the dynamics of the phosphate group, and this confirms the on set of 'reverse micelle-to-liquid crystalline' phase transition observed in this system by other spectroscopic and physical techniques. Keywords. [31P]-NMR; spin lattice relaxation; lecithin reverse micelles. Introduction There has been a rapid growth of interest in recent years in the study of phospholipid aggregates in nonpolar media since these aggregated structures often ‘model’ faithfully the nature of cell membranes. -

Extraction of Phospholipid-Rich Fractions from Egg Yolk And
Food and Chemical Toxicology 133 (2019) 110749 Contents lists available at ScienceDirect Food and Chemical Toxicology journal homepage: www.elsevier.com/locate/foodchemtox Extraction of phospholipid-rich fractions from egg yolk and development of T liposomes entrapping a dietary polyphenol with neuroactive potential João Bernardoa, Romeu A. Videiraa, Patrícia Valentãoa, Francisco Veigab,c, Paula B. Andradea,* a REQUIMTE/LAQV, Laboratório de Farmacognosia, Departamento de Química, Faculdade de Farmácia, Universidade do Porto, Rua de Jorge Viterbo Ferreira, no. 228, 4050-313, Porto, Portugal b REQUIMTE/LAQV, Group of Pharmaceutical Technology, Faculty of Pharmacy, University of Coimbra, Coimbra, Portugal c Department of Pharmaceutical Technology, Faculty of Pharmacy, University of Coimbra (FFUC), Pólo das Ciências da Saúde, Azinhaga de Santa Comba, 3000-548, Coimbra, Portugal ARTICLE INFO ABSTRACT Keywords: A new protocol to obtain egg yolk phospholipids in ethanol is presented. Rutin-phospholipids nanoliposomes Egg yolk were prepared and characterized. The procedure takes advantage of the different solubility of egg yolk lipids in Phospholipids ethanol and acetone at low temperature, to efficiently obtain a phospholipid-rich fraction of high purity degree. Liposomes The phospholipid content in the final fraction is 208.65 ± 26.46 μmol/g fresh egg yolk (16%), accounting for Flavonoids ca. 96% of the extract's dry weight. The phospholipid-rich fraction contains cholesterol (0.069–0.082 choles- Excitotoxicity terol/phospholipid molar ratio), and vestigial amounts of lutein and zeaxanthin (89.24 ± 9.76 and Neuroprotection 14.9 ± 2.16 ng/g of fresh egg yolk, respectively). Saturated fatty acids dominate the extracted phospholipids (50% of egg's total yolk phospholipids), the levels of monounsaturated ranging from 20 to 25%, and poly- unsaturated up to 35%. -
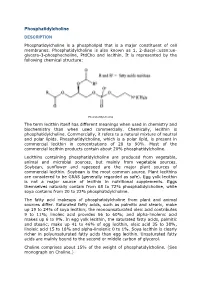
Phosphatidylcholine DESCRIPTION
Phosphatidylcholine DESCRIPTION Phosphatidylcholine is a phospholipid that is a major constituent of cell membranes. Phosphatidylcholine is also known as 1, 2-diacyl-:ussn:ue- glycero-3-phosphocholine, PtdCho and lecithin. It is represented by the following chemical structure: Phosphatidylcholine The term lecithin itself has different meanings when used in chemistry and biochemistry than when used commercially. Chemically, lecithin is phosphatidylcholine. Commercially, it refers to a natural mixture of neutral and polar lipids. Phosphatidylcholine, which is a polar lipid, is present in commercial lecithin in concentrations of 20 to 90%. Most of the commercial lecithin products contain about 20% phosphatidylcholine. Lecithins containing phosphatidylcholine are produced from vegetable, animal and microbial sources, but mainly from vegetable sources. Soybean, sunflower and rapeseed are the major plant sources of commercial lecithin. Soybean is the most common source. Plant lecithins are considered to be GRAS (generally regarded as safe). Egg yolk lecithin is not a major source of lecithin in nutritional supplements. Eggs themselves naturally contain from 68 to 72% phosphatidylcholine, while soya contains from 20 to 22% phosphatidylcholine. The fatty acid makeups of phosphatidylcholine from plant and animal sources differ. Saturated fatty acids, such as palmitic and stearic, make up 19 to 24% of soya lecithin; the monounsaturated oleic acid contributes 9 to 11%; linoleic acid provides 56 to 60%; and alpha-linolenic acid makes up 6 to 9%. In egg yolk lecithin, the saturated fatty acids, palmitic and stearic, make up 41 to 46% of egg lecithin, oleic acid 35 to 38%, linoleic acid 15 to 18% and alpha-linolenic 0 to 1%. -

