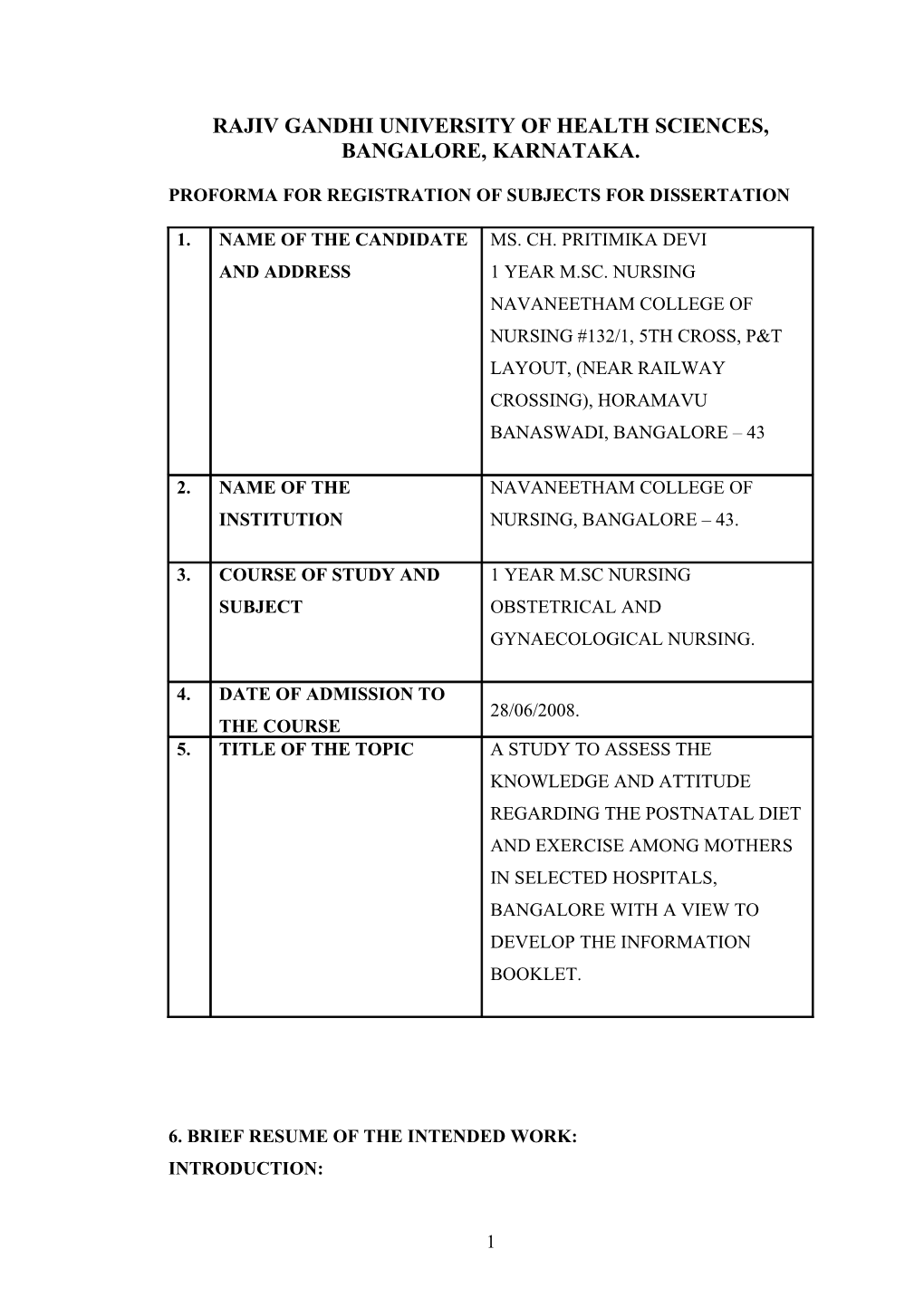
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES, BANGALORE, KARNATAKA.
