Clinical Pearls: Significant Drug Interactions
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

( 12 ) United States Patent
US010376507B2 (12 ) United States Patent (10 ) Patent No. : US 10 , 376 , 507 B2 Srinivasan et al. (45 ) Date of Patent: Aug. 13 , 2019 CRESEMBA® ( isavuconazonium sulfate ) , Highlights of Prescrib (54 ) METHOD OF TREATING A PATIENT WITH ing Information , Label ; Patient Information approved by the U . S . A CYP3A4 SUBSTRATE DRUG Food and Drug Administration ; Astellas Pharma US , Inc. ( Licensed from Basilea Pharmaceutics International Ltd . ) , Illinois, USA , Ini (71 ) Applicant: Bow River LLC , Corona Del Mar , CA tial U . S . Approval: 2015 , Revised Mar. 2015 , Reference ID : 3712237, ( US ) 28 pages . DIFLUCAN® ( fluconazole ), Label ; Patient Information , Reference ( 72 ) Inventors : Sundar Srinivasan , Corona Del Mar, ID : 3650838 , Roerig , Division of Pfizer Inc ., New York , NY, Revised Mar. 2013 , 35 pages. CA (US ) ; Christina Chow , Seattle , WA NIZORAL® (ketoconazole )Label ; Patient Information approved by (US ) the U . S . Food and Drug Administration , Reference ID : 3458324 , Copyright 2014 Janssen Pharmaceuticals, Inc . , New Jersey, USA , ( 73 ) Assignee : BOW RIVER LLC , Corona del Mar , Revised Feb . 2014 , 23 pages . NOXAFIL® (posaconazole ) , Highlights of Prescribing Informa CA (US ) tion , Label ; Patient Information approved by the U . S . Food and Drug Administration ; Copyright © 2006 , 2010 , 2013 , 2014 Merck ( * ) Notice : Subject to any disclaimer , the term of this Sharp & Dohme Corp . , a subsidiary of Merck & Co ., Inc ., New patent is extended or adjusted under 35 Jersey , USA , Revised Sep . 2016 , Reference ID : 3983525, 37 pages . U . S . C . 154 (b ) by 0 days. ORAVIG® (miconazole ) , Highlights of Prescribing Information , Label ; Patient Information approved by the U . S . Food and Drug Administration ; Copyright 2012 Praelia Pharmaceuticals , Inc . , North (21 ) Appl. -

Addyi Generic Name: Flibanserin Manufacturer
Brand Name: Addyi Generic Name: Flibanserin Manufacturer: Sprout Pharmaceuticals Drug Class: Central Nervous System Agent, Serotonin Agonist, Dopamine antagonist Uses: Labeled Uses: Indicated for the treatment of premenopausal women with acquired, generalized hypoactive sexual desire disorder (HSDD) as characterized by low sexual desire that causes marked distress or interpersonal difficulty and is NOT due to: A co-existing medical or psychiatric condition, problems within the relationship, or the effects of a medication or other drug substance. Unlabeled Uses: none. Mechanism of Action: The mechanism of action for flibanserin in the treatment of hypoactive sexual desire disorder is unknown. Flibanserin has high affinity for serotonin (5-hydroxytryptamine or 5-HT) 1A receptors, as an agonist, and 5-HT2A receptors, as an antagonist, and moderate affinity for 5- HT2B, 5-HT2C, and dopamine D4 receptors as an antagonist Pharmacokinetics: Absorption: Tmax 0.75 hours Vd 50L t ½ 11 hours Clearance Not reported Protein binding 98% (albumin) Bioavailability 33% Metabolism: Flibanserin is extensively metabolized primarily by CYP3A4 and, to a lesser extent, CYP2C19 to at least 35 metabolites, with most of the metabolites occurring in low concentrations in plasma. Elimination: Flibanserin is primarily excreted through the kidneys in to urine (44%) and feces (51%). Two metabolites could be characterized that showed plasma concentration similar to that achieved with flibanserin: 6,21-dihydroxy-flibanserin-6,21-disulfate and 6- hydroxy-flibanserin-6-sulfate. These two metabolites are inactive. Efficacy: Katz M, DeRogatis LR, Ackerman R, et al. Efficacy of flibanserin in women with hypoactive sexual desire disorder: results from the BEGONIA trial. J Sex Med. -

