Planning a Healthy Menu a Toolkit for Supportive Living Sites
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Diet Industry the Diet Industry
Issue: The Diet Industry The Diet Industry By: Lisa Rabasca Roepe Pub. Date: March 5, 2018 Access Date: September 24, 2021 DOI: 10.1177/237455680408.n1 Source URL: http://businessresearcher.sagepub.com/sbr-1946-105904-2881576/20180305/the-diet-industry ©2021 SAGE Publishing, Inc. All Rights Reserved. ©2021 SAGE Publishing, Inc. All Rights Reserved. Will it adapt to changing attitudes? Executive Summary The $70.3 billion industry for diet products and plans is experiencing a shakeout as consumer perceptions shift. The industry still fills a need, since about 70 percent of U.S. adults are overweight or obese, according to government data. But attitudes about how to control weight are changing, as many dieters bounce from one plan to another without finding satisfaction. Many give up on dieting altogether in favor of a broader approach that emphasizes eating a wider variety of foods, exercising and seeking to sustain a healthy lifestyle. In addition, new competitors are entering the field to challenge the traditional industry leaders, but the established firms are finding ways to survive in the changing climate. Key takeaways include: The year 2017 was a period of recovery for the industry after several down years for major players such as Weight Watchers. One well-established company, Nutrisystem, has been especially successful in adapting to a changing business environment by seeking partnerships with major retailers. Fitness apps and trackers, once seen as a potential industry disrupter, have had a mixed record, in part because owners often stop using them after a few months. Click hear to listen to an interview with author Lisa Rabasca Roepe. -

Clear Liquid Diet for Diabetics
CLEAR LIQUID DIET FOR DIABETICS Important Facts About Diet: 1. The liquid meal plan that is given to you will replace only the calories that you would normall get from the carbohydrates containing foods in your diet (such as breads, starches, cereals, fruits, and vegetables.) For Example: the plan that replaces a 1500 calorie diet will provide approximately 900 calories. If you replaced all the calories in your diet with juices and sweetened beverages, it could cause your blood sugar to be too high. 2. You will reduce your normal dosage of daily insulin to 2/3 normal dosage on each day you are on clear liquids. Do NOT take insulin the morning of your test, however, it is very important that you bring your insulin with you. Basic List of Foods Considered As Clear Liquids: (NO MILK OR MILK PRODUCTS) Soft drinks (regular, not Sugar-Free) Gatorade (NO RED or PURPLE) Fat-Free Broth or Boullion Lemonade (powdered) Jello – Yellow or Green only Popsicles (only clear fruit flavored) Coffee Fruit Juice / Drinks (NO PULP) (NO RED or PURPLE) Tea Kool-Aid (NO RED or GRAPE) DIABETIC CLEAR LIQUID DIET FOOD GROUPS: Group A (each serving contains about 40 calories) Apple Juice 1/3 cup Fruit Juice ½ cup Lemonade ½ cup Sugar 1 Tbsp. Lemon-Lime Soda ½ cup Gingerale ½ cup White Cranberry Juice ¼ cup Sweetened Gelatin ¼ cup Popsicle ½ Twin Bar Fat-Free Broth/Boullion - any amount Group B (each serving contains about 60 calories) Apple Juice 1/3 cup White Cranberry Juice 1/3 cup Lemonade ¾ cup Gingerale ¾ cup Lemon-Lime Soda ¾ cup Fat-Free Broth/Boullion -any -