The Effect of Papain Enzyme Dosage on the Modification of Egg- Yolk Lecithin Emulsifier Product Through Enzymatic Hydrolysis Reaction
International Journal of Technology (2018) 2: 380-389 ISSN 2086-9614 © IJTech 2018 THE EFFECT OF PAPAIN ENZYME DOSAGE ON THE MODIFICATION OF EGG- YOLK LECITHIN EMULSIFIER PRODUCT THROUGH ENZYMATIC HYDROLYSIS REACTION Setiadi1*, Nurul Hidayah 1 1Department of Chemical Engineering, Faculty of Engineering, Universitas Indonesia, Kampus UI Depok. Depok 16424, Indonesia (Received: December 2017 / Revised: January 2018 / Accepted: February 2018) ABSTRACT Lecithin is needed as a bioemulsifier product in stabilizing agents for the food, pharmaceutical and cosmetic industries due to its renewability and as it is environmentally friendly. In the food industry, most of the emulsifiers used are the oil-in-water (O/W) type. Lecithin can be seen as a promising emulsifier product because it is extracted from egg yolk and modified by enzymatic hydrolysis reaction using the papain enzyme. This modification will change the molecular structure of the compound, which makes lecithin more stable in the oil-in-water type of emulsion. This study aims to determine the optimum amount of papain enzyme used in the hydrolysis reaction to achieve the most stable O/W lecithin emulsion type. The results show that the breaking of a single fatty acid chain from the structure of lecithin can be demonstrated by FTIR instrumentation. The fatty acids detected from the lecithin structure are shown at wavenumber 1699.45 cm-1 (C=O), 1231.44 cm-1 (C-O), 1422.45 cm-1 (C-O-H), 1092.85 cm-1 (C-C), 665.89 -1 cm (CH2), and 3400.57 (-OH in carboxylate). Determination of the modified lecithin yield was made by several tests, namely a stability test, and tests for acid value, surface tension and zeta potential. -

Current Research in Phospholipids and Their Use in Drug Delivery
pharmaceutics Review Review TheThe PhospholipidPhospholipid ResearchResearch Center:Center: CurrentCurrent ResearchResearch inin PhospholipidsPhospholipids andand TheirTheir UseUse inin DrugDrug DeliveryDelivery SimonSimon DrescherDrescher ** andand Peter Peter van van Hoogevest Hoogevest PhospholipidPhospholipid ResearchResearch Center,Center, ImIm NeuenheimerNeuenheimerFeld Feld 515, 515, 69120 69120 Heidelberg, Heidelberg, Germany; Germany; [email protected] [email protected] * Correspondence: [email protected]; Tel.: +49-06221-588-83-60 * Correspondence: [email protected]; Tel.: +49-06221-588-83-60 Received:Received: 24 November 2020;2020; Accepted:Accepted: 14 December 2020; Published: 18 December 2020 Abstract:Abstract: ThisThis reviewreview summarizessummarizes thethe researchresearch onon phospholipidsphospholipids andand theirtheir useuse forfor drugdrug deliverydelivery relatedrelated toto thethe PhospholipidPhospholipid ResearchResearch CenterCenter HeidelbergHeidelberg (PRC).(PRC). TheThe focusfocus isis onon projectsprojects thatthat havehave beenbeen approvedapproved by by the the PRC PRC since since 2017 2017 and areand currently are currently still ongoing still ongoing or have recentlyor have been recently completed. been Thecompleted. different The projects different cover projects all facets cover of all phospholipid facets of phospholipid research, fromresearch, basic from to applied basic to research, applied includingresearch, including the -

