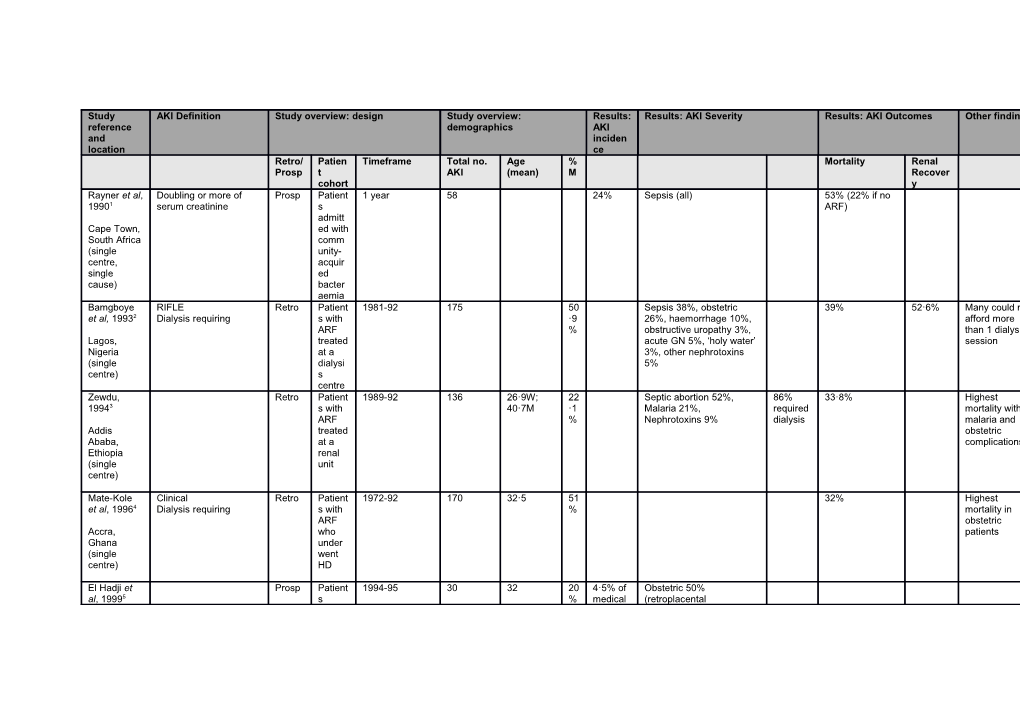
Study AKI Definition Study overview: design Study overview: Results: Results: AKI Severity Results: AKI Outcomes Other findings reference demographics AKI and inciden location ce Retro/ Patien Timeframe Total no. Age % Mortality Renal Prosp t AKI (mean) M Recover cohort y Rayner et al, Doubling or more of Prosp Patient 1 year 58 24% Sepsis (all) 53% (22% if no 19901 serum creatinine s ARF) admitt Cape Town, ed with South Africa comm (single unity- centre, acquir single ed cause) bacter aemia Bamgboye RIFLE Retro Patient 1981-92 175 50 Sepsis 38%, obstetric 39% 52·6% Many could not et al, 19932 Dialysis requiring s with ·9 26%, haemorrhage 10%, afford more ARF % obstructive uropathy 3%, than 1 dialysis Lagos, treated acute GN 5%, ‘holy water’ session Nigeria at a 3%, other nephrotoxins (single dialysi 5% centre) s centre Zewdu, Retro Patient 1989-92 136 26·9W; 22 Septic abortion 52%, 86% 33·8% Highest 19943 s with 40·7M ·1 Malaria 21%, required mortality with ARF % Nephrotoxins 9% dialysis malaria and Addis treated obstetric Ababa, at a complications Ethiopia renal (single unit centre)
Mate-Kole Clinical Retro Patient 1972-92 170 32·5 51 32% Highest et al, 19964 Dialysis requiring s with % mortality in ARF obstetric Accra, who patients Ghana under (single went centre) HD
El Hadji et Prosp Patient 1994-95 30 32 20 4·5% of Obstetric 50% al, 19995 s % medical (retroplacental referre admissio haematoma 66·7%, Dakar, d to a ns eclampsia 20%, other: Senegal (2 medica abortion, peripartum centres) l clinic haemorrhage) and an Medical 36% (malaria ICU 55%) with Surgical 14% ARF Mtika et al, Dialysis requiring Retro Patient 1998-00 21 50 20026 s % requiri Lilongwe, ng HD Malawi (single centre) Luyckx et al, elevated serum urea Retro Patient 78 Pre-renal 27%, ATN 27%, 41% Higher if HIV vs. 20057 and creatinine above s with Hepatorenal Syndrome non-HIV normal range, persistent ARF 6%, UTI 8%, Primary renal Johannesbu oligoanuria, worsening second disease 8% rg, South renal function with time, ary to Africa or need for dialysis folk (single remed centre, y use single cause)
Bah et al, Acute increase in Retro All 1999-03 46 44 60 21% 60% ‘had 20068 creatinine renal ·2 consumed admiss % decoctions of Conakry ions leaves and University roots’ prior to Hospital, presentation Mali (single centre) 14% had been to health centre Kaballo et Sudden rise in Retro Patient 2003-04 89 39 64 37% ATN secondary to 18% 60% al, 20079 creatinine to > 3mg/dL s who % volume depletion, in patients who had no under infections (inc. malaria and Khartoum, history of previous renal went typhoid fever), or Sudan impairment and who dialysi snakebites (single then required renal s for 13% ATN secondary to centre) replacement ARF paraphenylene-diamine (hair dye) suicide attempts 12% obstructive uropathy 9% glomerular disease