1. Exposure Data
1. EXPOSURE DATA 1.1 Identification of the agents by-products such as blood. It is also important to distinguish between industrial processing The focus of thisMonograph is the consump- and household preparations. As there is a huge tion of red meat and processed meat. These terms variety of processed meat products, it is difficult are defined below. to sort them into categories (Santarelli et al., 2008). However, based on recommendations by 1.1.1 Red meat the Food and Agriculture Organization of the United Nations (FAO) (Heinz & Hautzinger, Red meat refers to fresh unprocessed 2007), different groups of industrial processed mammalian muscle meat (e.g. beef, veal, pork, meats can be proposed. lamb, mutton, horse, or goat meat), which may be minced or frozen, and is usually (a) Cured meat pieces consumed cooked. Examples of cured meat include raw beef, raw 1.1.2 Offal ham, cooked beef, cooked ham, corned beef, and bacon. Mammalian offal refers to the internal Curing is a process by which the meat is organs and entrails of a butchered animal (e.g. treated with a small amount of salt (sodium scrotum, small intestine, heart, brain, kidney, chloride, NaCl, with or without potassium chlo- liver, thymus, pancreas, testicle, tongue, tripe, or ride, KCl), with or without nitrate or nitrite salts. stomach) consumed as such. Mammalian offal Curing enhances shelf-life by preserving and is considered to be a specific food category in preventing the spoilage of meat. Cured meat cuts food consumption surveys (FAO, 2015); however, are made of entire pieces of muscle meat and can mammalian offal is reported together with red be subdivided into two groups: cured raw meats meat in some epidemiological studies. -

Mediterranean Diet Food: Strategies to Preserve a Healthy Tradition
imental er Fo p o x d E C Journal of Experimental Food f h o e l m a n i Boskou, J Exp Food Chem 2016, 1:1 s r t u r y o J Chemistry DOI: 10.4172/2472-0542.1000104 ISSN: 2472-0542 Review Article open access Mediterranean Diet Food: Strategies to Preserve a Healthy Tradition Dimitrios Boskou* Aristotle University of Thessaloniki, Greece *Corresponding author: Dimitrios Boskou, Aristotle University of Thessaloniki, Greece, Tel: +30 2310997791; E-mail: [email protected] Received date: September 21, 2015; Accepted date: November 28, 2015; Published date: December 7, 2015 Copyright: © 2015 Boskou D. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract The traditional Mediterranean diet refers to a dietary pattern found in olive growing areas of the Mediterranean region. It’s essential characteristic is the consumption of virgin olive oil, vegetables, fresh fruits, grains, pasta, bread, olives, pulses, nuts and seeds. Moderate amounts of fish, poultry, dairy products and eggs are consumed with small amounts of red meat and wine. Over the past few decades there has been a growing interest in the role of the Mediterranean diet in preventing the development of certain diseases, especially cardiovascular disease. Mediterranean food products are now re-evaluated for the beneficial health effects in relation to the presence of bioactive compounds. The body of science unraveling the role of bioactives such as phenolic acids, various polyphenols, flavonoids, lignans, hydroxyl-isochromans, olive oil secoiridoids, triterpene acids and triterpene alcohols, squalene, αlpha-tocopherol and many others is growing rapidly. -

