Appendix B
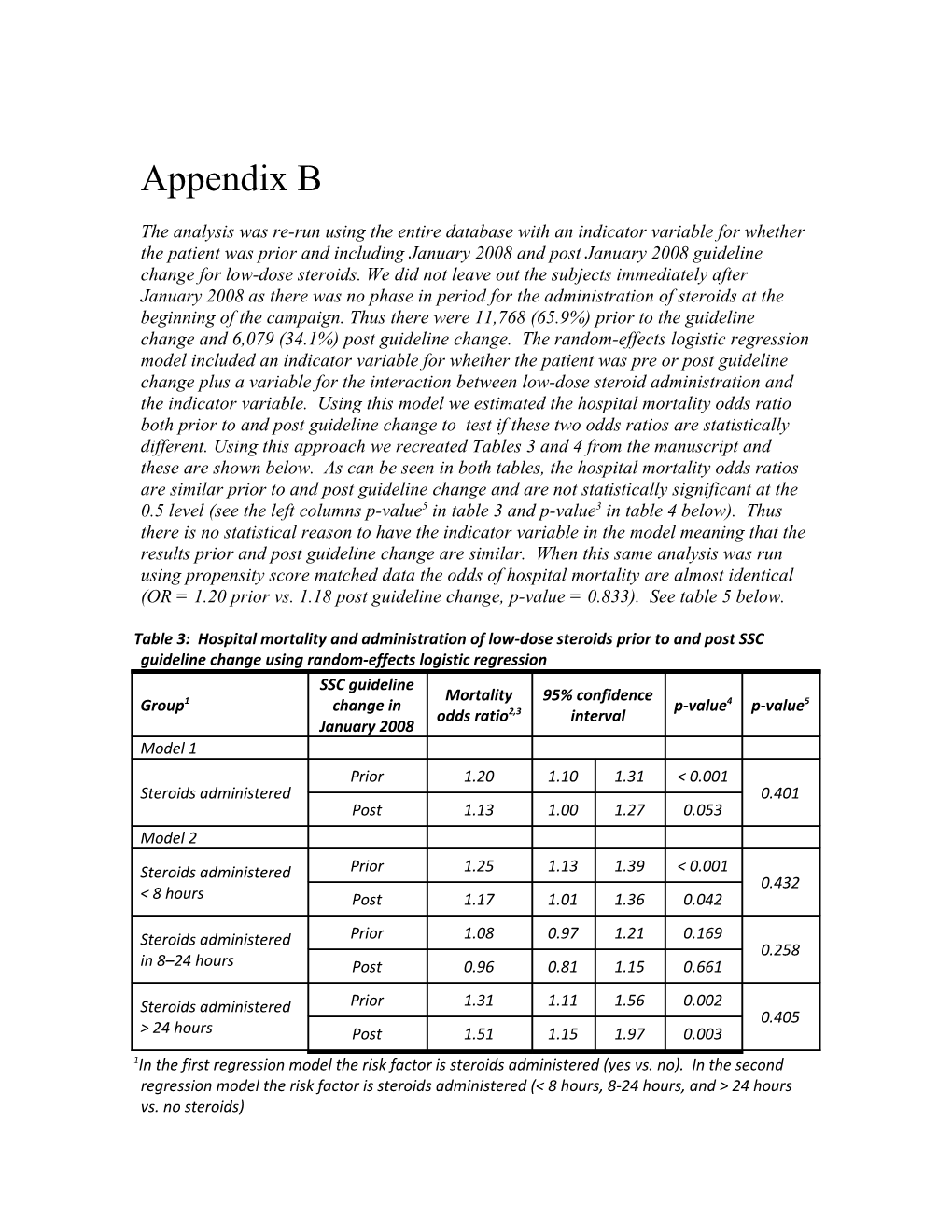
The analysis was re-run using the entire database with an indicator variable for whether the patient was prior and including January 2008 and post January 2008 guideline change for low-dose steroids. We did not leave out the subjects immediately after January 2008 as there was no phase in period for the administration of steroids at the beginning of the campaign. Thus there were 11,768 (65.9%) prior to the guideline change and 6,079 (34.1%) post guideline change. The random-effects logistic regression model included an indicator variable for whether the patient was pre or post guideline change plus a variable for the interaction between low-dose steroid administration and the indicator variable. Using this model we estimated the hospital mortality odds ratio both prior to and post guideline change to test if these two odds ratios are statistically different. Using this approach we recreated Tables 3 and 4 from the manuscript and these are shown below. As can be seen in both tables, the hospital mortality odds ratios are similar prior to and post guideline change and are not statistically significant at the 0.5 level (see the left columns p-value5 in table 3 and p-value3 in table 4 below). Thus there is no statistical reason to have the indicator variable in the model meaning that the results prior and post guideline change are similar. When this same analysis was run using propensity score matched data the odds of hospital mortality are almost identical (OR = 1.20 prior vs. 1.18 post guideline change, p-value = 0.833). See table 5 below.