Arogundade Rapid increase in urea Prosp Patient 1998-02 46 38·2 73 Gastroenteritis 36·9% 43·5% No difference in et al, 200710 >10mmol/L; increase s ·9 Sepsis 30·5% outcome PD vs. creatinine > 260umol/L underg % HD Osun State, + clinical oing Nigeria Dialysis requiring renal (single replac centre) ement (HD and PD) for ARF El Imam et On ‘the basis of clinical Retro Patient 2007-08 94 34 75 90% of 31% al, 200911 and laboratory findings’ s % ARF admitt required Gezira ed to a RRT Hospital, renal (peritone Sudan unit al (single with dialysis) centre, ARF single second cause) ary to Rift Valley Fever (RVF) Friederickse Serum creatinine level Retro Patient 2003-04 46 44·4 60 23% ATN 82%, acute GN 49% (vs. 17% if 6·5% HIV n et al, >177 µmol/l, or a s with % 8·6%, malignant HTN no ARF) 200912 twofold increase in ARF 6·5%, vasculitis 2·2% baseline serum presen Cape Town, creatinine ting to South Africa ICU (single centre) Eghan et al, Dialysis requiring Retro Patient 2006-07 6 28·7 33 200913 s % underg Kumasi, oing Ghana HD at (single a new centre) unit Lengani et Acute onset renal Retro Patient 2004-06 121 38·6 62 18·4% Pre-renal 36% 24% Co-morbidities: al, 201014 impairment, creatinine s % (of Renal 47% Heart failure >240umol/L admitt medical Obstruction 12% 11% Burkina ed with admissio HTN 11% Faso (single ARF ns) Liver failure 7% centre) Malignancy 3%
10% NSAIDS and 21·5% herbs pre hospital
Dialysis provided in 14/84 (17%) Okpechi et Acute presentation Retro All 2000-10 274 36·8 45 21·3% Acute tubular necrosis al, 201115 associated with renal native ·2 of all 23·4% impairment kidney % biopsies HIVAN 15·0% Cape Town, biopsie were for Lupus nephritis 14·2% South Africa s ARF Acute interstitial nephritis (single undert 6·6% centre) aken Hypertensive nephroangiosclerosis 6·6% Crescentic GN 5·1% Post-infectious GN 4·4% Diabetic nephropathy 4·0% Mesangial proliferative GN 3·3% Mesangiocapillary GN 2·9% IgAN 1·8% Chronic interstitial nephritis 1·5%
Arendse et Patients requiring acute Retro HIV 2002-07 117 34 53 ATN (58%) 41% 33% 100% HIV al, 201116 HD positiv (median) ·5 93·2% black e % Cape Town, patient South Africa s who (single under centre) went HD Ekrikpo et Dialysis requiring Retro Patient 2008-09 14 57 Main predictor al, 201117 s % of mortality underg inability to pay Uyo, Nigeria oing for HD (single HD centre) Emem- ADQI/RIFLE Retro Patient 1996-99 and 62 41·3 55 1·9% Medical 71% 51% of 43·5% Chioma et Dialysis requiring s 2007-09 % admissio Sepsis 22·7%, acute GN AKI al, 201218 underg ns 20·5%, GE 16%, toxinx required oing 11·4% HD Port HD for Harcourt, AKI Nigeria (single centre) Chijioke et RIFLE Retro Patient 1989-09 138 29·4 42 Sepsis 36% 13·3% Mean number al, 201219 Dialysis requiring s who % Acute GN 16% HD sessions under Septic abortion 12% 2·24 Ilorin, went Toxin 11% Nigeria HD for GE 8% Mean LOS 20·1 (single ARF Post partum haemorrhage days centre) 8% Drug 4% Eclampsia 2% Other 7%
Okunola et AKIN Retro Patient 2005-10 45 33·7 53 Sepsis 36%, Obstetric 28·8% Major cause of al, 2012 and Dialysis requiring s who % related (pre-eclampsia, mortality pre- 201320,21 under septic abortion, post- eclampsia went partum haemorrhage) Osogbo, HD for 27%, Nephrotoxins 18%, Nigeria AKI Diarrhoea 9%, Acute GN (single 7%, Snake bite 2%, centre) Rhabdomyolysis (burns) 2%
Kilonzo et Renal impairment Retro Patient 2009-11 16 adults 33·9 56 ATN 45% 20% 20% used al, 201222 requiring dialysis and s who (4 % GN 25% traditional [see also history/clinical under children) Eclampsia/HELLP 10% medicaiotns Carter et al, investigations went HUS 5% 201223 and suggestive of AKI PD for Rhabdomyolysis 5% Callegari et AKI al, 201324]
