APPENDIX 2:INPATIENT REHABILIATION UNIT SERVICE SPECIFICATION
SCHEDULE 2
THE SERVICES
Schedule 2 Part 1: Service Specifications
Mandatory headings Sections 1-3. Mandatory but detail for local determination and agreement. Optional headings Sections 4-6. Optional to use, detail for local determination and agreement. Subheadings for local determination and agreement] SERVICE SPECIFICATION
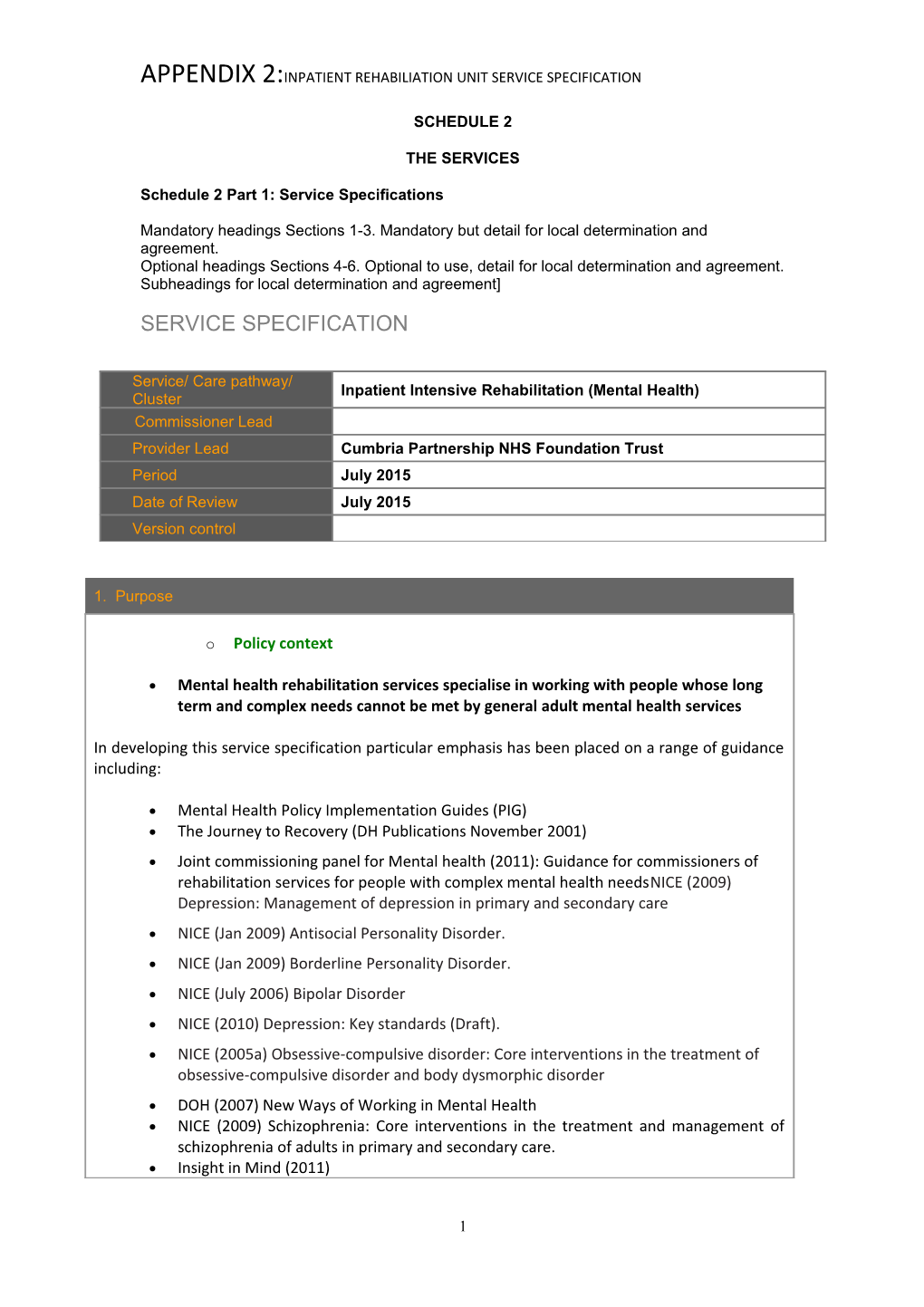
Service/ Care pathway/ Inpatient Intensive Rehabilitation (Mental Health) Cluster Commissioner Lead Provider Lead Cumbria Partnership NHS Foundation Trust Period July 2015 Date of Review July 2015 Version control
1. Purpose
o Policy context
Mental health rehabilitation services specialise in working with people whose long term and complex needs cannot be met by general adult mental health services
In developing this service specification particular emphasis has been placed on a range of guidance including:
Mental Health Policy Implementation Guides (PIG) The Journey to Recovery (DH Publications November 2001) Joint commissioning panel for Mental health (2011): Guidance for commissioners of rehabilitation services for people with complex mental health needsNICE (2009) Depression: Management of depression in primary and secondary care NICE (Jan 2009) Antisocial Personality Disorder. NICE (Jan 2009) Borderline Personality Disorder. NICE (July 2006) Bipolar Disorder NICE (2010) Depression: Key standards (Draft). NICE (2005a) Obsessive-compulsive disorder: Core interventions in the treatment of obsessive-compulsive disorder and body dysmorphic disorder DOH (2007) New Ways of Working in Mental Health NICE (2009) Schizophrenia: Core interventions in the treatment and management of schizophrenia of adults in primary and secondary care. Insight in Mind (2011)
1 Enabling recovery for people with complex mental health needs (2009 NICE (2004a) & (Jan 2011) Anxiety: Management of anxiety (panic disorder, with or without agoraphobia, and generalised anxiety disorder) in adults in primary, secondary and community care DOH (2001) Choosing Talking Therapies No Health Without Mental Health: (HM Gov 2011) Dr Frank Holloway et al, Royal college of psychiatrists (2005)Chair of the Faculty of Rehabilitation and Social Psychiatry – The Forgotten Need for Rehabilitation in Contemporary Mental Health Services: A position statement from the Executive Committee of the Faculty of Rehabilitation and Social Psychiatry NIMHE (2003) Personality Disorder; No Longer a Diagnosis of Exclusion. Organising and Delivering Psychological Therapies, DOH 2004 Tony Ryan Associates Review of Cumbrian Rehabilitation Services (November 2012) Implementation of ‘Refocusing the Care Programme Approach’ (DH 2008) Meeting the needs of those with mental illness, addressing inequalities, tackling problems of stigma and discrimination, social exclusion and promoting positive risk management Cumbria mental health cluster pathways Related guidance and clinical guidelines such as achieving the National Suicide Prevention Strategy
