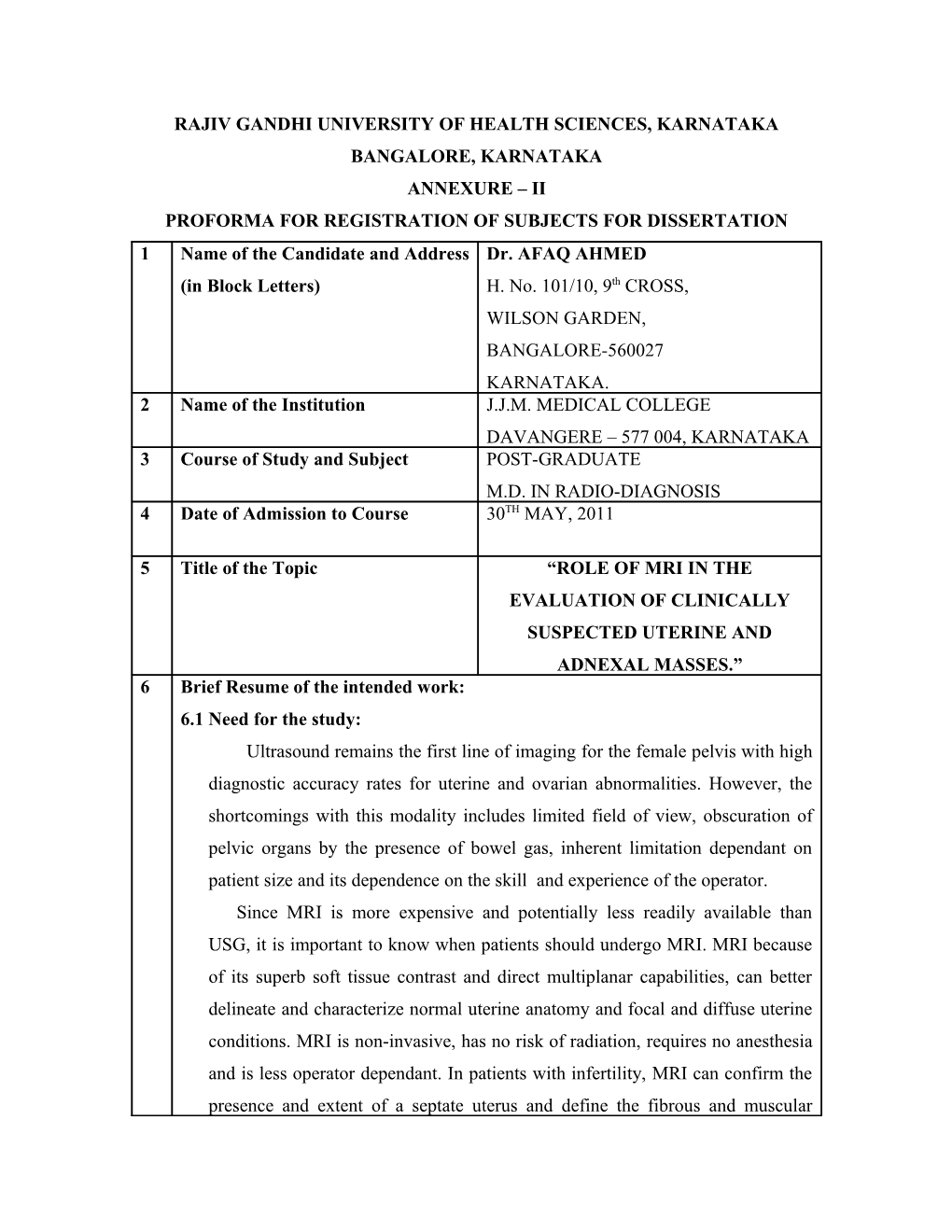
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES, KARNATAKA BANGALORE, KARNATAKA ANNEXURE – II PROFORMA FOR REGISTRATION OF SUBJECTS FOR DISSERTATION 1 Name of the Candidate and Address Dr. AFAQ AHMED (in Block Letters) H. No. 101/10, 9th CROSS, WILSON GARDEN, BANGALORE-560027 KARNATAKA. 2 Name of the Institution J.J.M. MEDICAL COLLEGE DAVANGERE – 577 004, KARNATAKA 3 Course of Study and Subject POST-GRADUATE M.D. IN RADIO-DIAGNOSIS 4 Date of Admission to Course 30TH MAY, 2011
5 Title of the Topic “ROLE OF MRI IN THE EVALUATION OF CLINICALLY SUSPECTED UTERINE AND ADNEXAL MASSES.” 6 Brief Resume of the intended work: 6.1 Need for the study: Ultrasound remains the first line of imaging for the female pelvis with high diagnostic accuracy rates for uterine and ovarian abnormalities. However, the shortcomings with this modality includes limited field of view, obscuration of pelvic organs by the presence of bowel gas, inherent limitation dependant on patient size and its dependence on the skill and experience of the operator. Since MRI is more expensive and potentially less readily available than USG, it is important to know when patients should undergo MRI. MRI because of its superb soft tissue contrast and direct multiplanar capabilities, can better delineate and characterize normal uterine anatomy and focal and diffuse uterine conditions. MRI is non-invasive, has no risk of radiation, requires no anesthesia and is less operator dependant. In patients with infertility, MRI can confirm the presence and extent of a septate uterus and define the fibrous and muscular components. In patients with pelvic pain, MRI is more sensitive and specific than USG for the findings of Adenomyosis. MRI should be considered for the evaluation of uterine and adnexal pathology when sonographic characteristics are not definitive to determine the origin of the mass and to determine the likelihood of malignancy. Sonographically indeterminate adnexal masses of uncertain origin and solid or cystic content benefit from further evaluation with MRI, which is highly accurate for identifying the origin of a mass and characterizing its tissue content. Thus, use of MRI will prove to be cost-effective in that it reduces unnecessary surgical procedures by its