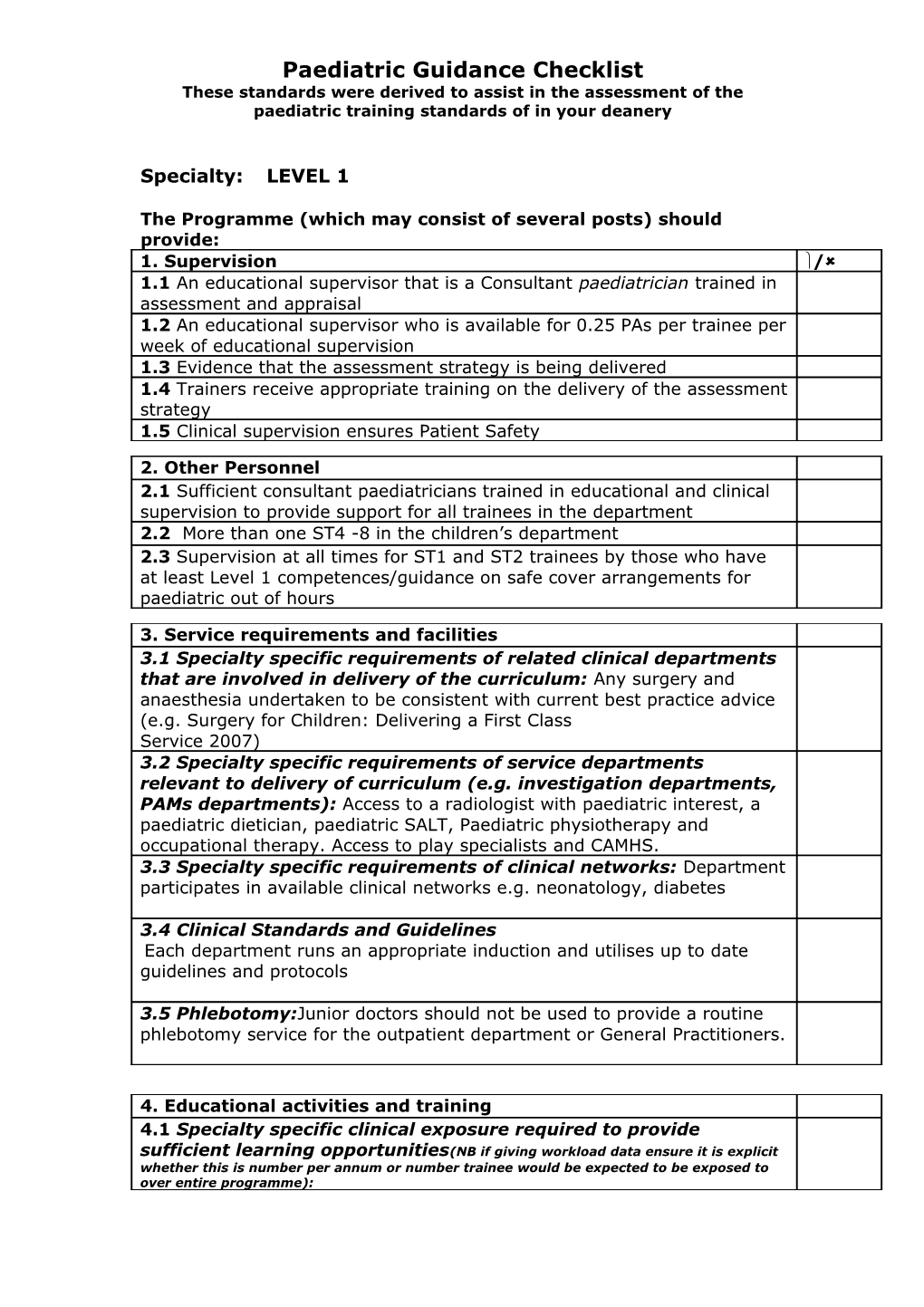
Paediatric Guidance Checklist These standards were derived to assist in the assessment of the paediatric training standards of in your deanery
Specialty: LEVEL 1
The Programme (which may consist of several posts) should provide: 1. Supervision / 1.1 An educational supervisor that is a Consultant paediatrician trained in assessment and appraisal 1.2 An educational supervisor who is available for 0.25 PAs per trainee per week of educational supervision 1.3 Evidence that the assessment strategy is being delivered 1.4 Trainers receive appropriate training on the delivery of the assessment strategy 1.5 Clinical supervision ensures Patient Safety
2. Other Personnel 2.1 Sufficient consultant paediatricians trained in educational and clinical supervision to provide support for all trainees in the department 2.2 More than one ST4 -8 in the children’s department 2.3 Supervision at all times for ST1 and ST2 trainees by those who have at least Level 1 competences/guidance on safe cover arrangements for paediatric out of hours
3. Service requirements and facilities 3.1 Specialty specific requirements of related clinical departments that are involved in delivery of the curriculum: Any surgery and anaesthesia undertaken to be consistent with current best practice advice (e.g. Surgery for Children: Delivering a First Class Service 2007) 3.2 Specialty specific requirements of service departments relevant to delivery of curriculum (e.g. investigation departments, PAMs departments): Access to a radiologist with paediatric interest, a paediatric dietician, paediatric SALT, Paediatric physiotherapy and occupational therapy. Access to play specialists and CAMHS. 3.3 Specialty specific requirements of clinical networks: Department participates in available clinical networks e.g. neonatology, diabetes
3.4 Clinical Standards and Guidelines Each department runs an appropriate induction and utilises up to date guidelines and protocols
3.5 Phlebotomy:Junior doctors should not be used to provide a routine phlebotomy service for the outpatient department or General Practitioners.