M2021: Pharmacogenetic Testing
Pharmacogenetic Testing Policy Number: AHS – M2021 – Pharmacogenetic Prior Policy Name and Number, as applicable: Testing • M2021 – Cytochrome P450 Initial Presentation Date: 06/16/2021 Revision Date: N/A I. Policy Description Pharmacogenetics is defined as the study of variability in drug response due to heredity (Nebert, 1999). Cytochrome (CYP) P450 enzymes are a class of enzymes essential in the synthesis and breakdown metabolism of various molecules and chemicals. Found primarily in the liver, these enzymes are also essential for the metabolism of many medications. CYP P450 are essential to produce many biochemical building blocks, such as cholesterol, fatty acids, and bile acids. Additional cytochrome P450 are involved in the metabolism of drugs, carcinogens, and internal substances, such as toxins formed within cells. Mutations in CYP P450 genes can result in the inability to properly metabolize medications and other substances, leading to increased levels of toxic substances in the body. Approximately 58 CYP genes are in humans (Bains, 2013; Tantisira & Weiss, 2019). Thiopurine methyltransferase (TPMT) is an enzyme that methylates azathioprine, mercaptopurine and thioguanine into active thioguanine nucleotide metabolites. Azathioprine and mercaptopurine are used for treatment of nonmalignant immunologic disorders; mercaptopurine is used for treatment of lymphoid malignancies; and thioguanine is used for treatment of myeloid leukemias (Relling et al., 2011). Dihydropyrimidine dehydrogenase (DPD), encoded by the gene DPYD, is a rate-limiting enzyme responsible for fluoropyrimidine catabolism. The fluoropyrimidines (5-fluorouracil and capecitabine) are drugs used in the treatment of solid tumors, such as colorectal, breast, and aerodigestive tract tumors (Amstutz et al., 2018). A variety of cell surface proteins, such as antigen-presenting molecules and other proteins, are encoded by the human leukocyte antigen genes (HLAs). -

(Flibanserin) (Flibanserin) Tablets
™ MEDICATION GUIDE addyi ADDYI™ (add-ee) (flibanserin) (flibanserin) Tablets Read this Medication Guide before you start taking ADDYI™ and each time you get a refill. There may be new information. This information does not take the place of talking to your doctor. What is the most important information I should know about ADDYI? Your risk of severe low blood pressure and fainting (loss of consciousness) is increased if you take ADDYI and: • drink alcohol. Do not drink alcohol if you take ADDYI. • take certain prescription medicines, over-the-counter medicines, or herbal supplements. Do not take or start taking any prescription medicines, over-the-counter medicines, or herbal supplements while taking ADDYI until you have talked with your doctor. Your doctor will tell you if it is safe to take other medicines or herbal supplements while you are taking ADDYI. • have liver problems. Do not take ADDYI if you have liver problems. If you take ADDYI and you feel lightheaded or dizzy, lie down right away. Get emergency medical help or ask someone to get emergency medical help for you if the symptoms do not go away or if you faint (lose consciousness). If you faint (lose consciousness), tell your doctor as soon as you can. ADDYI is only available through the ADDYI Risk Evaluation and Mitigation Strategy (REMS) Program because of the increased risk of severe low blood pressure and fainting (loss of consciousness) with alcohol use. You can only get ADDYI from pharmacies that are enrolled in the ADDYI REMS Program. For more information about the Program and a list of pharmacies that are enrolled in the ADDYI REMS Program, go to www.AddyiREMS.com or call 1-844-PINK-PILL (1-844- 746-5745). -

Comparison of Clinical Pharmacology of Voriconazole and Posaconazole 367
Review Despite greater knowledge and pos- sibilities in pharmacotherapy, fungal infections remain a challenge for cli- nicians. As the population of immu- Comparison of clinical nocompromised patients and those treated for their hematologic ailments pharmacology of voriconazole increases, the number of fungal infec- tions grows too. This is why there is and posaconazole still a quest for new antifungal drugs as well as for optimization of phar- macotherapy with already registered pharmaceutics. Voriconazole and posaconazole are broad-spectrum, new generation, tri- Beata M. Sienkiewicz, Łukasz Łapiński, Anna Wiela-Hojeńska azole antifungal agents. The drugs are used in the pharmacotherapy of Wroclaw Medical University, Wroclaw, Poland invasive aspergillosis, Candida and Fusarium infections. Voriconazole is also used in infections caused by Sce- dosporium. Posaconazole is used in Introduction the treatment of coccidioidomycosis Fungal infections are one of the most severe problems in clinical practice, and chromoblastomycosis. Besides some similarities, the two mentioned especially in hematology and oncology units. They make up from 9 to 10% drugs also show differences in thera- of all infections developing among hospitalized patients. Fungemia can be peutic indications, pharmacokinetics either a complication connected with the malignancy itself or an adverse (mainly absorption and metabolism), effect of the oncological treatment (chemo-, radio- and corticotherapy). Fur- frequency and severity of adverse thermore, it can influence the final -