PROFORMA FOR REGISTRATION OF SUBJECTS FOR DISSERTATION
1. NAME OF THE CANDIDATE MS. CH. PRITIMIKA DEVI AND ADDRESS 1 YEAR M.SC. NURSING NAVANEETHAM COLLEGE OF NURSING #132/1, 5TH CROSS, P&T LAYOUT, (NEAR RAILWAY CROSSING), HORAMAVU BANASWADI, BANGALORE – 43
2. NAME OF THE NAVANEETHAM COLLEGE OF INSTITUTION NURSING, BANGALORE – 43.
3. COURSE OF STUDY AND 1 YEAR M.SC NURSING SUBJECT OBSTETRICAL AND GYNAECOLOGICAL NURSING.
4. DATE OF ADMISSION TO 28/06/2008. THE COURSE 5. TITLE OF THE TOPIC A STUDY TO ASSESS THE KNOWLEDGE AND ATTITUDE REGARDING THE POSTNATAL DIET AND EXERCISE AMONG MOTHERS IN SELECTED HOSPITALS, BANGALORE WITH A VIEW TO DEVELOP THE INFORMATION BOOKLET.
6. BRIEF RESUME OF THE INTENDED WORK: INTRODUCTION:
1 In the past maternal and child heath services were fragmented and provided care separately by the different ways and separate health delivery services. After the introduction reproductive and child health concept and child survival and safe motherhood program the family welfare united the mother and child together in the form of maternal and child health. Mother and child are considered as one unit because during the antenatal period, the fetus part of the mother. But after the birth the child depend on the mother for at least 6 to 9 months. The post natal period is very important crucial period for the both mother and baby. The postnatal care of the mother include the following. 1. Prevent the postnatal complications. 2. Restoring the optimum health. 3. Exclusive breast feeding for the six months and weaning. 4. Family planning services. 5. Basic health education about hygiene and check up.1 In the above aspects of the care the restoration of the optimum health indicates the complete physical, mental and social wellbeing of the postnatal mothers. The broad areas fall in to this category was postnatal examination, anaemia, nutrition, postnatal exercise, promotion of psychological and social well being. The minor aliments some time major problem for the postnatal mother was the inadequate nutrition, urinary incontinence.1 Pregnancy and delivery takes its toll – both physical and emotional on the body. The post natal period is vital for the body to recover. A healthy nutritious diet is required both to recuperate and in view of breastfeeding. Trying to lose weight soon after delivery will only result in feeling more tired because breastfeeding is physiologically demanding and requires more calories. Moreover, breastfeeding will help to use up the fat accumulated during the pregnancy so is a healthier way to lose a little weight.1 Breastfeeding, apart from the numerous benefits it has for the baby, also relieves pain in the breasts which, due to hormonal changes, get engorged. A little lower abdominal cramping in response to breastfeeding is also normal and is a sign of the uterus getting back to its normal size. The nutritional needs of the postnatal mother include the both mother and baby nutritional requirements. The baby requires the nutritional demands for the fast growth and development of the infant period as well as the lactating mother require for the postnatal recovery.1
2 The ICMR reported that caloric requirement of the lactating mother was RDA + 550 K Calories first six months and + 400 K calories, protein requirement RDA+ 25g per day, 1000mg/dl and iron30mg/dl.2 The nutrition alone cannot make the recovery of the postnatal mother in to the pre pregnant state. The pelvic organs to recover into the normal state the postnatal exercise very important one to strengthen. The muscles and manage the minor ailments of the mother in the postnatal period.2 Exercise is important so much as to lose weight initially but to feel relaxed and get your body back to its pre pregnant state. Pelvic floor exercises are also important since the pelvic muscles get stretched and it’s necessary to tone them up the pelvic organs again. The exercise not only strengthens the pelvic floor muscles it helps relieve the constipation and reduce the postnatal depression. The postnatal exercises are deep breathing exercises, kegel exercises, exercises for the abdominal muscles and exercises for the back muscles.3 DEEP BREATHING: Breathing in slowly and deeply, the air is allowed to expand the lungs as far as possible. Then it is let out slowly. Even after all the air has apparently left the lungs, the chest muscles and the abdominal muscles should be contracted hard to expel as much air as possible from the lungs.3 KEGEL'S EXERCISES: The pelvic muscles are contracted hard in the way of holding in urine or a bowel motion. The contraction is held for some time and then relaxed. This exercise should be repeated as often as possible throughout the day. It tones the pelvic muscles, preventing uterine prolapse and stress incontinence later on.3 EXERCISES FOR THE ABDOMINAL MUSCLES: Lie on your back with legs flexed at the hip and knee joint. Breathing out slowly, the abdominal muscles are drawn in as much as possible. At the same time, the back should be flattened, allowing the small of the back to touch the floor. The muscles are then released slowly in time with drawing in the breath. This exercise tones the abdominal muscles.3 EXERCISES FOR THE BACK MUSCLES: In the standing up position, the arms are raised overhead while drawing in the breath. Slowly breathing out, the body is bent forwards and the toes are touched with the fingers. This exercise helps to tone up the back muscles and the sacroiliac joint.3 6.1 NEED FOR THE STUDY:
3 The postpartum period, or puerperium, starts about an hour after the delivery of the placenta and includes the following six weeks. Postpartum care should respond to the special needs of the mother and baby during this special phase and should include: the prevention and early detection and treatment of complications and disease, and the provision of advice and services on breastfeeding, birth spacing, immunization and maternal nutrition.1 Postpartum haemorrhage is the single most important cause of maternal death. It kills 150 000 women each year and nearly nine out of ten of these deaths take place within four hours of delivery. A woman who is anaemic is usually less able to cope with blood loss than a woman who is well nourished. During the first hours after the birth, the care-giver has to make sure that the uterus remains well contracted and that there is no heavy loss of blood. If the bleeding is particularly severe blood transfusion may be the only way of saving a woman’s life.1 Puerperal infections such as sepsis are still major causes of maternal mortality in many developing countries. Fever is the main symptom and antibiotics the main treatment, though prevention by ensuring cleanliness and hygiene at delivery is obviously the best course of action.2 Eclampsia is the third most important cause of maternal mortality worldwide. A woman suffering from eclampsia or severe preeclampsia the first days postpartum should be hospitalized. Other common postpartum complications include urinary tract problems such as infections, urine retention or incontinence. Many women also experience pain in the perineum and vulva for several weeks, especially if there was tissue damage or an episiotomy during the second stage of labour. The woman’s perineum should be regularly inspected to make sure it is not infected.4 The three main vitamin or mineral nutritional deficiencies in the postpartum period are iodine deficiency disorders, vitamin A deficiency and iron deficiency anaemia. The main causes of micronutrient malnutrition are inadequate intake of foods providing these micronutrients and their impaired absorption or utilization. Preventive and treatment measures include ensuring regular intake of appropriate foods, food fortification, giving supplements to pregnant and lactating women and infants and children.4 The number of health problems reported in the first months after delivery is high. In India 23% indicated problems, and in Bangladesh nearly 50% reported symptoms 6 weeks after delivery, while in England 47% of the women reported at
4 least one symptom. Some symptoms are more typically present in the immediate postpartum period and usually resolve quickly, while others, once they occur, often become chronic. The most frequently reported postpartum physical problems are:
Country Lower Abdominal Pain High fever Foul discharge
India 4.4% 5.3% 0.5%
Egypt 21.9% 15.5% 9.8%
Bangladesh 19.0% 16.5% 10.2%
Indonesia 15.2% 13.4% 4.5%
Apart from that the problems are stress incontienece, backache, headache, bladder problem, fistula, haemorrhoids and constipation.4 Psychological problems in the postpartum period are also not uncommon. These problems can be lessened by adequate social support and support from trained care-givers during pregnancy, labour and postpartum period. The nutritional status of the woman during adolescence, pregnancy and lactation has a direct impact on maternal and infant health in the puerperium. Women’s intake postpartum should be increased to cover the energy cost of lactation.5 A study conducted to investigate risk factors for poor self-rated health (SRH) in primiparous and multiparous women 2 months and 1 year after childbirth in a national wide Swedish sample. Women were recruited at their first booking visit at 593 (97%) antenatal clinics in Sweden during 3 weeks evenly spread over 1 year (1999-2000). The representatively of the sample was assessed by comparison with the total Swedish birth cohort of 1999.The Result shows that Physical problems, such as tiredness, musculoskeletal symptoms, and abdominal pain, and emotional problems, such as depressive symptoms, increased the risk of poor SRH in both primiparas and multiparas at one or both time points. Ongoing physical and emotional problems, lack of support, and infant factors seem more important than socio-demographic background. Mode of delivery and childbirth experience may have a long term effect on SRH.6