ability to differentiate benign and malignant lesions accurately. MRI can assist sonographic assessment of adnexal masses in pregnancy by depicting the characteristic findings of red degeneration of leiomyoma, endometrioma, decidualized endometrioma and massive ovarian edema. Accordingly, MRI should be considered as a useful adjunct when sonography is inconclusive or insufficient to guide management of adnexal masses discovered in pregnancy. Thus, MRI can be very useful in characterization and origin of uterine and adnexal masses, staging of known endometrial and cervical cancers, evaluation of suspected mullerian ductal anomalies, differentiating benign from malignant lesions where other imaging modalities (like ultrasonography and CT scan) are not conclusive.
6.2 Review of Literature With its high contrast resolution, its ability to provide good tissue characterization, and its multiplanar imaging capabilities, magnetic resonance imaging (MRI) is increasingly used to evaluate pelvic pathology. There is a significant difference, however, in the inherent costs of MRI and ultrasound. The dilemma for referring physicians and general radiologists is to decide when it is appropriate to refer patients for MRI. Leiomyomas Transvaginal ultrasound has been shown to be as efficient as MRI in the detection of the presence of myomas; however, MRI is superior in terms of mapping individual myomas [1] . This is especially true with larger uteri and with the presence of a large number of myomas. On MRI, a uterus containing leiomyomas will be enlarged and will have an abnormal contour. On T2W images, leiomyomas appear as sharply marginated lesions of low signal intensity relative to the myometrium. Often, a high-signal- intensity rim can be identified, more commonly in intramural or subserosal leiomyomas. Leiomyomas may contain calcifications, especially in older women. Calcified myomas can cause significant artifact on ultrasound and can obscure adjacent tissues. While similar calcification appears as a signal void on MRI, it typically does not limit the evaluation of adjacent tissues. On MRI, myomas larger than 3 to 5 cm are often heterogeneous because of various degrees of degeneration. Although varied, enhancement tends to be heterogeneous and less than that of the myometrium.