Moshi, Tanzania (single centre)
Vachiat et RIFLE Retro HIV 2005-06 78 37 (vs· 45 56 Sepsis 63% (43% if HIV 44% (vs. 47% if al, 201325 patient if HIV NR % NR) HIV NR) s AKI) Haemodynamic instability Johannesbu presen 17% rg, South ting Toxin 6% Africa with Obstruction 5% (single renal centre) failure Phillips et al, Prosp Investi On medical wards Assessment of: 201326 gation infection commonest Renal function of AKI reason for admission (in 51-100% Ethiopia (3 risk particular TB and other Urine output 6- centres – 1 factor infections related to HIV) 20% urban, 2 assess Urine dip 30- rural) ment 57% in BP 61-98% medica l, Assessment of surgica risk factors for l and AKI lacking in obstetr up to 23% ic inpatie nts Riley et al, AKIN Prosp All 6/52 (July- 23 49·6 (vs· 61 15·2% Sepsis (inc malaria) 35%, Stage 1 8·2% (vs· 7·8% 38% 68% of total 201327 admiss August 2012) 41 if no % Cardiac disease 35%, 30% if no renal persisten population had ions to AKI) Obstetric related 10%, Stage 2 impairment) t renal renal function University of hospita Primary renal disease 22% injury at measured – Gondar l (not (pyelonephritis, nephrotic Stage 3 discharg prevalence Hospital, all syndrome, post-strep GN, 48% e renal Ethiopia screen renal vein thrombosis) impairment (single ed) 20% 19·8% centre; rural) LOS 11 days (AKI = no AKI)
Skinner et RIFLE Retro Patient 2008-11 102 39 15% 57% AKI al, 201428 s independent admitt predictor of Durban, ed to mortality South Africa trauma (single ICU centre) with AKI Tshamba et Dialysis requiring Prosp Rando 2012 18 34% of Association of al, 201429 m patients death with selecti on HD interruption in Lumbashi, on of treatment (due DRC (single patient to finances) centre) s underg oing HD Okaka et al, Dialysis requiring Retro Patient 2004-11 241 38·9M 60 19% of Sepsis commonest cause 201430 s 33·1F ·9 patients underg % on HD Benin, oing Nigeria HD (single centre) Oluyombo et Dialysis requiring Retro Patient 2010-13 26 38·1 67 14·8% al, 201431 s % of underg patients Ido-Ekiti, oing on HD Nigeria HD (single centre) Bagasha et AKIN Prosp Patient 63 37 55 16% Stage 1 21% 59% Co-morbidity: al, 201532 s ·6 29% persisten HIV 61% admitt % Stage 2 t renal HTN 4% Kampala, ed with 24% injury at Uganda sepsis Stage 3 2/52 25% herbal (single to ER 46% medication prior centre, and to admission single medica cause) l wards No HD available (all screen ed) Kaze et al, RIFLE Retro Patient 2005-10 63 44·8 58 28% of ‘PARENCHYMAL’ Co-morbidities: 201533 s ·7 renal 58·7% HIV 15·9% admitt % admissio -ATN 59% (malaria 36%, HTN 11·8% Yaounde, ed to a ns sepsis 23%, drugs 18·2%, DM 7·9% Cameroon renal eclampsia 13·6%, herbal (single unit remedy 9%) centre) -AIN 19% (drug induced 57%, infectious 29%, lymphoma 14%) -Acute GN 11% (post- infective 100%) -Vascular 11% (malignant HTN 50%, ANCA vasculitis 50%)
‘FUNCTIONAL’ 25·4% Enterocolitis 56%, Heart failure 31·3%, digestive haemorrhage 12·5%)
‘OBSTRUCTIVE’ 15·9% Prostate hypertrophy 60%, nephrolithiasis 20%, cervical cancer 20%
Table S3: Summary of AKI studies undertaken in sub-Sahara Africa (SSA) published from 1990-2015
References:
1. Rayner BL, Willcox PA, Pascoe MD. Acute renal failure in community-acquired bacteraemia. Nephron. 1990;54(1):32–5.
2. Bamgboye EL, Mabayoje MO, Odutola TA, Mabadeje AF. Acute renal failure at the Lagos University Teaching Hospital: a 10-year review. Ren Fail. 1993;15(1):77–80.
3. Zewdu W. Acute renal failure in Addis Abeba, Ethiopia: a prospective study of 136 patients. Ethiop Med J. 1994 Apr;32(2):79–87.
4. Mate-Kole MO, Yeboah ED, Affram RK, Ofori-Adjei D, Adu D. Hemodialysis in the treatment of acute renal failure in tropical Africa: a 20-year review at the Korle Bu Teaching Hospital, Accra.
Ren Fail. 1996 May;18(3):517–24.
5. El Hadji FK, Diouf B, Niang A, Ndiaye MF, Diop TM. Acute renal failure in adults in dakar. Saudi J Kidney Dis Transplant Off Publ Saudi Cent Organ Transplant Saudi Arab. 1999
Dec;10(4):513–4.
6. Mtika VG, Muula AS, Chipolombwe J, Nyirongo J, Rajabu J. Renal replacement therapy at Lilongwe Central Hospital, Malawi. Trop Doct. 2002 Jul;32(3):163–5.
7. Luyckx VA, Steenkamp V, Stewart MJ. Acute renal failure associated with the use of traditional folk remedies in South Africa. Ren Fail. 2005;27(1):35–43.
8. Bah AO, Kaba ML, Diallo MB, Kake A, Balde MC, Keita K, et al. [Renal diseases--morbidity and mortality in Nephrology Service, National Hospital Donka]. Mali Méd. 2006;21(4):42–6. 9. Kaballo BG, Khogali MS, Khalifa EH, Khaiii EAG, Ei-Hassan AM, Abu-Aisha H. Patterns of ‘severe acute renal failure’ in a referral center in Sudan: excluding intensive care and major surgery
patients. Saudi J Kidney Dis Transplant Off Publ Saudi Cent Organ Transplant Saudi Arab. 2007 Jun;18(2):220–5.
10. Arogundade FA, Sanusi AA, Okunola OO, Soyinka FO, Ojo OE, Akinsola A. Acute renal failure (ARF) in developing countries: which factors actually influence survival. Cent Afr J Med. 2007
Aug;53(5–8):34–9.
11. El Imam M, El Sabiq M, Omran M, Abdalkareem A, El Gaili Mohamed MA, Elbashir A, et al. Acute renal failure associated with the Rift Valley fever: a single center study. Saudi J Kidney Dis
Transplant Off Publ Saudi Cent Organ Transplant Saudi Arab. 2009 Nov;20(6):1047–52.
12. Friedericksen DV, Van der Merwe L, Hattingh TL, Nel DG, Moosa MR. Acute renal failure in the medical ICU still predictive of high mortality. South Afr Med J Suid-Afr Tydskr Vir Geneeskd.
2009 Dec;99(12):873–5.
13. Eghan BA, Amoako-Atta K, Kankam CA, Nsiah-Asare A. Survival pattern of hemodialysis patients in Kumasi, Ghana: a summary of forty patients initiated on hemodialysis at a new
hemodialysis unit. Hemodial Int Int Symp Home Hemodial. 2009 Oct;13(4):467–71.
14. Lengani A, Kargougou D, Fogazzi GB, Laville M. [Acute renal failure in Burkina Faso]. Néphrologie Thérapeutique. 2010 Feb;6(1):28–34.
15. Okpechi I, Swanepoel C, Duffield M, Mahala B, Wearne N, Alagbe S, et al. Patterns of renal disease in Cape Town South Africa: a 10-year review of a single-centre renal biopsy database.
Nephrol Dial Transplant. 2011 Jan 6;26(6):1853–61.
16. Arendse C, Okpechi I, Swanepoel C. Acute dialysis in HIV-positive patients in Cape Town, South Africa. Nephrol Carlton Vic. 2011 Jan;16(1):39–44.