5 From the above review and the investigator own experience the postnatal mother knowledge about the diet and exercise needed to minimize the pelvic floor problem following the delivery is needed .So the investigator selected this topic to assess the knowledge and attitude of the mother regarding the postnatal diet and exercise in indention to develop the information. 6.2 REVIEW OF LITERATURE: The review of literature will discussed based on the following headings 1. Studies related to the physical health complaints of the postnatal mothers. 2. Studies related to the Knowledge of postnatal diet and exercise among the general mothers. 1. Studies related to the physical health complaints of the postnatal mother. The postal survey was distributed to all women who gave birth in a two-week period in Victoria, Australia .The response rate to the postal survey was 62.5% (n = 1,336). Physical and related health problems associated with significantly increased odds of depression at six to seven months were: tiredness (OR 3.42 [2.2-5.3]); urinary incontinence (OR 2.23 [1.5-3.4]); back pain (OR 2.20 [1.6-3.0]); sexual problems (OR 2.16 [1.6-3.0]); more coughs, colds and minor illnesses than usual (OR 2.78 [1.9- 4.1]); bowel problems (OR 1.93 [1.3-2.9]) and relationship difficulties (OR 3.88 [2.8- 5.4]). At follow up, three physical health factors were associated with statistically significant linear trends with poorer levels of emotional wellbeing. These were: tiredness (chi2 for linear trend = 12.38, P < 0.001); urinary incontinence (chi 2 for linear trend = 5.63, P = 0.02); and more minor illnesses than usual (chi 2 for linear trend = 7.94, P = 0.005). This study confirms a link between maternal emotional wellbeing and physical health and recovery in the postnatal period and has important implications for clinical practice. Strategies for encouraging greater disclosure of physical and emotional health problems, assessment of the physical health of recent mothers presenting with depression, and emotional health of recent mothers presenting with other morbidity should be high priorities for all health professionals in contact with mothers in the year following childbirth.7 Postpartum mothers experience certain physical health conditions that may affect their quality of life, future health, and health of their children. Twenty-two articles were reviewed from searches in scientific databases, reference lists, and an up-to-date survey. In general, postpartum mothers self-rate their health as good. They experience certain physical conditions such as fatigue/physical exhaustion, sleep-
6 related problems, pain, sex-related concerns, hemorrhoids/constipation, and breast problems. Despite a limited number of studies, the findings provide a glimpse of the presence of a number of physical health conditions experienced by women in the 2 years postpartum. In the articles reviewed, physical health conditions and postpartum period were poorly defined, no standard scales existed, and the administration of surveys varied widely in time. Those disparities prevented systematic comparisons of results and made it difficult to gain a coherent understanding of the physical health conditions of postpartum mothers. More longitudinal research is needed that focuses on the etiology, predictors, and management of the health conditions is most prevalent among postpartum mothers. Instruments are needed that target a broader range of physical conditions in respect to type and severity.8 This study examines that personal and work-related factors associated with the postpartum health of employed women 11 weeks after childbirth. Using a prospective cohort design, recruited 817 Minnesota mothers into the study while they were hospitalized for childbirth in 2001. Telephone interviews were conducted at 5 and 11 weeks postpartum. Eligible women were 18 years or older, employed, and spoke English and gave birth to a singleton infant. This results show that 11 weeks postpartum, 661 participants (81% of enrollees) completed a full interview, and 50% of participants had returned to work. On average, women reported 4.1 (SD 3.2) childbirth-related symptoms, most frequently fatigue (43%). Factors significantly associated with better health outcomes included better preconception health, the absence of prenatal mood problems, more control over work and home activities, more social support at work and home, and less job stress. This finding suggested that postpartum women need to be evaluated regarding their fatigue levels and mental and physical symptoms. Women whose fatigue or postpartum symptoms limit daily role function may find it helpful to have health care clinicians counsel them on strategies to decrease job stress, increase social support at work and home, and certify their use of intermittent family and medical leave to help them manage their symptoms.9 The Cohort study were to describe the prevalence of a number of physical symptoms, as described by women themselves, two months and one year after childbirth in a national Swedish sample and to investigate the association between specific symptoms and women's self-rated health. A total of 2413 women recruited from 593 antenatal clinics in Sweden during one-week periods evenly spread over one year (1999-2000), representing 54% of women eligible for the study and 76% of those