Incorporating Away-From-Home Foods Into a Healthy Eating Plan
Incorporating Away–From–Home Food into a Healthy Eating Plan Summary Much of this brief is based upon a In our often time-pressed society, convenience is a recently published way of life for many individuals. Foods and meals report: The prepared outside of the home are an increasingly Keystone Forum 1, 2 important part of the American diet. This is a on Away-From- trend that has coincided with a dramatic rise in the Home Foods: prevalence of obesity. While food, wherever prepared, Opportunities for is not the only factor affecting body weight, away- Preventing Weight from-home food should be an important consideration Gain and Obesity.3 for people aiming to maintain or lose weight. A The report resulted growing body of literature indicates that the eating from consensus of away-from-home food can be a factor influencing building workshops energy intake. Informed choices pertaining to away- which included from-home food could help reduce calorie over participants from consumption and aid in weight management. the private sector, nongovernmental The objectives of this brief are to: organizations, Summarize environmental and societal changes academia, and government to “identify the state of that may contribute to the increased consumption of the evidence, as well as, important knowledge gaps, away-from-home food. regarding obesity and weight gain prevention and away-from-home foods.” Review the properties of away-from-home-food that may facilitate the over-consumption of energy. In this brief, away-from-home food refers to food Examine studies investigating the relationship of prepared and purchased outside of the home. -
RENEW FOOD PLAN Comprehensive Guide
RENEW FOOD PLAN Comprehensive Guide Version 4 Table of Contents What is the “ReNew Food Plan”? .... 3 Why ReNew? .................................... 4 Features of ReNew Food Plan ......... 5 Touring Through the ReNew Food Plan .......................... 17 Preparing for the ReNew Food Plan .......................... 24 Frequently Asked Questions ......... 25 Resources and Tools for Success .. 28 © 2020 The Institute for Functional Medicine What is the “ReNew Food Plan”? The ReNew Food Plan recommended by a Functional Medicine practitioner is a therapeutic, short-term approach followed for a specific amount of time, often used as a first step in: n Ridding the body of the most common foods that cause inflammation n Identifying food allergies, sensitivities, intolerances, and triggers n Eliminating foods with potentially harmful components n Providing nutritional support for the body’s detoxification systems The following questions may help to determine if the ReNew Food Plan is right for an individual: n Do you routinely consume and crave fast food, packaged foods, and processed foods with sugar or flour? n Do you consume fish or shellfish regularly? If so, what kind and where does it come from? n Do you regularly eat fruits and vegetables that are non-organic? n Do you eat fewer than five servings of fresh fruits or vegetables per day? n Do you consume lots of animal products every day (e.g., meat, milk, cheese, and eggs)? If a person answers “yes” to one or more of the questions above, he or she may have a physical or emotional attachment to sugar or processed foods, may be exposed to a high level of potential food triggers or allergens, or may have a high total body burden of toxins. -

Development of Food Chemistry, Natural Products, and Nutrition Research: Targeting New Frontiers
foods Editorial Development of Food Chemistry, Natural Products, and Nutrition Research: Targeting New Frontiers Antonello Santini 1,* and Nicola Cicero 2 1 Department of Pharmacy, University of Napoli Federico II, Via D. Montesano 49, 80131 Napoli, Italy 2 Department of Biomedical and Dental Sciences and Morphofunctional Imaging, University of Messina, Polo Universitario Annunziata, 98125 Messina, Italy; [email protected] * Correspondence: [email protected]; Tel.: +39-81-253-9317 Received: 3 April 2020; Accepted: 4 April 2020; Published: 12 April 2020 Abstract: The Special Issue entitled: “Development of Food Chemistry, Natural Products, and Nutrition Research” is focused on the recent development of food chemistry research, including natural products’ sources and nutrition research, with the objectives of triggering interest towards new perspectives related to foods and opening a novel horizon for research in the food area. The published papers collected in this Special Issue are studies that refer to different aspects of food, ranging from food chemistry and analytical aspects, to composition, natural products, and nutrition, all examined from different perspectives and points of view. Overall, this Special Issue gives a current picture of the main topics of interest in the research and proposes studies and analyses that may prompt and address the efforts of research in the food area to find novel foods and novel applications and stimulate an environmentally-friendly approach for the re-use of the by-products of the agro-food area. This notwithstanding, the main challenge is currently addressed to achieve a full comprehension of the mechanisms of action of food components, the nutrients, outlining their high potential impact as preventive and/or therapeutic tools, not only as a source of macro- and/or micro-nutrients, which are necessary for all the metabolic and body functions. -

CHEMICAL CUISINE ~ COMMONLY USED FOOD ADDITIVES from A-Z
CHEMICAL CUISINE ~ COMMONLY USED FOOD ADDITIVES from A-Z Have you ever wondered why peanut butter doesn’t separate? Why baking mixes rise in the oven? Why ice cream is smooth and creamy? Most likely, you take food appearances and quality for granted. But desirable qualities in processed foods can often be attributed to food additives. People have been using food additives for There are two categories of additives that are thousands of years. Today nearly 3,000 substances exempt from the testing and approval process. are used as food additives. Salt, sugar, and corn syrup Almost 700 substances are on the Generally are the most widely used food additives in the United Recognized as Safe (GRAS) list. These substances States. Another 12,000 find their way into our food are already considered harmless because of extensive supply indirectly, including pesticides. use in the past with no known harmful effects. Americans want to know...are additives safe, or Prior Sanctioned Substances are also exempt and do they increase our risk for cancer and other include those additives approved before 1958 for use diseases? Intentional food additives pose little health in food. The safety of approved additives is hazard because so much is known about food continually under review. Additives never have additives, and their use is well regulated. The permanent approval. exception lies with a small number of individuals with specific allergies, who may actually experience Monitoring the Safety of Food Additives reactions to food additives. Before any substance can be added to food, its safety must be assessed. FDA evaluates the safety of History of Food Additives all food additives. -