Comparative Analysis of the Physiological Value of Lecithins Obtained from Different Types of Raw Materials
Elena Aleksandrovna Butina et al /J. Pharm. Sci. & Res. Vol. 9(12), 2017, 2493-2497 Comparative Analysis of the Physiological Value of Lecithins Obtained From Different Types of Raw Materials Elena Aleksandrovna Butina Evgeny Olegovich Gerasimenko Ivan Alekseevich Bugaets Irina Aleksandrovna Dubrovskaia Kuban State Technological University, Russia, 350072, Krasnodar, Moskovskaya Street, 2 Abstract The article provides comparative data describing the chemical composition and characteristics of the physiologically functional properties of the lecithins derived from plant and animal raw materials. The results of the clinical studies of the sunflower lecithin are presented, which show its hepatoprotective lipid-lowering and antioxidant properties. The quick and beneficial impact of the sunflower lecithin on lipid exchange, lipid peroxidation processes allows this type of lecithin to be seen as a promising tool for the prevention and comprehensive treatment of a range of diseases in the pathogenesis of which the above processes are being violated. Keywords: lecithin, phospholipids, chemical composition, physiologically functional properties. INTRODUCTION The main physiologically functional properties of lecithins Lecithin is the commercial name of the lipid complex with are determined by the group composition (type of a polar a preponderance of phospholipids that meets the group) and fatty acid composition (types of acyls of fatty established requirements [1]. acids), phospholipid molecules. These indicators also Phospholipids are the substances contained in cells of all identify the major differences of lecithins from different living organisms performing vital functions related to the types of raw materials. regulation of metabolic processes and protection of cell The chicken eggs and oilseed plants are the primary membranes. As part of the cellular membrane, sources of lecithin [1]. -

Oxidative Stability of Egg and Soy Lecithin As Affected by Transition Metal Ions and Ph in Emulsion Guang Wang Iowa State University
Food Science and Human Nutrition Publications Food Science and Human Nutrition 12-10-2008 Oxidative Stability of Egg and Soy Lecithin as Affected by Transition Metal Ions and pH in Emulsion Guang Wang Iowa State University Tong Wang Iowa State University, [email protected] Follow this and additional works at: http://lib.dr.iastate.edu/fshn_ag_pubs Part of the Food Chemistry Commons, and the Human and Clinical Nutrition Commons The ompc lete bibliographic information for this item can be found at http://lib.dr.iastate.edu/ fshn_ag_pubs/5. For information on how to cite this item, please visit http://lib.dr.iastate.edu/ howtocite.html. This Article is brought to you for free and open access by the Food Science and Human Nutrition at Iowa State University Digital Repository. It has been accepted for inclusion in Food Science and Human Nutrition Publications by an authorized administrator of Iowa State University Digital Repository. For more information, please contact [email protected]. Oxidative Stability of Egg and Soy Lecithin as Affected by Transition Metal Ions and pH in Emulsion Abstract Oxidative stability of egg and soy lecithin in emulsion was evaluated with two transition metal ions, cupric and ferric ion, at two concentration levels (50 and 500 μM). The effect of pH on lipid oxidation was also examined under these two concentrations for each ion. Egg lecithin (EL) had similar peroxide value (PV) development pattern as soy lecithin (SL) when treated with cupric ion under both acidic and neutral pH. Acidic pH of 3 accelerated oxidation of both EL and SL, especially under high concentration of copper. -

Fractionation of Egg Yolk Lípids Usíng Supercrítícal Carbon Díoxíde and Entrainer
Fractionation of Egg Yolk Lípids Usíng Supercrítícal Carbon Díoxíde and Entrainer by Lucia T. Labay subm¡ßed to tll Fdr*, {,!1ì)1, in Pañal Fulfillnent oÍ"¡or**l thc Requiremcnts for the Degree of MASTER oF SCIENCE Dcpøtnæu of Food Science Universit, of Manitoba Winnipeg , Maniøba, Canada @ April 1991 A.M.D,G. FR.A,CTIONATION OF EGG YOLK LIPIDS USING SUPERCRITICAL CARBON DIOXIDE AND ENTRAINER BY LUCIA T, LABAY A ¡hesis subntined to thc Faculty of Craduate Studies of the Univcrsily of M¿nitoba in partiel fullìllment of the requirenrerrls of the degrec of I'ÍASTER OF SCIENCE o r99r Permission has bccn granted to thc LIBRARY OF THE UNIVER- S¡TY OF MANITOBA to lend or scll copics of this rhesis. ro IhC NATIONA! LIBRARY OF CANADA tO fNJCfOfiIM this thesis and to lend o¡ scll copies oí th! ,ìlm, and UNIVERSITY MICROF¡LMS to publish an abstract of rhis thesis. The autho¡ ¡escrvcs other publication rights, and neither thc tlcsis nor cxtensivc extracts from it may be pnnlcC or other. wisc rcproduccd without the author's writtcn permission. Abstract The efficacy of egg yolk lipid fractionation with supercritical ca¡bon dioxide and enEainers was studied. The principal aims we¡e to study the feasibility of cholesterol removal and to determine the effects of extraction pressure and temperature and entrainer type and concentration upon extraction rate and lipid fractionation. Analysis for phosphatidylcholine (PC) was also performed. A Superpressure Supercritical Screening unit was used to extract freeze- dried egg yolk samples. Extraction pressure was varied from 15 to 36 MPa at 40"C and extraction temperature was varied from 40'C to 75'C at 36 MPa. -