1.2 Local strategic context
The Joint Commissioning Panel for Mental Health state : Mental health rehabilitation services specialise in working with people whose long term and complex needs cannot be met by general adult mental health services.
Rehabilitation services are not the same as recovery services.
There is an ongoing need for specialist rehabilitation services
People using rehabilitation services are a ‘low volume, high needs’ group:
People with complex mental health problems often require a large proportion of mental health resources.
There is good evidence that rehabilitation services are effective.
Investment in a local rehabilitation care pathway is cost effective.
Commissioning a “good” rehabilitation service includes components of care provided by the NHS,
2 APPENDIX 2:INPATIENT REHABILIATION UNIT SERVICE SPECIFICATION independent and voluntary sector.
Mental health rehabilitation services require multidisciplinary staffing.
The quality and effectiveness of rehabilitation service provision can be assessed with simple indicators and standardised outcome tools. (Currently, in line with Joint Commissioning Panel recommendations, Acorn use the Camberwell Assessment of Needs Short Appraisal Schedule (CANSAS) and have begun preparatory work to become AIMS – Rehab accredited)
1.3 Aims and objectives of the service
To provide hospital based intensive rehabilitation which will form part of the proposed end-to-end rehabilitation pathway from acute and secure services to community living. To maximise the rehabilitation offer in county and to support out of area placements due to capacity or clinical need The unit will be able to work with individuals who are there both voluntarily, as well as those detained under the Mental Health Act (2007). The principles/policies on which the foundations of the unit are built should echo the core principles arising from evidenced based theories of recovery and social inclusion within a framework of therapeutic optimism. To support the continuation of comprehensive treatment from the hospital based Intensive Rehabilitation Service (IRS). This will follow established pathways of care which will meet the needs of the service user for community living. To ensure seamless transition between hospital and stepped down community mental health services delivered by care pathway workers to ensure continuity of care, treatment and management of condition and risk.