Aetna Formulary Exclusions Drug List
Covered and non-covered drugs Drugs not covered – and their covered alternatives 2020 Advanced Control Plan – Aetna Formulary Exclusions Drug List 05.03.525.1B (7/20) Below is a list of medications that will not be covered without a Key prior authorization for medical necessity. If you continue using one of these drugs without prior approval, you may be required UPPERCASE Brand-name medicine to pay the full cost. Ask your doctor to choose one of the generic lowercase italics Generic medicine or brand formulary options listed below. Preferred Options For Excluded Medications1 Excluded drug name(s) Preferred option(s) ABILIFY aripiprazole, clozapine, olanzapine, quetiapine, quetiapine ext-rel, risperidone, ziprasidone, VRAYLAR ABSORICA isotretinoin ACANYA adapalene, benzoyl peroxide, clindamycin gel (except NDC^ 68682046275), clindamycin solution, clindamycin-benzoyl peroxide, erythromycin solution, erythromycin-benzoyl peroxide, tretinoin, EPIDUO, ONEXTON, TAZORAC ACIPHEX, esomeprazole, lansoprazole, omeprazole, pantoprazole, DEXILANT ACIPHEX SPRINKLE ACTICLATE doxycycline hyclate capsule, doxycycline hyclate tablet (except doxycycline hyclate tablet 50 mg [NDC^ 72143021160 only], 75 mg, 150 mg), minocycline, tetracycline ACTOS pioglitazone ACUVAIL bromfenac, diclofenac, ketorolac, PROLENSA acyclovir cream acyclovir (except acyclovir cream), valacyclovir ADCIRCA sildenafil, tadalafil ADZENYS XR-ODT amphetamine-dextroamphetamine mixed salts ext-rel†, dexmethylphenidate ext-rel, dextroamphetamine ext-rel, methylphenidate ext-rel†, MYDAYIS, -

Noxafil, INN-Posaconazole
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Noxafil 40 mg/mL oral suspension 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each mL of oral suspension contains 40 mg of posaconazole. Excipients with known effect This medicinal product contains approximately 1.75 g of glucose per 5 mL of suspension. This medicinal product contains 10 mg of sodium benzoate (E211) per 5 mL of suspension. This medicinal product contains up to 1.25 mg of benzyl alcohol per 5 mL of suspension. This medicinal product contains up to 24.75 mg of propylene glycol (E1520) per 5 mL of suspension. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Oral suspension White suspension 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Noxafil oral suspension is indicated for use in the treatment of the following fungal infections in adults (see section 5.1): - Invasive aspergillosis in patients with disease that is refractory to amphotericin B or itraconazole or in patients who are intolerant of these medicinal products; - Fusariosis in patients with disease that is refractory to amphotericin B or in patients who are intolerant of amphotericin B; - Chromoblastomycosis and mycetoma in patients with disease that is refractory to itraconazole or in patients who are intolerant of itraconazole; - Coccidioidomycosis in patients with disease that is refractory to amphotericin B, itraconazole or fluconazole or in patients who are intolerant of these medicinal products; - Oropharyngeal candidiasis: as first-line therapy in patients who have severe disease or are immunocompromised, in whom response to topical therapy is expected to be poor. -