Adenomyosis Although adenomyosis is typically a diffuse process, focal areas of involvement are also seen. It is these focal lesions that are often mistaken for leiomyomas. It is important to differentiate between them, as their treatments vary greatly. Studies have shown that MRI is superior to ultrasound for the diagnosis of adenomyosis [2] . The characteristic appearance of adenomyosis on MRI is diffuse thickening (>12 mm) of the junctional zone. This is most evident on
T2W sequences and corresponds to the smooth muscle hyperplasia associated with the ectopic tissue. A junctional zone ≤ 8 mm virtually excludes the disease, whereas a width of 9 to 11 mm is equivocal. Other findings that may suggest the diagnosis include poorly defined margins of the junctional zone and foci of high signal intensity on T1W or T2W sequences that indicate the presence of endometrial cysts. The foci of high signal may represent ectopic endometrium, cystically dilated endometrial glands, or hemorrhage. Contrast administration has been shown to be of very little benefit in the diagnosis of adenomyosis. Distinguishing between focal adenomyosis and leiomyomas is reliably achieved with MRI, and we now know that these conditions often coexist[3]. Unlike leiomyomas, a focal area of adenomyosis will have indistinct margins and extend subjacent to the myometrium. The signal characteristics will otherwise be the same as with the diffuse form of the disease. Treatment implications for focal adenomyosis and leiomyoma differ however, so accurate diagnosis is important.
Uterine endometrial pathology: Endometrial thickening seen at ultrasound is a nonspecific finding. For years, endometrial biopsy was the diagnostic standard for differentiating benign causes, such as polyps and leiomyomas, from endometrial carcinoma. However, benign abnormalities far outnumber cancer in these situations. Other problems with biopsy include vaginal or cervical stenosis and difficulty in obtaining an adequate specimen. MRI can be helpful in further differentiating these lesions.
Endometrial carcinoma: MRI is not recommended as a screening procedure in the diagnosis of endometrial carcinoma. However, MRI has proven to be an important tool for the staging of known endometrial carcinoma [4] . MRI can differentiate between superficial and deep-muscle-invasive tumors by using a combination of T2W imaging and contrast-enhanced MRI. This can significantly alter surgical management. The presence of cervical invasion also alters preoperative and surgical management. MRI has been shown to be superior to both CT and ultrasound in assessing myometrial invasion, cervical extension, and nodal involvement. Endometrial carcinomas appear isointense to the myometrium and endometrium on T1W images. On T2W images, their signal intensity is commonly hyperintense; however, this is quite variable [4] . Endometrial carcinomas usually enhance less than the myometrium does, with the difference less marked on delayed images. Myometrial invasion is best visualized on T2W images, where it appears as a disruption or an irregularity of the junctional zone by a mass of intermediate signal intensity. Transmyometrial extension of tumor is identified by interruption of the normal low signal intensity of the serosal surface. However, early serosal invasion may be difficult to detect. Parametrial involvement is best depicted on
T1W images with a signal intensity change in the parametrial fat. T1-weighted images are also better for identifying tumor involvement of the vagina when there is disruption of the low signal intensity wall. Lymph node involvement is suggested on T1W images with nodes that have a diameter >1 cm in the short axis. MRI can also detect tumor extension outside the true pelvis as well as bladder and rectal invasion.
