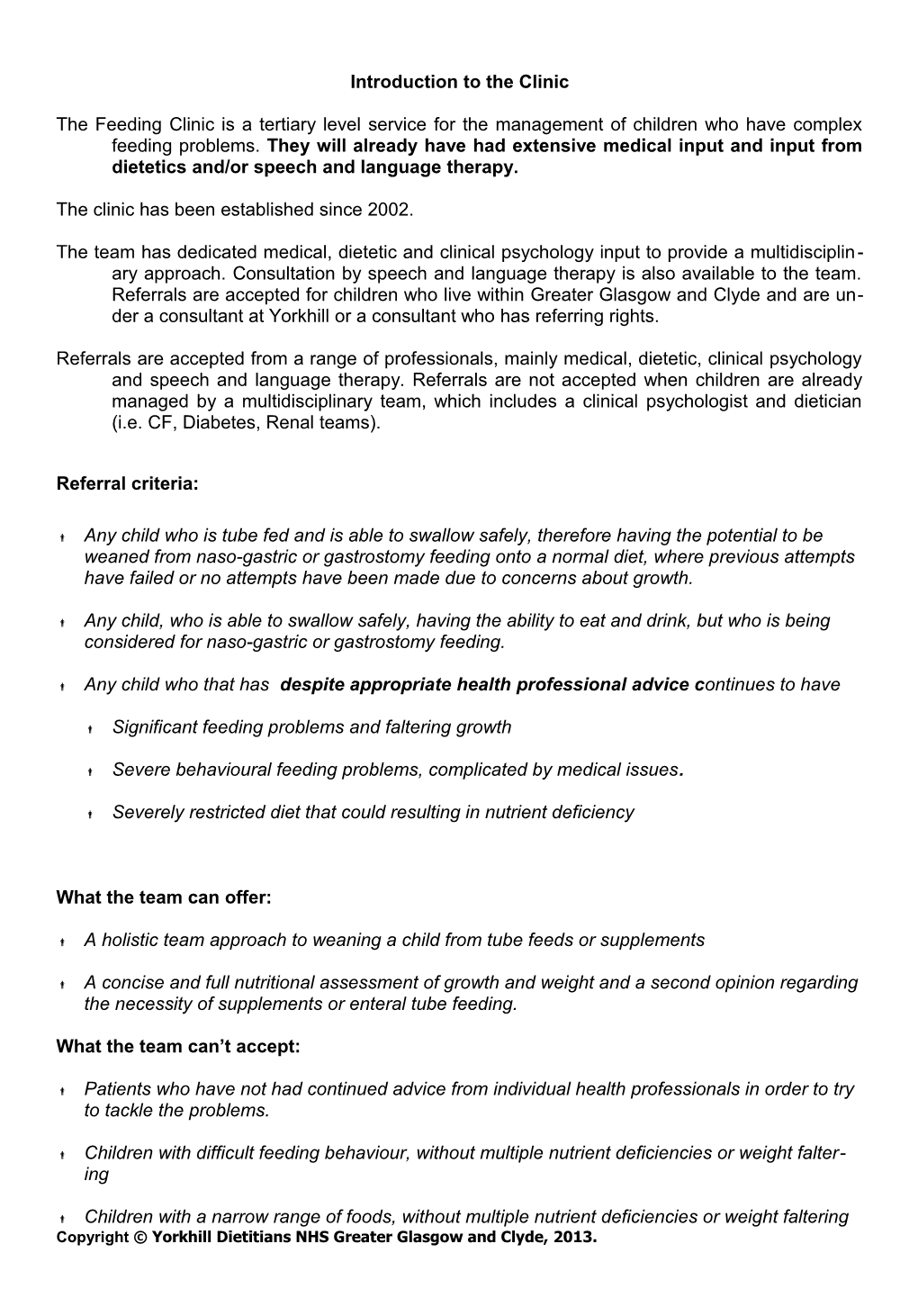
Introduction to the Clinic
The Feeding Clinic is a tertiary level service for the management of children who have complex feeding problems. They will already have had extensive medical input and input from dietetics and/or speech and language therapy.