Hunger and Nutrition from Belly-Full to Body-Fuel
Hunger and Nutrition from belly-full to body-fuel Hunger and Nutrition from belly-full to body-fuel Inter-American Institute for Cooperation on Agriculture (IICA), 2015 Hunger and nutrition from belly-full to body-fuel by IICA is licensed under a Creative Commons Attribution-ShareAlike 3.0 IGO (CC-BY-SA 3.0 IGO) (http://creativecommons.org/licenses/by-sa/3.0/igo/) Based on a work at www.iica.int IICA, CTA and CaRAPN encourages the fair use of this document. Proper citation is requested. This publication is also available in electronic (PDF) format from the Institute’s Web site: http://www.iica.int, www.cta.int and www.pn4ad.org Editorial coordination: Diana Francis Mechanical Editing: Steve Maximay and Marissa Wilson Layout: Kathryn Duncan Cover design: Kathryn Duncan Printed: The Office Authority Limited Hunger and nutrition from belly-full to body-fuel /CARAPN, CTA, IICA - San Jose, C.R.: IICA, 2015. 122 p.: 22.86 cm x 20.32 cm ISBN: 978-92-9248-566-5 1. Famine 2. Malnutrition 3. Foods 4. Food supply 5. human nutrition 6. Food security 7. Health 8. Nutritional status 9. Food consumption 10. Caribbean I. CARAPN II. CTA III. IICA IV. Title AGRIS DEWEY E10 338.19 Port of Spain, Trinidad and Tobago 2015 Food is an important and major, but not only source of nutrition. But all foods are not equal! To keep the body healthy, an individual must choose among the wide range of options and within their means, foods that are ‘nutrient dense’. Simply put, individuals must ‘fuel-up’ on a mix of foods that have the greatest nutritional value and not ‘fill-up’ on ‘empty calorie’ foods. -