The support of flexible recovery practitioners will address the gap in provision between an inpatient unit and supported housing schemes which can often result in relapse or increase of mental health symptoms and an increase in social isolation. The trust and support built between inpatient and community is vital to ensure a productive and sustained discharge from hospital. This model is supported by key guidance documents as well as the recent Cumbria Rehabilitation Review.
The objectives for achieving this will be: Offer high quality, evidence based inpatient rehabilitation and recovery based treatment focusing on those individuals suffering with severe functional impairments as a consequence of severe mental health issues Provide short term, targeted transition for each client in order to support the step down of individuals from hospital based units into less dependent community settings Offer expert consultation to acute mental health services in the management of treatment resistance, thereby capacity building within the wider workforce Provide expert assessment for decisions about placement within the rehabilitation pathway Provide expert advice on the development of complex packages of community care and support. To support services users, family and carers in the promotion of recovery
3 To work within the pan-Cumbrian MDO framework To reduce hospital admissions and length of stay wherever possible To improve social functioning and inclusion, facilitate personal growth and provide opportunities for personal fulfilment and recovery To provide a service that is sensitive and responsive to service users’ cultural, religious and gender needs To promote effective interagency working To ensure effective risk assessment and safe management of risk. Compliance with Cumbria’s Area Prescribing committee guidelines on shared care prescribing & monitoring Promote health and wellbeing as an essential part of treatment Provide cost effective solutions for the support and treatment of individuals with severe and enduring mental illness
2. Service Scope
2.1 Service user groups covered The current profile of service users accessing intensive rehabilitation services, in general, shows that:
80% are male and aged between 20 and 40 20% are female aged between 20 and 40 Their risk history profile includes challenging and chaotic lifestyles including risky and impulsive behaviours and forensic history. Non-compliance is a feature together with disengagement from services Mental health is highly symptomatic Dual diagnosis with either alcohol or substance misuse is evident in some service users The Client group have high vulnerability
Referrals into the service will be accepted from CPFT inpatient acute units, community mental health services and secure services.
The intensive rehabilitation service (IRS) will provide comprehensive assessment where the service user will either be accepted into the service or recommendations made for on-going care. This will follow established pathways of care which will meet the needs of the service user either ‘stepped down’ for community living or ‘stepped up’ for more secure services. Transitions between hospital (IRS) and community mental health services will ensure continuity of care, treatment and management of condition and risk.
2.2 Current admission criteria for admission to Acorn
Current criteria for admission to Acorn Centre:
• Male
• Over the age of 18
• A diagnosis of mental illness with complexity in terms of:
4 APPENDIX 2:INPATIENT REHABILIATION UNIT SERVICE SPECIFICATION o Usually a primary diagnosis of psychotic disorder (schizophrenia, schizoaffective or bipolar disorder) o Other comorbidities such as substance misuse, depression, anxiety, personality disorder, poor physical health o Poor response to or engagement with treatment
• Difficulty in managing in the community in one or more of the following areas: o Staying safe and well o Managing symptoms and preventing relapse o Maintaining a tenancy o Self-care o Maintaining relationships o Having a satisfying and meaningful daily routine o Being motivated o Having capacity to and the support to make choices o Managing finances
• Where less intensive interventions have either been tried and been unsuccessful or where the costs of a failure would be high (in terms of personal motivation and hope, or in terms of risk to self and others) and where there is clinical evidence to suggest a high likelihood of failure
2.3 Service description
The service is an intensive inpatient rehabilitation unit, with a high level of integrated, registered professionals to make up a multi-disciplinary team. The unit will be able to manage individuals who may be detained and /or behaviourally disturbed and highly symptomatic.
Anticipated length of stay is between 12-24 months with individuals stepping down to appropriate commissioned community rehabilitation services/community living.
Care will take a whole system approach with practitioners communicating regularly with each other, other agencies and with service users, family and carers where appropriate in relation to treatment planning. The service will be provided by a consistent group of staff with whom it is possible for the service user to develop a trusting relationship. This staff group will provide a flexible approach during admission and discharge to ensure smooth transition from inpatient to community living. Acorn are utilising a legacy approach to discharge, the transferring of our acquired in depth knowledge of individuals that is passed to Care Coordinators on discharge. Acorn work closely with 3rd sector providers and facilitate “side by side” training for organisations who will be working with discharged patients in order to assist providers in working effectively.