Cancer and Leukemia Group B
Protocol Update #11 XX/XX/17 ALLIANCE FOR CLINICAL TRIALS IN ONCOLOGY _________________________________________ PROTOCOL UPDATE TO CALGB 10701/CTSU 10701 _________________________________________ A PHASE II STUDY OF DASATINIB (SPRYCEL®) (IND #73969, NSC #732517) AS PRIMARY THERAPY FOLLOWED BY TRANSPLANTATION FOR ADULTS ≥ 18 YEARS WITH NEWLY DIAGNOSED PH+ ACUTE LYMPHOBLASTIC LEUKEMIA BY CALGB, ECOG AND SWOG Investigational Agent: Dasatinib (IND #73969, NSC # 732517 will be supplied by NCI DCTD Companion Studies for Alliance Institutions: CALG 8461 (required), 9665 (optional) Companion Study for ECOG-ACRIN Institutions: E3903 (required) X Update: Status Change: Eligibility changes Activation Therapy / Dose Modifications / Study Calendar changes Closure Informed Consent changes Suspension / temporary closure Scientific / Statistical Considerations changes Reactivation X Data Submission / Forms changes Editorial / Administrative changes Other : Expedited review is allowed. IRB approval (or disapproval) is required within 90 days. Please follow your IRB of record guidelines. UPDATES TO THE PROTOCOL: Section 6.1 Data Submission - In the data submission table, the form “C10701 ABL1 Mutational Analysis Form” has been added prior to “During Treatment (Course I).” This form must be completed for all patients and mailed to the Alliance Statistics and Data Center. - In the data submission table, under “During Treatment (Course VI) and Post-Treatment Follow-Up,” the form “C10701 ABL1 Mutational Analysis Form” has been added. This form must be completed for all patients and mailed to the Alliance Statistics and Data Center. 1 Section 10.13 Filgrastim (G-CSF: Granulocyte Colony-Stimulating Factor; Neupogen; recombinant- methionyl human granulocyte-colony stimulating factor; r-methHuG-CSF; filgrastim-sndz, Zarxio(R)) Zarxio can be used in place of neupogen, therefore, the text “filgrastim-sndz, Zarxio(R)” has been added to the end of the section title. -
Prediction of Drug Interactions with Methadone, Buprenorphine and Oxycodone from in Vitro Inhibition of Metabolism
The author(s) shown below used Federal funds provided by the U.S. Department of Justice and prepared the following final report: Document Title: Prediction of Drug Interactions with Methadone, Buprenorphine and Oxycodone from In Vitro Inhibition of Metabolism Author(s): David E. Moody, Ph.D. Document No.: 250127 Date Received: July 2016 Award Number: 2011-DN-BX-K532 This report has not been published by the U.S. Department of Justice. To provide better customer service, NCJRS has made this federally funded grant report available electronically. Opinions or points of view expressed are those of the author(s) and do not necessarily reflect the official position or policies of the U.S. Department of Justice. February 2016 Research and Development in Forensic Toxicology Prediction of drug interactions with methadone, buprenorphine and oxycodone from in vitro inhibition of metabolism Final Technical Report Submitted electronically to: U.S. Department of Justice Office of Justice Programs National Institute of Justice Prepared by: David E. Moody. Ph.D. Director of the Center for Human Toxicology, and Research Professor of Pharmacology and Toxicology [email protected] / 801-581-5117 NIJ Award Number: 2011-DN-BX-K532 Reporting Period: January 1, 2012 to December 31, 2015 Recipient Organization: University of Utah 75 South 2000 East, Room 222 Salt Lake City, UT 84112-8930 Organizational DUNS: 0090953650000 EIN: 876000525 This document is a research report submitted to the U.S. Department of Justice. This report has not been published by the Department. Opinions or points of view expressed are those of the author(s) and do not necessarily reflect the official position or policies of the U.S. -