Cervical carcinoma: Like the uterus, the cervix has a zonal anatomy that is well delineated on
T2W images. MRI is not initially used to diagnose cervical cancer but is used to stage disease in women who have had a diagnosis established by a Pap smear or biopsy. T2-weighted images obtained in the sagittal plane and in a plane along the short axis of the cervix are the most useful for local staging. On T2W images, cervical cancer appears as a mass of higher signal intensity than the adjacent fibrous cervical stroma, but the mass is of lower signal intensity than the endometrium [5] . If the low signal intensity of the inner cervical stroma is preserved, stage IIB or higher disease is excluded, which indicates that the patient is likely a surgical candidate. Macroscopic extension of tumor into the parametrial fat establishes a diagnosis of stage IIB disease. MRI has an accuracy range of 75% to 95% in detecting parametrial invasion. MRI can accurately assess for more advanced disease such as pelvic sidewall invasion and obstruction of the distal ureter [5] . Localizing the tumor and determining the presence or absence of ureteral obstruction can provide a road map for radiation therapy. Mullerian duct anomalies: The incidence of müllerian duct anomalies is approximately 0.1% to 3%. Although they are often asymptomatic, obstetrical complications occur in up to 25% of these women, including spontaneous abortion, stillbirth, preterm delivery, and adverse obstetrical outcomes. Knowledge of the type and severity of the anomaly can significantly impact treatment, as the therapies vary greatly. With an accuracy approaching 100%, MRI has become the gold standard in identifying müllerian duct anomalies [6,7] . Various studies have shown that it is superior to sonography and hysterosalpingography [6] . In patients with primary amenorrhea, MRI can determine the presence or absence of the vagina, cervix, and uterus [7] . Bicornuate and septate uteri are the 2 most common types of mullerian ductal anomalies. Differentiating between these 2 entities is important because of their complications and different treatments. The evaluation of the external fundal contour is the key to differentiating between bicornuate and septate uteri. This can be best evaluated on a plane that passes through the long axis of the uterus. The outer contour of the septated uterus is convex or fat, with <10-mm concavity. The outer fundal contour of a bicornuate uterus or uterus didelphys should have >10-mm concavity between the right and left uterine horns.
Sonographically indeterminate adnexal masses: A perception in radiology is that MRI may be superfluous for a mass that is large (>5 cm), suspicious, or inconclusive for ovarian cancer on sonography[8,9,]. However, Outwater and Dunton[9] revealed that unnecessary surgery was performed in 50–67% of benign cases because of suspicious sonography findings. Study done by Adusumilli et al., revealed 90 final benign diagnoses, 13 of which were actually normal MRI findings despite a sonographically questioned mass. The value of reassuring a patient that a sonographically detected ovarian mass is not a malignancy but a normal structure or a benign mass cannot be underestimated; patients avoid not only surgery but also unnecessary followup imaging and anxiety. These issues justify the need to recognize which sonographic features routinely result in an indeterminate or suspicious diagnosis and to determine whether MRI is the appropriate next step. Surprisingly, only 11 indeterminate diagnoses were the result of technically limited sonograms; rather, a specific imaging feature of a mass more commonly yielded an indeterminate diagnosis. The study reveals that sonography performs poorly for determining the origin of the mass, which is the essential first step in characterizing an adnexal mass. For example, although a solid intrauterine mass is likely a fibroid, a solid mass located adjacent to the uterus may be a pedunculated uterine fibroid or an ovarian mass. In this study (Adusumilli et al.,) 48% of such masses were pedunculated fibroids and 34% were ovarian masses. Large mass size was an additional contributing factor to an indeterminate sonographic diagnosis in five cases. Unless specific features of fibroids can be identified, such as refractory shadowing, these large solid pelvic masses remain diagnostic dilemmas on sonography[10,11]. Unlike sonography, excellent agreement was seen between MRI and the final proven origin of a mass. This stresses the importance of MRI as the best next step in evaluating such a mass before subjecting a patient to surgery that might be unnecessary. The results of the study in accurately characterizing an adnexal mass as a pedunculated uterine fibroid (17/18 masses) are similar to those reported in prior MR studies[12,13]. Because fibrous tumors of the ovary have imaging features similar to those of fibroids, such as low signal intensity on T2-weighted images, the recognition of the stalk of the fibroid and the identification of separate normal ovaries can help confirm the diagnosis of a fibroid. In postmenopausal women, identification of atrophic ovaries can be problematic and the uterus may be small, which limits visualization of a stalk[13, 14]. In such cases, the identification of vessels bridging the mass and the uterus on T2-weighted and gadolinium- enhanced images (“bridging vascular” sign) has an accuracy of 80% for the diagnosis of pedunculated uterine fibroids[14]. This study (Adusumilli et al.,) also documented that eight indeterminate “masses” on sonography were not masses but a cervical remnant, mullerian anomaly, or low-lying bowel filled with feces. MRI is well suited to the characterization of uterine and cervical tissue and the evaluation of congenital uterine anomalies [15,7]. Extraovarian cystic masses can pose a diagnostic challenge on sonography and MRI. The advantage of MRI is its ability to reveal separate normal ovaries and to delineate the characteristic morphologic features of a mass on multiple imaging planes, such as the pathognomonic tortuous folded appearance of a hydrosalphinx[9]. The study (Adusumilli et al.,) showed that accurate tissue characterization, the second essential component of characterizing an adnexal mass, was poor for sonography and excellent for MRI. The entire spectrum of benign and malignant pelvic masses appeared solid on sonography in this study, and benign masses sometimes appeared complex on sonography, thereby mimicking a malignancy.
