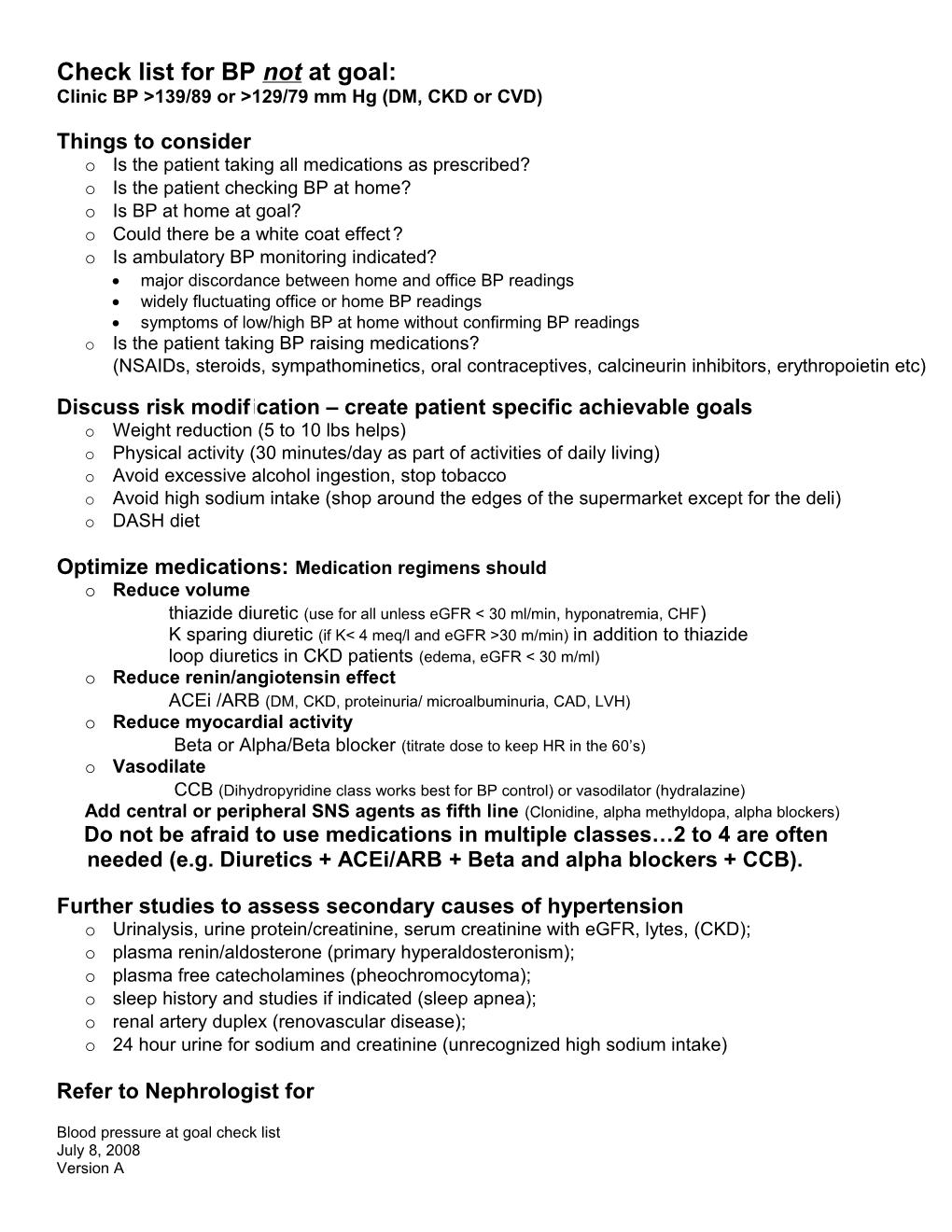
Check list for BP not at goal: Clinic BP >139/89 or >129/79 mm Hg (DM, CKD or CVD)
Things to consider o Is the patient taking all medications as prescribed? o Is the patient checking BP at home? o Is BP at home at goal? o Could there be a white coat effect? o Is ambulatory BP monitoring indicated? major discordance between home and office BP readings widely fluctuating office or home BP readings symptoms of low/high BP at home without confirming BP readings o Is the patient taking BP raising medications? (NSAIDs, steroids, sympathominetics, oral contraceptives, calcineurin inhibitors, erythropoietin etc) Discuss risk modification – create patient specific achievable goals o Weight reduction (5 to 10 lbs helps) o Physical activity (30 minutes/day as part of activities of daily living) o Avoid excessive alcohol ingestion, stop tobacco o Avoid high sodium intake (shop around the edges of the supermarket except for the deli) o DASH diet
Optimize medications: Medication regimens should o Reduce volume thiazide diuretic (use for all unless eGFR < 30 ml/min, hyponatremia, CHF) K sparing diuretic (if K< 4 meq/l and eGFR >30 m/min) in addition to thiazide loop diuretics in CKD patients (edema, eGFR < 30 m/ml) o Reduce renin/angiotensin effect ACEi /ARB (DM, CKD, proteinuria/ microalbuminuria, CAD, LVH) o Reduce myocardial activity Beta or Alpha/Beta blocker (titrate dose to keep HR in the 60’s) o Vasodilate CCB (Dihydropyridine class works best for BP control) or vasodilator (hydralazine) Add central or peripheral SNS agents as fifth line (Clonidine, alpha methyldopa, alpha blockers) Do not be afraid to use medications in multiple classes…2 to 4 are often needed (e.g. Diuretics + ACEi/ARB + Beta and alpha blockers + CCB).
Further studies to assess secondary causes of hypertension o Urinalysis, urine protein/creatinine, serum creatinine with eGFR, lytes, (CKD); o plasma renin/aldosterone (primary hyperaldosteronism); o plasma free catecholamines (pheochromocytoma); o sleep history and studies if indicated (sleep apnea); o renal artery duplex (renovascular disease); o 24 hour urine for sodium and creatinine (unrecognized high sodium intake)
Refer to Nephrologist for
Blood pressure at goal check list July 8, 2008 Version A suspected or known secondary cause(s) of hypertension and/or CKD uncontrolled BP after 6 -12 months of treatment
Blood pressure at goal check list July 8, 2008 Version A