7 who consented to participate. The result shows that Tiredness, headache, neck, shoulder and low back pain were common problems at two months as well as one year after childbirth. At two months, pain from caesarean section, dyspareunia and haemorrhoids were frequent problems, whereas stress incontinence was often reported at one year. Ninety-one percent of the women said self-rated health was 'very good' or 'good' at two months after birth, and 86% at one year. Low self-rated health was associated with symptoms that affected general physical functioning and wellbeing, such as tiredness, headache, musculoskeletal problems, mastitis, perineal pain, dysuria, stomachache and nausea. Complaints related to more specific situations, such as dyspareunia, constipation and stress incontinence were not associated with self- rated health.10 2. Studies related to the Knowledge of postnatal diet and exercise among the mothers. A prospective case-control study of infants from birth to one year was conducted in a lower middle-class urban setting in Amman, Jordan. The study objective was to examine the relationship between maternal anaemia and iron- deficiency anaemia during infancy. A sample of 107 anaemic (Hb < 11 g/dl) and 125 non-anaemic mothers was selected at 37 weeks' gestation and matched for age and parity, and infant data at birth obtained. The main outcome measure was the incidence of iron-deficiency anaemia in the two groups of infants, defined in the study as Hb < 11 g/dl and either plasma ferritin < 12 mcg/l or zinc protoporphyrin > 35 mcg/dl. The result shows that Iron endowment in cord blood samples appeared similar between the two groups. The incidence of iron-deficiency anaemia was very high in these infants, at 72% by research criteria, (51% if Hb < 10.5 g/dl), but significantly higher in the infants born to anaemic mothers at all stages of the year, with overall incidence of 81% (n = 91), compared to 65% in controls (n = 112). Anaemic mothers had not recovered adequate iron status at 6 months' postpartum, with implications for future pregnancy and lactation iron demands. The study concluded that the anaemia during pregnancy compromises the health of mothers in traditional cultures, where women tend to have several children close together after marriage, with an inadequate interval to replenish nutritional stores. Their infants also appear to be at increased risk of developing iron-deficiency anaemia, undetected at birth.11 A longitudinal study establish the report practice of pelvic floor exercises and stress urinary incontinence after delivery in 257 women in the North-East of Scotland.
8 One hundred and sixty-three women responded (63.4%). This finding shows that more women reported the practice of pelvic floor exercises after delivery than during pregnancy: 134 (83.2%) compared with 123 (76.4%). Six to 12 months after delivery, 96 (60%) women said that they were still doing the exercises. A third of respondents (n=54, 33.1%) reported stress incontinence at some time since having the baby. Of those reporting incontinence at the time of questionnaire completion, six (19.3%) said the incontinence was moderate or severe, whereas eight (34.7%) reported incontinence once a week or more. The practice of pelvic floor exercises daily or more often during pregnancy was associated with less reported postnatal incontinence compared with less frequent practice. Self-reported rates of practice of pelvic floor exercises increased from pregnancy to the immediate postnatal period and subsequently declined. A third of women reported the symptoms of stress incontinence after delivery. Daily or more frequent practice of the exercises during pregnancy may be required in order to prevent postnatal incontinence (although further research is required to confirm this finding). Midwives should continue to encourage regular and frequent practice of pelvic floor exercises in the postnatal period and beyond. They also need to ask about symptoms of stress incontinence and refer as necessary.12 The evidence-based effectiveness of peripartum pelvic floor exercises (PFEs) in the prevention of pelvic floor problems including urinary and anal incontinence, and prolapse. A comprehensive literature search was performed to find all studies that involved the use of antepartum and postpartum PFEs. For the MEDLINE (1966 to 2002) and CINAHL (1980 to 2002) searches, the following key words were used: urinary incontinence (prevention and control, rehabilitation, therapy), fecal incontinence, exercise or exercise therapy, Kegel, muscle contraction, muscle tonus, muscle development, pelvic floor, pregnancy, puerperium, puerperal disorders. Twelve studies evaluating the role of antepartum PFE were found, of which 3 randomized controlled trials (RCTs) comparing PFEs for the prevention of urinary incontinence to controls were included. Twelve studies evaluating postpartum PFEs for prevention of urinary incontinence were reviewed, of which 4 RCTs were included. Five studies evaluating postpartum PFEs for the prevention of anal incontinence were reviewed, of which 4 RCTs were included. The result shows that Postpartum PFEs, when performed with a vaginal device providing resistance or