Egg Lecithin Is Different from Soy Lecithin in the Phospholipids Profile
Iowa State University Animal Industry Report 2006 Soy Lecithin but Not Egg Lecithin Decreased the Plasma Cholesterol Concentration in Golden Syrian Hamsters A.S. Leaflet R2080 absorption in vitro and in vivo, which, in turn, might decrease the blood cholesterol concentration. Shu Zhang, graduate student of biochemistry; Tong Wang, Soy lecithin consists of three types of phospholipids associate professor of food science and human (PL): PC, phosphatidylethanolamine (PE), and nutrition; Donald Beitz, distinguished professor in phosphotidylinositol (PI), with similar amounts of each PL. animal science and biochemistry In contrast, egg lecithin contains PC and PE, with PC as the major component. The concentration of total unsaturated Summary and Implication fatty acids is much higher in soy lecithin than in egg Egg lecithin differs from soy lecithin in its lecithin. The objective of this study was to test whether egg phospholipid profile and fatty acid composition. The lecithin or soy lecithin decreased the plasma cholesterol current study was designed to test whether egg lecithin or concentration in hamsters used as a model for human. soy lecithin decreased the plasma cholesterol concentration in hamsters that are used as a model for humans. Male Materials and Methods golden Syrian hamsters were assigned randomly to eight Animals and diets. Male golden Syrian hamsters (10 dietary treatments lasting 4 weeks (n=10 per treatment) that weeks old, weighing ~100 g) were housed individually in contained 0.12% (wt/wt) of cholesterol and varied amount metabolic rodent cages. All animals were maintained in a of supplemental lipids. The diet groups were: control with temperature-controlled room (23°C) with a 12-hour/12- no supplemental lipid, 0.05%, 0.5%, and 5% (wt/wt) of egg hour light/dark cycle. -

Soy Lecithin but Not Egg Lecithin Decreased the Plasma Cholesterol Concentration in Golden Syrian Hamsters
Animal Industry Report Animal Industry Report AS 652 ASL R2080 2006 Soy Lecithin but Not Egg Lecithin Decreased the Plasma Cholesterol Concentration in Golden Syrian Hamsters Shu Zhang Iowa State University Tong Wang Iowa State University, [email protected] Donald C. Beitz Iowa State University Follow this and additional works at: https://lib.dr.iastate.edu/ans_air Part of the Agriculture Commons, and the Animal Sciences Commons Recommended Citation Zhang, Shu; Wang, Tong; and Beitz, Donald C. (2006) "Soy Lecithin but Not Egg Lecithin Decreased the Plasma Cholesterol Concentration in Golden Syrian Hamsters ," Animal Industry Report: AS 652, ASL R2080. DOI: https://doi.org/10.31274/ans_air-180814-128 Available at: https://lib.dr.iastate.edu/ans_air/vol652/iss1/21 This Companion Animal is brought to you for free and open access by the Animal Science Research Reports at Iowa State University Digital Repository. It has been accepted for inclusion in Animal Industry Report by an authorized editor of Iowa State University Digital Repository. For more information, please contact [email protected]. Iowa State University Animal Industry Report 2006 Soy Lecithin but Not Egg Lecithin Decreased the Plasma Cholesterol Concentration in Golden Syrian Hamsters A.S. Leaflet R2080 absorption in vitro and in vivo, which, in turn, might decrease the blood cholesterol concentration. Shu Zhang, graduate student of biochemistry; Tong Wang, Soy lecithin consists of three types of phospholipids associate professor of food science and human (PL): PC, phosphatidylethanolamine (PE), and nutrition; Donald Beitz, distinguished professor in phosphotidylinositol (PI), with similar amounts of each PL. animal science and biochemistry In contrast, egg lecithin contains PC and PE, with PC as the major component. -