Referral standards
• We encourage early collaboration to ensure the best use of a limited resource and will work with referrers to ensure early dialogue for clinically appropriate assessments.
• Telephone consultation for referrers within 1 working day.
• Formal referral to decision to assessment within 1 working week.
5 • Completed assessment within 3 working weeks (in area).
• Completed assessment within 6 working weeks (out-of-area).
• The offer of a unit visit to patient and carer where clinically appropriate.
Admission standards
• Acorn will admit within 1 working week where bed availability and funding agreed.
• Admissions normally take place on Tuesdays to ensure safe handover and transition between clinical teams.
• Key working team identified via assessment process.
• Care plan and rehabilitation core assessment within 1st working week.
• Risk assessment (GRIST) updated within 24 hours.
• Medication reconciliation on admission.
• Physical health check on admission.
• An MDT will take place as a minimum every 6 weeks, to include care co-ordinator, service user and carers (more frequent if clinically required).
Discharge
• A Discharge Planning meeting is arranged before discharge.
• 117 meetings to take place in line with Trust policy.
• Legacy documents to support future planning.
• Specific individualised training to support continued progress (where indicated).
• Support the facilitation of In reach with other support agencies who will provide follow-on care.
• A formative 12 week assessment with all professionals involved.
• On request, a follow-up professional consultation to maximise the success of move-on of placement.
Acorn 12 week Pathway
Referral form including: Reasons for requesting Acorn centre, current presentations, copy of current GRIST and Care Plan, other relevant reports e.g. OT assessments and community assessments Discussed in Triage Meeting & either declined or assigned to two assessors
Pre-admission Notes summary-This should include- psychosocial history; family and relationships; financial situation; functional skills; admissions to other wards; list of medications; risk and vulnerability; relapse indicators- including (early middle and late stage indicators); symptoms reported; work; education; interests; Capacity to consent and other capacity issues; legal status including leave. Current community situation. Assessment care plan- initial care planning based on goals identified in assessment;
6 APPENDIX 2:INPATIENT REHABILIATION UNIT SERVICE SPECIFICATION
general needs and process of transfer. Triage meeting- Assessment is presented and discussed, and final decision to accept is made by those present. If decision is to accept, the key team and key workers are assigned. Pre Assessment Meeting- Arranged in an MDT slot, led by key team (or key worker) – issues raised by assessment are discussed, transfer planning and any complicating factors.
Admission (This can be flexible but is preferred on a Tuesday or Wednesday p.m.)
Initial 48 hours: - Orientation & Introduction to ward– basic health checks etc. Admission Checklist - Introduce Key worker/Key OT etc.
Up to 2 Weeks: - Mental state assessed; physical health assessed; overt plans/goals identified and clarified; motivation assessed; environmental risk assessment; - HONOS & GRIST, CANSAS & CGT -Introduce Psychologist and assess possible needs for input. - Engagement with community care co-ordinator and any other providers
2 Week Review Meeting Led by key team and consultant
Develop initial rehabilitation formulation and Goals as a team and communicate with care co- ordinator Implement any bespoke measurement tools for progress Plan initial interventions based on information from first two weeks Identify missing information that is still required. Engage person in appropriate care plans: Valued Functional Clinica Physic Relationshi Perso Risk Activity Skills. e.g.: l al p and nal Manag e.g.: Self-care Needs Health Social Devel ement. -Social Finance . e.g.: Needs Needs: e.g. opme e.g. engagem Budget Medic . e.g.: Carers nt Relap ent Banking ation -GP support needs. se - Public manag and Family e.g. plans Volunteer Transport ement Dental contact Devel Vulner ing or suppor Wider oping ability -Creative review t social self manag activities sympt - contact identit ement om Health Social skills y Positiv relief y Therapy Educa e risk strateg eating intervention tion taking ies - s and and CBTp specifi vocati grade c onal d investi plans manag gation Enhan ement s cing of risk and mana ging capaci ty
2-10 weeks in depth assessment and interventions Undertake assessments and interventions as detailed in care plan Review progress and goals at weekly rehabilitation planning meeting and community care team Undertake team formulation meeting with key working team and psychologist Assess progress using CANSAS, CGT, Bespoke tools identified above and persons own report
10 Week Review meeting
7 MDT review of progress based on above, led by key team, care co-ordinator and consultant. 12 week progress review letter Developed by key team Review of data from measuring tools Recommendation agreed for discharge at 12 weeks or engagement with further rehabilitation (including rationale and goals.)