9 feedback, appear to decrease postpartum urinary incontinence and to increase strength.13 A prospective matched controlled trial conducted to evaluate the long term effect of a postpartum pelvic floor muscle training course in prevention and treatment of urinary incontinence. Eight-week pelvic floor muscle training program in prevention and treatment of urinary incontinence in the immediate postpartum period were contacted by telephone one year after delivery. They were invited to participate in a follow up study. The study group consisted of 81 matched pairs (n = 162), with a mean age (range) 28 years (19-40), and mean number (range) of deliveries 1.8 (1-5). Seventy-six pairs had normal vaginal deliveries and five elective caesarean sections. Clinical assessment of pelvic floor muscle function and strength were by vaginal palpation and vaginal squeeze pressure. The result shows that at the one year follow up, significantly more women in the former control group than in the training group reported stress urinary incontinence and/or showed urinary leakage at the pad test (P < 0.01). A significantly greater (P < 0.01) muscle strength increase in the period between 16th week and one year postpartum was demonstrated in the former training group (mean 4.4 cm H2O, 95% CI 3.2-5.6) than in the control group (mean 1.7 cm H2O, 95% CI 0.8-2.7). This one year follow up study demonstrates that a specially designed postpartum pelvic floor muscle training course was effective in the prevention and treatment of stress urinary incontinence. The benefits from pelvic floor muscle training are still present one year after delivery.14 6.3 STATEMENT OF THE PROBLEM: A study to assess the knowledge and attitude regarding the postnatal diet and exercise among mothers in selected hospitals, Bangalore with a view to develop the information booklet. 6.4 OBJECTIVES: 1. To assess the level of knowledge and attitude regarding the postnatal diet and exercise among the selected mothers. 2. To correlate the level of knowledge with attitude regarding the postnatal diet and exercise between mothers and mothers. 3. To associate the level of knowledge and attitude regarding the postnatal diet and exercise with selected socio demographic variable. 4. To develop the information booklet based on the findings. 6.5 OPERATIONAL DEFINITIONS:
10 Assess: To measure the level of knowledge and attitude regarding the postnatal diet and exercise. Compare: To assess the similarity between the level of knowledge and attitude regarding the postnatal diet and exercise. Knowledge: It is acquiring the information regarding the postnatal diet and exercise measured in terms of numerically. Attitude: It is an opinion, idea regarding the postnatal diet and exercise measured in terms of numerically. Postnatal: The period which follows soon after the delivery to six weeks. Postnatal diet: The planned balanced food which meets the adequate nutritional requirement of the postnatal mothers. Postnatal exercise: The set of physical activity which specially planned for the postnatal mothers to promote the health and fitness. Mothers: The women in the reproductive age group those who are attending the antenatal and postnatal clinic in the selected hospital, Bangalore. 6.6 ASSUMPTION: 1. Information promotes the self decision to meet the postnatal needs of the Mothers. 2. Knowledge can promote the healthy life style. 3. Awareness prevents the malnutrition. 6.7 HYPOTHESES:
H1: There will be significant increases in the knowledge and attitude regarding the postnatal diet and exercise among the mothers. 6.8 INCLUSION AND EXCLUSION CRITERIA: INCLUSION CRITERIA: 1. Samples are mothers in the selected hospital in Bangalore. 2. Those that can able to understand and read either Kannada or English. 3. Both antenatal and postnatal mothers included in the study. 4. Both primi and multi Mothers included in the study. EXCLUSION CRITERIA: 1. Those who are absent during the period of study. 2. Those who are non cooperative. 6.9 DELIMITATION: 1. The sample size is limited to 100 mothers.
11 2. Prescribed data collection is only 8 weeks. 7. MATERIALS AND METHODS OF STUDY: 7.1 SOURCE OF DATA: The mothers those who are attending to the selected hospital in Bangalore. 7.2 METHOD OF DATA COLLECTION: a. RESEACH DESIGN: A descriptive non experimental design. b. SETTING: The study will be conducted to the selected hospital in Bangalore. c. POPULATION: The mothers those who are attending antenatal and postnatal clinic in the selected hospital in Bangalore. d. SAMPLING TECHNIQUE: Non Probability – convenient sampling. e. SAMPLE SIZE: Sample comprises of 100 mothers. f. TOOLS: Using close-ended questioners. g. METHOD OF DATA ANALYSIS AND PRESENTATION: The data will be analyzing by using descriptive and inferential statistics. h. DURATION OF THE STUDY: 6-8 weeks 6 weeks data collection. 2 weeks follow up. i. PROJECTED OUTCOME: By the end of the study the mother will help to find out the knowledge and attitude of mothers in hospital regarding diet and exercise. 7.3 ETHICAL CONSIDERATION: 1. Does the study require any intervention to be provided to the subjects? Yes. 2. Has ethical clearances being obtained from institution? Yes.
