Delivery OB-GYN 101 Facts Card ©2003 Brookside Press
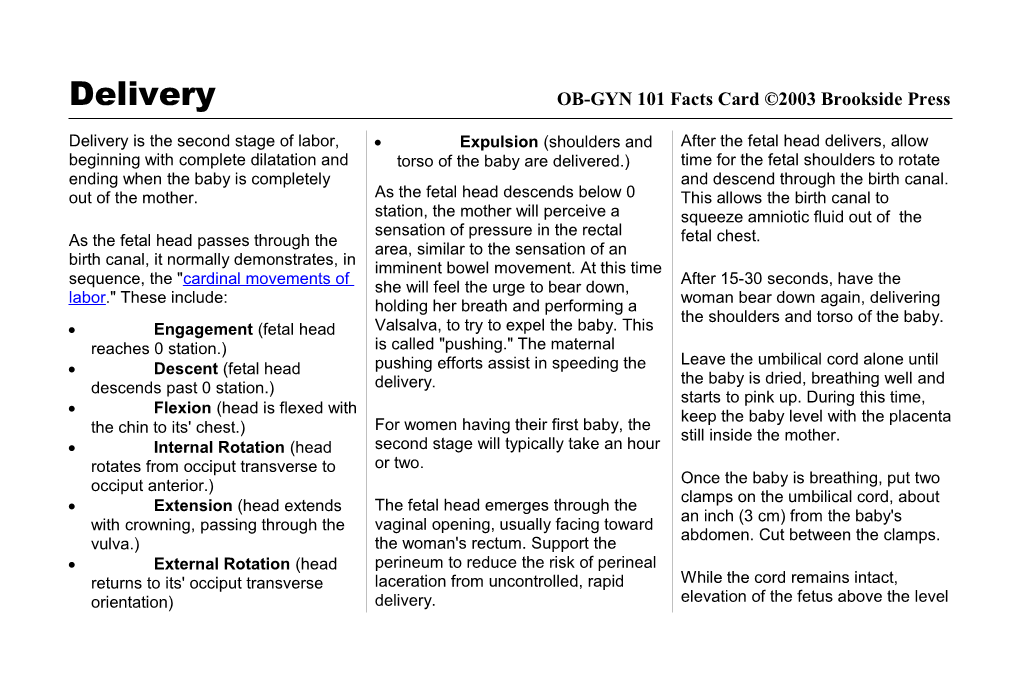
Delivery is the second stage of labor, Expulsion (shoulders and After the fetal head delivers, allow beginning with complete dilatation and torso of the baby are delivered.) time for the fetal shoulders to rotate ending when the baby is completely and descend through the birth canal. out of the mother. As the fetal head descends below 0 This allows the birth canal to station, the mother will perceive a squeeze amniotic fluid out of the sensation of pressure in the rectal As the fetal head passes through the fetal chest. area, similar to the sensation of an birth canal, it normally demonstrates, in imminent bowel movement. At this time sequence, the "cardinal movements of After 15-30 seconds, have the she will feel the urge to bear down, labor." These include: woman bear down again, delivering holding her breath and performing a the shoulders and torso of the baby. Engagement (fetal head Valsalva, to try to expel the baby. This reaches 0 station.) is called "pushing." The maternal Leave the umbilical cord alone until Descent (fetal head pushing efforts assist in speeding the the baby is dried, breathing well and descends past 0 station.) delivery. starts to pink up. During this time, Flexion (head is flexed with keep the baby level with the placenta For women having their first baby, the the chin to its' chest.) still inside the mother. Internal Rotation (head second stage will typically take an hour rotates from occiput transverse to or two. occiput anterior.) Once the baby is breathing, put two clamps on the umbilical cord, about Extension (head extends The fetal head emerges through the an inch (3 cm) from the baby's with crowning, passing through the vaginal opening, usually facing toward abdomen. Cut between the clamps. vulva.) the woman's rectum. Support the External Rotation (head perineum to reduce the risk of perineal returns to its' occiput transverse laceration from uncontrolled, rapid While the cord remains intact, orientation) delivery. elevation of the fetus above the level of the placenta results in pooling of The uterus becomes Encourage firm uterine contraction newborn blood within the making the globular. with uterine massage. baby somewhat anemic. Holding the The uterus enlarges. baby below the level of the placenta results in pooling of placental blood As the placenta separates, the woman within the newborn, leading to will again feel painful uterine cramps. increased neonatal jaundice. Keep the As the placenta descends, she will feel baby level with the placenta until the the urge to bear down and will push out cord is clamped. the placenta.
If the baby is not breathing well after If the placenta is not promptly expelled, delivery and needs resuscitation, or if the patient hemorrhages while immediately clamp and cut the cord so awaiting delivery of the placenta, this is you can move the baby to the called a "retained placenta" and it resuscitation area. should be manually removed.
After delivery of the baby, the placenta After delivery of the placenta, the is still attached inside the uterus. Some uterus normally contracts firmly, time later, the placenta will detach from closing off the open blood vessels the uterus and then be expelled. This Without this contraction, rapid blood process is called the "3rd stage of loss occurs. labor" and may take just a few minutes or as long as an hour. To firmly contract the uterus, give oxytocin 10 mIU IM or IV. Breast Signs of placenta separation include: feeding the baby or providing nipple stimulation causes release of oxytocin, A sudden gush of blood causing similar, but milder effects. Lengthening of the cord.