Request is sent to commissioners for further funding; Person continues with MDT review meetings 4-6 weekly; Rehab goals are reviewed in weekly planning meeting.
OR
Discharge pathway agreed and meeting planned for 12th week; Team complete summary assessment documentation to return to care co-ordinator.
3. Service Delivery
3.1 Location of service
The service is located on Carleton Clinic site. The unit will primarily treat service users with high clinical needs who will be undergoing treatment under the mental health framework. Close proximity to acute inpatient facilities and specialist mental health staff will be required at times to ensure safety and high quality care being provided and available for service users. The staff will work into the community to provide a socially inclusive approach and to provide transitional support to community services.
3.2 Days/ hours of operation
The service will be available 24 hours a day, 7 days a week.
3.3 Interventions
(i) Aim of interventions
Supporting client’s in establishing their life goals and for each of these determining the level of skills they need, or support required, for success with the minimum professional input in the longer term consistent with success improvement in functioning improved quality of life improved outcomes for clients in what they see as important, in their chosen area Changes to core beliefs where ingrained beliefs are detrimental to the service user achieving their goals.
Intervention will be based on thorough, holistic assessment and formulation with collaboratively agreed goals. There will be therapeutic review and goal planning on a weekly basis with formal comprehensive reviews at least every 6 weeks. Therapeutic sessions will be agreed with the service user/carer/family where appropriate.
All care should take a whole system approach with practitioners communicating regularly in relation to treatment planning.
8 APPENDIX 2:INPATIENT REHABILIATION UNIT SERVICE SPECIFICATION
For all assessments and treatment modalities, individuals with the most severe and complex difficulties will receive input from the most skilled practitioners for that modality. All interventions will be carried out by practitioners within their competencies with adequate support and supervision/consultation from the relevant profession.
Psychological therapies
Psychological therapies are part of essential health care. The term “psychological therapies” covers a wide range of different models. Psychologically informed care needs to be delivered as part of a well-coordinated multidisciplinary care plan agreed with the service user. Psychological therapy will be well structured and geared to achieving adherence. It will have a clear focus, be evidence based and theoretically coherent. Duration will be relatively long term , be well integrated with other services and have defined short and long term aims with a clear treatment alliance.
Therapeutic interventions (from an appropriately trained member of the mental health team) will consider the following:
o CBT, CAT and IPT, Behaviour therapy (BT), problem solving, DBT, motivational work, TFP, trauma focussed work, EMDR, SFT, psycho-educational, DBT informed skills group o Mindfulness o Systemic therapy o Considerations and suitable interventions when service user has dual diagnosis (Drugs/Alcohol) o Psychodynamic therapy may be considered for complex co-morbidities o For self-harm, assessment needs to include psychologically informed formulation. Consider self injury support group, survivors of sexual abuse group, DBT
All the above will be delivered by staff with specialist training and supervision.
Pharmacological interventions Will be delivered in line with Trust protocols which follow NICE guidelines and additional evidence in relation to prescribing. Occupational interventions Occupational assessment and treatment is based on the premise that occupational performance is a central force in health, wellbeing, development and change. Human occupation comprises three broad areas: self-care, productivity and leisure that are influenced by the three inter-related components: volition, habituation and performance capacity. The elements include:
Assessment of occupational functioning Identifying areas of occupational need Use of standardised assessment Consideration of social and environmental issues
Treatment, evaluation and discharge planning:
Collaborative treatment planning to address areas of occupational need Recommendations identified and discussed with individual, their family/carer where appropriate, GP and wider care team
9 Links to other providers regarding social and environmental requirements to support step down
The occupational practitioner will receive professional supervision.