8. LIST OF REFERENCE:
12 1. K. Park. Preventive and social Medicine. Banarsidas publishers 19th edition.367-369. 2. ICMR recommended dietary Intakes for Indians, New Delhi. Report 1990. 3. Shruthi Home › Frequently Asked Questions › Health Information › how important is post natal care? Is it common to feel more and more tired as the baby grows older? s\ Sun, 10/12/2008 - 21:35. 4. Dr. Soledad Diaz. Postpartum Care of the Mother and Newborn: WHO/RHT/MSM/98.3,2006. 5. Enkin M, Keirse MJNC, Renfrew M, Neilson J. A guide to effective care in pregnancy and childbirth. 2 nd edition. Oxford University Press, 1995. 6. Schytt E, and Waldenström U. Risk factors for poor self-rated health in women at 2 months and 1 year after childbirth. Journal of Womens Health. 2007 Apr;16(3):390-405. 7. Brown S, Lumley J. Physical health problems after childbirth and maternal depression at six to seven months postpartum. British Journal of Obstretics and Gynecology. 2000 Oct;107(10):1194-201. 8. Cheng CY and Li Q. Integrative review of research on general health status and prevalence of common physical health conditions of women after childbirth. Womens Health Issues. 2008 Jul-Aug;18(4):267-80. 9. McGovern P and Dowd B. Mothers' health and work-related factors at 11 weeks postpartum. Ann Fam Med. 2007 Nov-Dec;5(6):519-27. 10. Schytt E, Lindmark G et.al. Physical symptoms after childbirth: prevalence and associations with self-rated health. British Journal of Obstretics and Gynecology. 2005 Feb;112(2):210-7. 11. J .Kilbride and TG Baker, Anaemia during pregnancy as a risk factor for iron- deficiency anaemia in infancy: a case-control study in Jordan. International Journal of Epidemiology, Vol 28, 461-468 2006 online in Wiley interscience.com. 12. Whitford HM and Alder B.A longitudinal follow up of women in their practice of perinatal pelvic floor exercises and stress urinary incontinence in North-East Scotland. Midwifery. 2007 Sep;23(3):298-308. 13. Harvey MA.Pelvic floor exercises during and after pregnancy: a systematic review of their role in preventing pelvic floor dysfunction. J Obstet Gynaecol Can. 2003 Jun;25(6):451-3.
13 14. Morkved S, Bo K. Effect of postpartum pelvic flooruscle training in prevention and treatment of urinary incontinence: a one-year follow up. BJOG. 2000 Aug;107(8):1022-8.
9. SIGNATURE OF STUDENT :
14 10. REMARKS OF THE GUIDE : The research topic selected is relevant as it attempts to empower the mothers’ knowledge and attitude regarding the diet and exercises.
11. NAME AND DESIGNATION OF :
11.1 GUIDE NAME : MRS.INDIRA. V
ADDRESS : PROFESSOR, OBSTETRICS AND GYNAECOLOGICAL NURSING, NAVANEETHAM COLLEGE OF NURSING, BANGALORE-43.
11.2 SIGNATURE OF GUIDE :
11.3 HEAD OF DEPARTMENT :
NAME : MRS. INDIRA.V
ADDRESS : H.O.D. OBSTETRICS AND GYNAECOLOGICAL NURSING NAVANEETHAM COLLEGE OF NURSING, BANGALORE-43.
11.4 SIGNATURE OF H.O.D. :
12. REMARKS OF PRINCIPAL : MRS. MALARVIZHI
15 PRINCIPAL, NAVANEETHAM COLLEGE OF NURSING, BANGALORE-43 The related topic is relevant as it attempts to explore the mothers’ knowledge and attitude regarding diet and exercises.
12.1 SIGNATURE OF PRINCIPAL :
16