A Review on Mechanisms and Commercial Aspects of Food Preservation and Processing Sadat Kamal Amit†, Md
Amit et al. Agric & Food Secur (2017) 6:51 DOI 10.1186/s40066-017-0130-8 Agriculture & Food Security REVIEW Open Access A review on mechanisms and commercial aspects of food preservation and processing Sadat Kamal Amit†, Md. Mezbah Uddin†, Rizwanur Rahman, S. M. Rezwanul Islam and Mohidus Samad Khan* Abstract Food preservation involves diferent food processing steps to maintain food quality at a desired level so that maxi- mum benefts and nutrition values can be achieved. Food preservation methods include growing, harvesting, processing, packaging, and distribution of foods. The key objectives of food preservation are to overcome inappropri- ate planning in agriculture, to produce value-added products, and to provide variation in diet. Food spoilage could be caused by a wide range of chemical and biochemical reactions. To impede chemical and microbial deterioration of foods, conventional and primitive techniques of preserving foods like drying, chilling, freezing, and pasteurization have been fostered. In recent years, the techniques to combat these spoilages are becoming sophisticated and have gradually altered to a highly interdisciplinary science. Highly advanced technologies like irradiation, high-pressure technology, and hurdle technology are used to preserve food items. This review article presents and discusses the mechanisms, application conditions, and advantages and disadvantages of diferent food preservation techniques. This article also presents diferent food categories and elucidates diferent physical, chemical, and microbial factors responsible for food spoilage. Furthermore, the market economy of preserved and processed foods has been ana- lyzed in this article. Keywords: Food category, Food spoilage, Food preservation, Food processing, Global market Background increase its shelf life retaining original nutritional values, Foods are organic substances which are consumed for color, texture, and favor. -
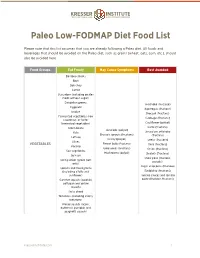
Paleo Low-FODMAP Diet Food List.Pages
! Paleo Low-FODMAP Diet Food List Please note that this list assumes that you are already following a Paleo diet. All foods and beverages that should be avoided on the Paleo diet, such as grains (wheat, oats, corn, etc.), should also be avoided here. Food Groups Eat Freely May Cause Symptoms Best Avoided Bamboo shoots Beet Bok choy Carrot Cucumber (including pickles made without sugar) Dandelion greens Artichoke (fructose) Eggplant Asparagus (fructose) Endive Broccoli (fructans) Fermented vegetables (raw Cabbage (fructans) sauerkraut, or lacto- fermented vegetables) Cauliflower (polyol) Green beans Garlic (fructans) Avocado (polyol) Kale Jerusalem artichoke Brussels sprouts (fructans) (fructans) Lettuce Celery (polyol) Leeks (fructans) Olives VEGETABLES Fennel bulb (fructans) Okra (fructans) Parsnip Green peas (fructans) Onion (fructans) Sea vegetables Mushrooms (polyol) Shallots (fructans) Spinach Snow peas (fructans, Spring onion (green part polyols) only) Sugar snap peas (fructose) Sprouts and microgreens (including alfalfa and Raddichio (fructans) sunflower) Tomato sauces and tomato Summer squash (zucchini, paste (fructose, fructans) pattypan and yellow squash) Swiss chard Tomatoes (including cherry tomatoes) Winter squash (acorn, butternut, pumpkin and spaghetti squash) kresserinstitute.com 1 ! Food Groups Eat Freely May Cause Symptoms Best Avoided Banana, ripe Blueberries Grapefruit Apple (fructose and polyol) Kiwi Apricot (polyol) Lemon Cherries (fructose and Lime polyol) Banana, unripe Mandarin Mango (fructose) Longon (polyol) Melons -

Sugar and Sugar Substitutes
Sugar and Sugar Substitutes There are two types of sweeteners found in food and beverages: sugars and sugar substitutes. Sugars provide calories, or energy, for our bodies and increase blood glucose, as well as overall calorie intake. All carbohydrate-containing foods, such as breads, fruits, vegetables, milk, and yogurt, increase blood sugar, even if they do not have added sugars. How sugars appear on package ingredient lists: . Sugar . Dextrose . Corn syrup or High Fructose Corn syrup . Lactose . Honey . Sucrose . Glucose . Maltose Sugar substitutes (artificial sweeteners) provide little or no calories or carbohydrates and do not increase blood sugar. Therefore, choosing sugar substitutes can assist with controlling carbohydrate and energy intake. Sugar alcohols are also used to replace sugar in food. Sugar alcohols are incompletely absorbed by your body and contain about half the carbohydrate and calories as sugar. Sugar substitutes approved by the Food and Drug Administration: . Acesulfame K . Saccharin (Sweet n’ Low) . Aspartame (Nutrasweet/Equal) . Stevia (multiple brands) . Luo han guo fruit extract (Monk Fruit) . Sucralose (Splenda) . Neotame Sugar alcohols commonly found in food: Sorbitol, Mannitol, Xylitol, Maltitol, Isomalt Sugar substitutes … safe to use or not? Are you confused about the safety of sugar substitutes? Consider the following: Concern: Sugar substitutes may increase hunger or cause overeating at later meals. Be aware that studies have shown people are more likely to overeat foods prepared with sugar substitutes. Benefit: Sugar substitutes offer a sweet taste without increasing blood glucose or calories. If you have diabetes check your carbohydrate intake and adjust it to help control blood sugar. Choosing sugar substitutes is one way to assist you with limiting carbohydrate intake.