4. Educational activities and training 4.1 Specialty specific clinical exposure required to provide sufficient learning opportunities(NB if giving workload data ensure it is explicit whether this is number per annum or number trainee would be expected to be exposed to over entire programme): Paediatric Guidance Checklist These standards were derived to assist in the assessment of the paediatric training standards of in your deanery
Level 1 programme consisting of a series of posts which allow adequate opportunity to cover the range of level 1 competences
St1-2 should be predominantly acute general paediatrics with 6 months of neonatal intensive care and some training in sub-specialty paediatrics
Appropriate clinical activity Assessment of 400 acute new presentations per trainee per year of training
During 6 months neonatal intensive care training opportunity to be present at 30 deliveries requiring attendance and to admit 20 infants to NICU/SCBU 4.2 Specialty specific requirements for structured training opportunities to include courses: Training in child protection awareness to include formal education and training courses which cover the Level 1 (ST1-3) safeguarding competences Relevant resuscitation training for example APLS/EPLS and NLS Structured programme of formal teaching and learning opportunities to complement work-place based training and ensure curriculum coverage 4.3 Specialty specific requirements for other experiential learning(excluding clinics and ward rounds): Level 1 training should include awareness of child health provision outside the hospital setting e.g. schools, community based clinics, primary care, and opportunities to experience and to witness multidisciplinary team working where possible
4.4 Administration of IV Antibiotics: Trainees should be fully trained in the preparation and administration of IV antibiotics as this may be necessary in an emergency situation. E.g. a child with meningococcal sepsis. 4.5 Newborn Examinations: Junior doctors should not be routinely expected to perform examinations of well newborn infants during evening and night shifts, unless this is clinically indicated.
5. Working patterns 5.1 Safe cover arrangements for paediatric department out of hours in line with RCPCH guidance 5.2 Evidence of compliance with existing employment rules to working time 5.3 Working intensity and pattern that is appropriate for learning 5.4 Acute general paediatric experience including the out of hours commitment will provide essential training for this level of training 5.6 Working patterns which allow trainees to regularly attend at least 60% of regional training days 5.7 inappropriate attendance to the Delivery Suite Clear local guidance should be in place to indicate which deliveries Paediatric staff should attend, minimising presence where there is no proven need. Guidance should be reviewed on a yearly basis. Paediatric Guidance Checklist These standards were derived to assist in the assessment of the paediatric training standards of in your deanery
6. Specific Post requirements 6.1 ST1 - 3 neonatal training must be provided in units that undertake Level 2 and 3 neonatal intensive care 6.2 General training based in acute settings must include emergency duties, inpatients and outpatients
7. Enabled to learn new skills, necessary skills and curriculum coverage (specialty specific) This section can be used to highlight marker conditions to which trainee should be exposed or the numbers of cases/procedures that trainee will be expected to see/do. Ensure that it is clear whether any numbers are for whole training programme or per annum 7.1 Specialty specific marker conditions trainee should be exposed to: Problems; Fever, fits, breathing difficulty, diarrhoea, vomiting, developmental delay, rashes, hypoxia, chronic disease, child abuse and neglect, prematurity, jaundice, faltering growth, behavioural problems, common post natal problems, post natal screening, resuscitation and stabilisation of a sick child
Diagnoses; diabetes, epilepsy, asthma, cerebral palsy, respiratory distress syndrome, congenital heart disease, nephrotic syndrome, arthritis, anaemia, head injury, ingestion, infectious diseases, gastroenteritis, childhood cancer, cystic fibrosis 7.2 Specialty specific skills/procedures trainee needs to complete: Bag, valve mask ventilation, blood sampling (capillary and venous) lumbar puncture, intravenous lines, tracheal intubation, umbilical vein catheterisation, prescribing, interosseous needle insertion
8. Access to clinics and ward rounds and long term care of patients 8.1 Specialty specific numbers and types of clinics expected to attend (including outreach clinics): 10 clinics per 6 months 5 clinics when in neonatal post 8.2 Specialty specific ward rounds consultant led and independent per week: Regular attendance at daily consultant led ward rounds
9. Meetings 9.1 Specialty specific number and types of MDT/multi- professional meetings expected to be exposed to: 1 MDT meeting per 6 months at level 1 (e.g. Discharge planning, complex care, safeguarding)
10. Clinical audit 10.1 Evidence of trainees participation in clinical governance (at least 1 full audit/year, preferably completing an audit cycle and attendance at critical incident meetings) 10.2 Evidence of trainees participation in clinical guideline development Paediatric Guidance Checklist These standards were derived to assist in the assessment of the paediatric training standards of in your deanery
11. Teaching appraising and assessing 11.1 Opportunities to deliver formal and informal teaching (e.g. to medical students or peers) and receive feedback 11.2 Opportunities for involvement in and contributing to the assessment of others (e.g. giving feedback) 11.3 Opportunity to receive training in work-place based assessment
12. Research 12.1 Provide opportunity to acquire level 1 competences in research 12.2 Provide opportunities to be involved in clinical research
13. Management 13.1 Opportunities to be involved in management e.g. participation in management meetings and projects 13.2 Opportunities for communication with colleagues e.g. Handover and discharge letter writing 13.3 Administrative duties including preparation of notes, finding equipment, filing of results within patient notes and locating and retrieving patient medical records following admission should not routinely be the responsibility of junior doctors. Trainees should assist with these tasks when appropriate but sufficient clerical support should exist within the department.
AND MUST BE WILLING TO HOST THE MRCPCH CLINICAL EXAM
X- Comments ref