17. Ekrikpo UE, Udo AI, Ikpeme EE, Effa EE. Haemodialysis in an emerging centre in a developing country: a two year review and predictors of mortality. BMC Nephrol. 2011;12:50.
18. Emem-Chioma PC, Alasia DD, Wokoma FS. Clinical outcomes of dialysis-treated acute kidney injury patients at the university of port harcourt teaching hospital, Nigeria. ISRN Nephrol.
2013;2013:540526.
19. Chijioke A, Makusidi AM, Rafiu MO. Factors influencing hemodialysis and outcome in severe acute renal failure from Ilorin, Nigeria. Saudi J Kidney Dis Transplant Off Publ Saudi Cent Organ
Transplant Saudi Arab. 2012 Mar;23(2):391–6.
20. Okunola Y, Ayodele O, Akinwusi P, Gbadegesin B, Oluyombo R. Haemodialysis practice in a resource-limited setting in the tropics. Ghana Med J. 2013 Mar;47(1):4–9.
21. Okunola OO, Ayodele OE, Adekanle AD. Acute kidney injury requiring hemodialysis in the tropics. Saudi J Kidney Dis Transplant Off Publ Saudi Cent Organ Transplant Saudi Arab. 2012
Nov;23(6):1315–9.
22. Kilonzo KG, Ghosh S, Temu SA, Maro V, Callegari J, Carter M, et al. Outcome of acute peritoneal dialysis in northern Tanzania. Perit Dial Int J Int Soc Perit Dial. 2012 Jun;32(3):261–6. 23. Carter M, Kilonzo K, Odiit A, Kalyesubula R, Kotanko P, Levin NW, et al. Acute peritoneal dialysis treatment programs for countries of the East African community. Blood Purif. 2012;33(1–
3):149–52.
24. Callegari J, Antwi S, Wystrychowski G, Zukowska-Szczechowska E, Levin NW, Carter M. Peritoneal dialysis as a mode of treatment for acute kidney injury in sub-Saharan Africa. Blood Purif.
2013;36(3–4):226–30.
25. Vachiat AI, Musenge E, Wadee S, Naicker S. Renal failure in HIV-positive patients—a South African experience. Clin Kidney J. 2013 Dec;6(6):584–9.
26. Phillips LA, Allen N, Phillips B, Abera A, Diro E, Riley S, et al. Acute kidney injury risk factor recognition in three teaching hospitals in Ethiopia. South Afr Med J Suid-Afr Tydskr Vir Geneeskd.
2013 Jun;103(6):413–8.
27. Riley S, Diro E, Batchelor P, Abebe A, Amsalu A, Tadesse Y, et al. Renal impairment among acute hospital admissions in a rural Ethiopian hospital. Nephrol Carlton Vic. 2013 Feb;18(2):92–6.
28. Skinner DL, Hardcastle TC, Rodseth RN, Muckart DJJ. The incidence and outcomes of acute kidney injury amongst patients admitted to a level I trauma unit. Injury. 2014 Jan;45(1):259–64.
29. Tshamba HM, Van Caillie D, Nawej FN, Kapend FM, Kaj FM, Yav GD, et al. Risk of death and the economic accessibility at the dialysis therapy for the renal insufficient patients in Lubumbashi
city, Democratic Republic of Congo. Pan Afr Med J [Internet]. 2014 Sep 23 [cited 2016 Apr 7];19. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4317069/
30. Okaka EI, Unuigbe EI. Eight year review of hemodialysis: treated patients in a tertiary center in Southern Nigeria. Ann Afr Med. 2014 Dec;13(4):221–5.
31. Oluyombo R, Okunola OO, Olanrewaju TO, Soje MO, Obajolowo OO, Ayorinde MA. Challenges of hemodialysis in a new renal care center: call for sustainability and improved outcome. Int J
Nephrol Renov Dis. 2014;7:347–52.
32. Bagasha P, Nakwagala F, Kwizera A, Ssekasanvu E, Kalyesubula R. Acute kidney injury among adult patients with sepsis in a low-income country: clinical patterns and short-term outcomes.
BMC Nephrol. 2015;16:4.
33. Kaze FF, Ekokobe FE, Halle MP, Fouda H, Menanga AP, Ashuntantang G. The clinical pattern of renal diseases in the nephrology in-patient unit of the Yaounde General Hospital in
Cameroon: a five-year audit. Pan Afr Med J [Internet]. 2015 Jul 20 [cited 2016 Apr 1];21. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4575702/