The clinic has been established since 2002.
The team has dedicated medical, dietetic and clinical psychology input to provide a multidisciplin- ary approach. Consultation by speech and language therapy is also available to the team. Referrals are accepted for children who live within Greater Glasgow and Clyde and are un- der a consultant at Yorkhill or a consultant who has referring rights.
Referrals are accepted from a range of professionals, mainly medical, dietetic, clinical psychology and speech and language therapy. Referrals are not accepted when children are already managed by a multidisciplinary team, which includes a clinical psychologist and dietician (i.e. CF, Diabetes, Renal teams).
Referral criteria:
Any child who is tube fed and is able to swallow safely, therefore having the potential to be weaned from naso-gastric or gastrostomy feeding onto a normal diet, where previous attempts have failed or no attempts have been made due to concerns about growth.
Any child, who is able to swallow safely, having the ability to eat and drink, but who is being considered for naso-gastric or gastrostomy feeding.
Any child who that has despite appropriate health professional advice continues to have
Significant feeding problems and faltering growth
Severe behavioural feeding problems, complicated by medical issues.
Severely restricted diet that could resulting in nutrient deficiency
What the team can offer:
A holistic team approach to weaning a child from tube feeds or supplements
A concise and full nutritional assessment of growth and weight and a second opinion regarding the necessity of supplements or enteral tube feeding.
What the team can’t accept:
Patients who have not had continued advice from individual health professionals in order to try to tackle the problems.
Children with difficult feeding behaviour, without multiple nutrient deficiencies or weight falter- ing
Children with a narrow range of foods, without multiple nutrient deficiencies or weight faltering Copyright © Yorkhill Dietitians NHS Greater Glasgow and Clyde, 2013. Summary of roles within the team
Consultant Paediatrician and SPR – The consultant and/or SpR carry out a detailed review of the medical notes, noting growth and feeding history. The growth history gives the team an understanding of how well the child has grown relative to peers and their expected growth pattern. The consultant and SpR address any medical or health aspects that affect the child’s feeding and appetite.
Clinical Psychologist –Helps the child and family address the behavioural and emotional aspects of the feeding problems. The clinical psychologist may often provide separate psychological input to the child and/or family in addition to team input.
Dietician – assesses the child’s current diet and provides support and recommendations to ensure the child’s nutritional intake (quantity as well as variety) is optimal. The dietician may recommend supplements or meal replacement formulas, information on different textures of food and ideas for introducing new foods.
Speech and Language Therapist – the Speech and Language therapist (SALT) works with the team on a needs basis only and therefore will not attend every clinic. The SALT assesses the child’s oral and motor feeding skills, documents clinical signs of swallowing dysfunction, and recommends any further diagnostic medial testing and goals to encourage the development of oral motor skills. Administration – the feeding clinic secretary maintains all the feeding clinic files, types clinic letters, books patients in to the clinic and takes care of all our other general admin requirements.
Operation of the Feeding Clinic
Feeding Clinic
All team members (except SALT unless requested) meet every Thursday from 9.30am – 12.30pm (approximately) at Outpatients.
Referrals Referrals are discussed in clinic by as many members of the team as possible.
Assessments First assessment appointments are given 1 hour. Parents/carers have already received an information leaflet about the clinic and what to expect at their first appointment.
Each team member introduces themselves and takes it in turn to ask relevant questions. Generally the paediatrician starts, then the dietician, then the psychologist. The assistant psychologist will keep notes of the session and if required play with the child. Once sufficient information has been gathered, the family are asked to leave the room for five minutes to allow the team time to discuss an action plan. The family are invited back in to discuss and agree on the plan.