Substance misuse
o Assessment of common co-morbidity: Dependence, harmful use, complications, motivation to change o Engagement with drug and alcohol services as required for consultation and continued work o Appropriate liaison for other relevant services eg. detox o Define ways of dealing with this alongside mental health issues, as per NICE guidelines. o Develop close links with drug and alcohol services
Physical health
Promote assessment and monitoring in partnership with GP:
o Generic review of physical health state, baseline bloods, preventative health opportunities, sexual health and physical disability issues o Supporting therapeutic interventions and assessment from specialist services where required (physiotherapy, dietetics, podiatry, speech and language) o Smoking cessation advice and referral where required o Physiotherapy specialist advice and support
Wellness, Nutrition, Exercise and mobility
Assessment and monitoring: o Generic review of physical health state, preventative health opportunities, mobility and physical disability issues
Enabling o Provision of information about community wellbeing activities o Liaison with and signposting to 3rd sector or statutory agencies
Therapeutic interventions o Supporting therapeutic interventions and assessment from specialist services where required o Physical health therapy (exercise) with dedicated physiotherapy o Social inclusion o Supporting family relationships o Social prescribing/personal budgets
Tools to support assessment and interventions
General: essential for assessment and management within care pathways including:
Assessment documentation Holistic Assessment- agreed with Service User/Carers when appropriate
10 APPENDIX 2:INPATIENT REHABILIATION UNIT SERVICE SPECIFICATION
CPA documentation Grist risk assessment HONOS plus Recovery star Physical health screening
Disorder and Clinical Discipline Specific Measures (guided by clinical assessment including:
CORE (Clinical Outcomes in Routine Evaluation) PHQ9 Beck Depression Inventory Beck Hopelessness scale Beck anxiety inventory F.R.A.S.E MMPI PDQ 4 Nutritional screening tool Medical alert system GASS side effect scale Shared care protocols where applicable Clozaril monitoring protocols if applicable MMSE ACE MOHOST (model of human occupation screening tool) OCAIRS (occupational circumstances assessment interview and rating scale) OPHI-II (occupational performance history interview) OSA (occupational self-assessment) Volitional questionnaire (VQ) Assessment of Communication and Interaction Skills (ACIS) AMPS (Assessment of motor and process skills) REIS – residential environmental impact scale
3.4 Outcomes Measures Use of specific outcome measures for aspects of treatment and other appropriate service user focused outcome measures as agreed.
Further to this , the service will develop: Physical Screening and Wellbeing Advice- physical health checks every 3 months or earlier if indicated Access to chronic disease monitoring and treatment programmes eg. for diabetes Smoking Cessation programmes Personalisation Agenda – Scope for Direct Payments Volunteering/Employment Assistance Help with Accommodation issues Access to employment support, training and educational opportunities. Compliance with NICE guidance Care Quality Commission Standards Compliance Service User and carer Charter document Easy access to relevant information and signposting. Compliance with anti-stigma and anti-discriminatory policies
11 Adherence to shared care guidelines AIMS – Rehab accreditation Embedding use of the CANSAS assessment tool Capturing patient stories on discharge Review of the Social Functioning Questionnaire (SFQ)
3.5 Training/ Education/ Research activities
Acorn will develop an Education and Training strategy which will include:
Training needs analysis and monitored Links to Key Skills Framework (KSF)and appraisal Mandatory training Links to Continuing Professional Development Links to Clinical Governance Content that is specific to service requirements. Learning environment for pre-registration Nurses and Occupational Therapists with identified Mentors and Preceptors
4. Quality Indicators including relevant CQUIN Indicators Quality Indicator(s) Method of Measurement/ Incentive or sanction information requirement % of people followed up within 7 >95% days of discharge % of people on CPA with a >90% housing status recorded % of people on CPA with an >90% employment status recorded All FCEs to have a valid ethnic >90% code % of FCEs with a valid diagnosis >90% % of people with a care co- >95% ordinator % of people with a care plan >95% marked as complete physical health and wellbeing checks minimum 3 monthly; use of shared care guidelines % of people with LD in mental health services having regular >95% physical health checks HoNOS recorded at initial 100% assessment HoNOS recorded at discharge 100%
Basis of Contract Unit of Price Thresholds Expected Annual Measurement Contract Value Block Arrangement/Cost and Volume £ £ Arrangement/Local Tariff/Non-Tariff Price______* Total £ £ *delete as appropriate
12 APPENDIX 2:INPATIENT REHABILIATION UNIT SERVICE SPECIFICATION
13