Emulsova Emulsifier Benefits of Using Egg Lecithin
MARCH 12, 2018 EMULSOVA EMULSIFIER BENEFITS OF USING EGG LECITHIN ALEX HOLDCROFT, BSC., MM ECOVATEC SOLUTIONS INC. 31231 Wheel Ave., Abbotsford, B.C., CANADA, V2T6H1 Executive Summary Ecovatec’s revolutionary technology has unlocked the amazing potential of Egg Phospholipids. Phospholipids make up most of the cell membranes in our bodies, holding and sustaining the protein molecules through which cells communicate via hormones and neurotransmitters. Healthy membranes allow our cells to remain “fluid” and flexible and thereby function properly. Healthy membranes make for healthy cells. Phospholipid (PL) products are often called lecithin, especially when in concentrations of about 20-30% phospholipids. Lecithin is used as an emulsifier in food and cosmetic products and is usually derived from soybeans. Other egg-emulsification products are enzyme modified egg yolk or solvent-extracted egg PL. However, there are significant problems with these products. Ecovatec’s Emulsova™ (hydrolyzed phospholipids) is a superior emulsifier: it dissolves immediately in water, does not allow for oil and water separation in emulsions, only requires a small quantity (so doesn’t affect the taste of the product), and does not require any heat to incorporate it into a mixture. It is also made without any of the harsh solvents used by other egg PL manufacturers and unlike other enzyme modified egg products, our enzymes don’t increase the amount of carcinogenic lysophosphatidic acid (LPA). Also, unlike most soy lecithin, egg lecithin is GMO free. In addition to its emulsification properties, egg phospholipids have been shown to have the following health benefits: anti-inflammatory and cancer-fighting properties, improved cardiovascular health, neurological performance (including nerve function, learning, and memory), and liver function. -

Egg Yolk Lecithin Fractionation and Characterization
Iowa State University Capstones, Theses and Retrospective Theses and Dissertations Dissertations 1-1-2004 Egg yolk lecithin fractionation and characterization Luz Elena Palacios Iowa State University Follow this and additional works at: https://lib.dr.iastate.edu/rtd Recommended Citation Palacios, Luz Elena, "Egg yolk lecithin fractionation and characterization" (2004). Retrospective Theses and Dissertations. 20225. https://lib.dr.iastate.edu/rtd/20225 This Thesis is brought to you for free and open access by the Iowa State University Capstones, Theses and Dissertations at Iowa State University Digital Repository. It has been accepted for inclusion in Retrospective Theses and Dissertations by an authorized administrator of Iowa State University Digital Repository. For more information, please contact [email protected]. Egg yolk lecithin fractionation and characterization by Luz Elena Palacios A thesis submitted to the graduate faculty in partial fulfillment of the requirements for the degree of MASTER OF SCIENCE Major: Food Science and Technology Program of Study Committee: Tong Wang, Major Professor Earl Hammond Donald Beitz Iowa State University Ames, Iowa 2004 Copyright © Luz Elena Palacios, 2004. All rights reserved. 11 Graduate College Iowa State University This is to certify that the master's thesis of Luz Elena Palacios has met the thesis requirements oflowa State University Signatures have been redacted for privacy 111 TABLE OF CONTENTS CHAPTER 1. GENERAL INTRODUCTION 1 Literature Review 1 Thesis Organization 5 References 5 CHAPTER 2. EFFECT OF PROTEIN DENATURATION AND OIL ON EGG YOLK LECITHIN FRACTIONATION 9 Abstract 9 Introduction 10 Materials and Methods 11 Results and Discussion 14 References 19 CHAPTER 3. EGG YOLK LECITHIN FRACTIONATION AND CHARACTERIZATION 25 Abstract 25 Introduction 26 Materials and Methods 27 Results and Discussion 33 References 39 CHAPTER 5.