Follow-Up Following an initial assessment, most families are seen at home by the assistant psychologist to video a meal time, which is reviewed with the parents/carers by the Clinical Psychologist. Thereafter follow-up appointments are offered by the Clinical Psychologist and in the clinic. Families are also followed up by the dietician outwith the clinic, often by telephone. Copyright © Yorkhill Dietitians NHS Greater Glasgow and Clyde, 2013. Patient Records and Files Each child has a feeding clinic file (kept in the dietetics department), a psychology file (kept in the Clinical Psychology Dept) and a medical file (kept in medical records). The feeding clinic secretary makes copies of all correspondence so that each file is kept up to date.
Any follow-up sessions, phone calls or discussions outwith the clinic are recorded on a Feeding Clinic Contact sheet and e-mailed round the team so everyone is kept informed. This is a key part of team work. It is essential that any contact is communicated with the whole team.
Copyright © Yorkhill Dietitians NHS Greater Glasgow and Clyde, 2013. Feeding Clinic Work Shadowing Experience -Aims & Objectives
Aim:
Aspect Initial Initial Objective Task / Action Type of Achievemen Self Joint Evidence t at Level 4 Assessme Assessme (Date & nt nt signature) 1) To be able to interpret growth Tutorial Plotted charts from Growth data patterns appropriately from the Growth charts tutorial feeding clinic growth data Discussion around package feeding clinic growth 2) To gain a knowledge of when data skinfold measurements would be helpful. Appropriateness 1) To gain a clear understanding Discussion Evidence of clear of Nutritional of when it is appropriate to exit plan for children support start tube feeding with a child started on nutritional who has a safe swallow. support 2) Understand what should be achieved with tube feeding Weaning of 1) Gain an understanding of how Attendance at pt notes - Evidence supplemental and when it is appropriate to clinic of clear exit plan for feeds wean from feeds or sessions children started on supplements nutritional support Common feeding Knowledge of common feeding Shadow discussion issues problems such as food refusal and clinical way to help parents manage these psychologist / problems assistant psychologist
Reading list: Outpatient tube weaning in Glasgow: how fast do we progress and what stops us? (Abstract) Riddell K, Wright C M
Wright CM, Smith KH, Morrison J. Withdrawing feeds from children on long term enteral feeding: factors associated with success and failure. Arch Dis Child 2011; 96(5):433-439. Chillingworth, A; Wright, CM High energy oral supplements may suppress appetite without benefiting growth Archives of Disease in Childhood. 97(Suppl_1) (Supplement 1):A108, May 2012. https://www.infantandtoddlerforum.org/feeding-toddlers-topics
Copyright © Yorkhill Dietitians NHS Greater Glasgow and Clyde, 2013. Tube weaning group draft consensus statement /guideline
Starting long term tube feeding
If long term enteral feeding has been initiated, or where a child tube fed since the neonatal period is sent home on enteral feeding, the team who made that clinic decision should 1. Discuss with the family how long tube feeding is likely to continue and plan for future withdraw- al 2. Continue to actively manage the child’s feeds or find another clinical team willing to take this on
Maintenance 1. Continue oral stimulation and food tasting 2. Involve speech therapy 3. Ensure nutritional sufficiency (steady growth and fat stores stable and within normal range) but avoid over feeding and excess BMI gain
Stopping tube feeding
When to wean As soon as the child has 1. A clinically safe swallow 2. The oromotor maturity to allow consumption of purees (liquids?) 3. Tolerance of bolus feeds 4. Medically stable 5. BMI >2nd centile
How to wean Outpatient (slow) weaning In a child aged 6-18 months Make no further feed increases Once beginning to eat, make feeds reduction by 20% of peak feed volume Continue reductions as long as net weight gain continues In a child aged >18 months Reduce feeds by 20% Once beginning to eat, make further reductions of 20% of peak feed volume Make further reductions once there has been any weight gain, even if previous weight not attained All ages Move from night feeds to daytime boluses Offer small portions of purees and finger foods to taste and smell Offer boluses only after meals
When to refer to specialist team Children who are still not eating despite above regime Children with sustained weight loss on feed reduction Children with BMI <2nd percentile Parents unwilling to make or maintain feed reductions