Table 3: Hospital mortality and administration of low-dose steroids prior to and post SSC guideline change using random-effects logistic regression SSC guideline Mortality 95% confidence Group1 change in p-value4 p-value5 odds ratio2,3 interval January 2008 Model 1 Prior 1.20 1.10 1.31 < 0.001 Steroids administered 0.401 Post 1.13 1.00 1.27 0.053 Model 2
Steroids administered Prior 1.25 1.13 1.39 < 0.001 0.432 < 8 hours Post 1.17 1.01 1.36 0.042
Steroids administered Prior 1.08 0.97 1.21 0.169 0.258 in 8–24 hours Post 0.96 0.81 1.15 0.661
Steroids administered Prior 1.31 1.11 1.56 0.002 0.405 > 24 hours Post 1.51 1.15 1.97 0.003 1In the first regression model the risk factor is steroids administered (yes vs. no). In the second regression model the risk factor is steroids administered (< 8 hours, 8-24 hours, and > 24 hours vs. no steroids) 2reference group is no steroids administered 3Steroid logistic regression model odds ratio adjusted for the following variables: pulmonary infection, cardiovascular organ failure, pulmonary organ failure, mechanical ventilation, the interaction between pulmonary organ failure and mechanical ventilation, hepatic organ failure, renal organ failure, measured lactate, blood culture before antibiotics, broad spectrum antibiotics, glucose control, pneumonia, urinary tract infection, abdominal infection, location of sepsis (ED, ward, or ICU), region (North America, Europe, or South America), and median glucose within 24 hours of time of presentation. 4p-value test if the odds ratio is less significantly different from 1.0 5p-value test if the odds ratios are significantly different from prior to post guideline change in January 2008 Table 4: Hospital mortality and administration of low-dose steroids in subjects with either 1 or ≥ 2 organ failures prior to and post SSC guideline change using random-effects logistic regression SSC guideline Steroid OR for Condition change in 95% CI p-value2 p-value3 treatment steroids1 January 2008 ≥ 2 organ 1.08- Prior 1.20 0.001 failures 1.33 0.963 1 organ 1.04- Prior 1.21 0.016 All steroids failure 1.40 versus none ≥ 2 organ 0.94- [N = 17,847] Post 1.09 0.247 failures 1.27 0.440 1 organ 0.99- Post 1.19 0.070 failure 1.46 ≥ 2 organ 1.14- Prior 1.29 < 0.001 failures 1.46 0.515 1 organ 1.01- Prior 1.20 0.038 Steroids ≤ 8 failure 1.44 hours vs. none ≥ 2 organ 0.93- [N = 13,715] Post 1.13 0.206 failures 1.37 0.488 1 organ 0.99- Post 1.26 0.061 failure 1.60 ≥ 2 organ 1.06- Prior 1.18 0.002 failures 1.32 0.965 1 organ 1.01- Prior 1.18 0.039 Steroids ≤ 24 failure 1.38 hours vs. none ≥ 2 organ 0.88- [N = 16,854] Post 1.03 0.701 failures 1.21 0.370 1 organ 0.95- Post 1.16 0.155 failure 1.42 1Random-effects logistic regression model odds ratio adjusted for the following variables: pulmonary infection, cardiovascular organ failure, mechanical ventilation, pulmonary organ failure, the interaction between pulmonary organ failure and mechanical ventilation, hepatic organ failure, renal organ failure, measured lactate, blood culture before antibiotics, broad spectrum antibiotics, glucose control, pneumonia, urinary tract infection, abdominal infection, source of sepsis (ED, ward, or ICU), region (North America, Europe, or South America), and median glucose within 24 hours of time of presentation 2p-value tests if odds ratio is significantly different from 1.0 3p-value tests if the ≥ 2 organ failure odds ratio is significantly different from the 1 organ failure odds ratio Table 5: Hospital mortality random-effects logistic regression for low-dose steroid administration SSC guideline Mortality 95% Steroids administered change in odds confidence p-value2 p-value3 January 2008 ratio1 interval Prior Unadjusted model using 1:1 1.20 1.08 1.33 0.001 N = 7,039 propensity score matched 0.833 Post steroid administration 1.18 1.01 1.35 0.026 N = 3,893 1Referent group is no steroids administered. 2p-value test if the odds ratio is less significantly different from 1.0 3p-value test if the odds ratios are significantly different from prior to post guideline change in January 2008