Pharmacokinetics, Pharmacodynamics
Supplementary Pharmacokinetics, Pharmacodynamics and Drug-Drug Interactions of New Anti-Migraine Drugs–Lasmiditan, Gepants, and Calcitonin-Gene-Related Peptide (CGRP) Receptor Monoclonal Antibodies Danuta Szkutnik-Fiedler Table S1. Possible drug-drug interactions of lasmiditan [14,28,31,35–38,40,42,45–47]. The risk or severity of Serum concentration of the Serum concentration of Lasmiditan may serotonin syndrome can following drugs (P-gp lasmiditan (P-gp substrate) increase the be potentially increased and/or BCRP substrates) may potentially increase bradycardic when lasmiditan is may potentially increase when it is combined with effects of the combined with the when combined with the following drugs3,. following drugs. following drugs1,. lasmiditan2,. 5-hydroxytryptophan* afatinib acebutolol alfentanil* alpelisib amlodipine almotriptan* ambrisentan atenolol amitriptiline* apixaban betaxolol amoxapine* belinostat carteolol buspirone* bisoprolol carvedilol citalopram* brentuximab vedotin diltiazem clomipramine* cabazitaxel esmolol cyclobenzaprine* ceritinib felodipine desipramine* cladribine isradipine desvenlavaxine* cobimetinib clobazam ivabradine dexfenfluramine* colchicine* daclatasvir labetalol dextromethorphan* cyclosporine erythromycin levobetaxolol dihydroergotamine* daunorubicin fexofenadine levobunolol dolasetron* delafloxacin lapatinib methyldopa doxepin* digitoxin ritonavir metipranolol doxepin topical* digoxin metoprolol duloxetine* donepezil nadolol eletriptan* doxorubicin nebivolol ergotamine* edoxaban* nicardipine escitalopram* -
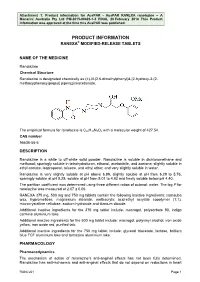
Attachment: Product Information: Ranolazine
Attachment 1: Product information for AusPAR - AusPAR RANEXA ranolazine – A Menarini Australia Pty Ltd PM-2015-00423-1-3 FINAL 20 February 2018 This Product information was approved at the time this AusPAR was published. PRODUCT INFORMATION RANEXA® MODIFIED-RELEASE TABLETS NAME OF THE MEDICINE Ranolazine Chemical Structure Ranolazine is designated chemically as (±)-N-(2,6-dimethylphenyl)4-[2-hydroxy-3-(2- methoxyphenoxy)propyl] piperazineacetamide. The empirical formula for ranolazine is C24H33N3O4 with a molecular weight of 427.54. CAS number 95635-55-5 DESCRIPTION Ranolazine is a white to off-white solid powder. Ranolazine is soluble in dichloromethane and methanol; sparingly soluble in tetrahydrofuran, ethanol, acetonitrile, and acetone; slightly soluble in ethyl acetate, isopropanol, toluene, and ethyl ether; and very slightly soluble in water. Ranolazine is very slightly soluble at pH above 6.99, slightly soluble at pH from 6.29 to 5.76, sparingly soluble at pH 5.25, soluble at pH from 5.01 to 4.82 and freely soluble below pH 4.40. The partition coefficient was determined using three different ratios of octanol: water. The log P for ranolazine was measured at 2.07 ± 0.06. RANEXA 375 mg, 500 mg and 750 mg tablets contain the following inactive ingredients: carnauba wax, hypromellose, magnesium stearate, methacrylic acid-ethyl acrylate copolymer (1:1), microcrystalline cellulose, sodium hydroxide and titanium dioxide. Additional inactive ingredients for the 375 mg tablet include: macrogol, polysorbate 80, indigo carmine aluminium lake. Additional inactive ingredients for the 500 mg tablet include: macrogol, polyvinyl alcohol, iron oxide yellow, iron oxide red, purified talc. -

Sacubitril/Valsartan
Wednesday, June 8, 2016 4 p.m. Oklahoma Health Care Authority 4345 N. Lincoln Blvd. Oklahoma City, OK 73105 The University of Oklahoma Health Sciences Center COLLEGE OF PHARMACY PHARMACY MANAGEMENT CONSULTANTS MEMORANDUM TO: Drug Utilization Review (DUR) Board Members FROM: Bethany Holderread, Pharm.D. SUBJECT: Packet Contents for DUR Board Meeting – June 8, 2016 DATE: May 20, 2016 Note: The DUR Board will meet at 4:00 p.m. The meeting will be held at 4345 N Lincoln Blvd. Enclosed are the following items related to the June meeting. Material is arranged in order of the agenda. Call to Order Public Comment Forum Action Item – Approval of DUR Board Meeting Minutes – Appendix A Update on Medication Coverage Authorization Unit/SoonerPsych Program Update – Appendix B Action Item – Vote to Prior Authorize Zepatier™ (Elbasvir/Grazoprevir) – Appendix C Action Item – Vote to Prior Authorize Eloctate™ [Antihemophilic Factor (Recombinant), Fc Fusion Protein], Adynovate® [Antihemophilic Factor (Recombinant), PEGylated], Alprolix® [Coagulation Factor IX (Recombinant), Fc Fusion Protein], Idelvion® [Coagulation Factor IX (Recombinant), Albumin Fusion Protein], Obizur® [Antihemophilic Factor (Recombinant), Porcine Sequence], Corifact® [Factor XIII Concentrate (Human)], Tretten® [Coagulation Factor XIII A-Subunit (Recombinant)], and Coagadex® [Coagulation Factor X (Human)], and Establish Pharmacy Provider Standards of Care – Appendix D Action Item – Vote to Prior Authorize Vaginal Progesterone Products (Crinone® and Endometrin®) and Update Makena® (Hydroxyprogesterone