Unenhanced T1- and T2-weighted imaging is important for accurate tissue characterization. Lipid and blood are readily detected on T1-weighted imaging
[9,16, 17,18]. with and without fat suppression T2-weighted imaging helps to identify the relatively low signal intensity of endometriomas, reflecting blood degradation products from repeated cyclical bleeding[9] or the very low signal intensity of fibrous tissue in a fibrous tumor of the ovary (i.e., Brenner tumor, ovarian fibroma, fibrothecoma)[19,20,16]. Gadolinium is usually reserved for improved delineation of papillary projections, nodules, and thick enhancing septations in ovarian cancers[8,21,22]. Although in this study (Adusumilli et al.,) they correctly classified eight purely cystic unilocular ovarian masses as benign or probably benign, they could not distinguish between a functional ovarian cyst and a serous cystadenoma to prevent surgery in seven patients. Although MRI is sensitive for the detection of the fluid content of a mass[12, 9, 23], it may not add information beyond what is gleaned from a good-quality sonogram for a unilocular, purely cystic ovarian mass. Moreover, the size of a simple unilocular cyst has little correlation with the likelihood of malignancy[9]. Therefore, the more appropriate and cost- effective way of managing such a mass in a premenopausal woman is to perform follow-up sonography for interval resolution. The high specificity (94%) for establishing a benign diagnosis in this study (Adusumilli et al.,) is similar to that reported by Scoutt et al.[12] (fibroids, 100%; dermoids, 99%; endometriomas, 91%). The specificity of this study is slightly higher than reported by Hricak et al.[8], which may be explained by their larger number of cystic ovarian masses (53/91 lesions), which are difficult to characterize as benign because of lack of tissue specificity. The study done by Adusumilli et al., also had mullerian anomalies and a larger number of uterine fibroids (17 V/s 3), which are more readily diagnosed as benign, than did Hricak et al. The radiologist’s subjective impression of malignancy versus benignity was highly accurate in this study, which supports prior conclusions that subjective assessment is one of the best discriminators in making such a diagnosis[24]. The false diagnoses of ovarian cancer occurred with cystic ovarian masses because of large mass size (> 4 cm) and lack of tissue specificity and with a solid adnexal mass that was a broad-ligament fibroid having intermediate signal intensity on T2-weighted images and avid enhancement, two features suggestive of malignancy. Pathologic adnexal mass is found in 1–2% of pregnancies. Sonography is the primary method of detection and evaluation, but findings may be nonspecific and then MRI may assist characterization[25]. The use of MRI in pregnancy has expanded because of improvements in rapid breath-hold sequences and because better imaging helps avoid the potential hazards of surgery during gestation. Gadolinium is teratogenic in animal studies and crosses the placenta where it is presumably excreted by the fetal kidneys into the amniotic fluid. In the era of nephrogenic systemic fibrosis, this characteristic of gadolinium raises theoretic concerns of toxicity related to disassociation and persistence of free gadolinium. Gadolinium is classified as a category C drug by the U.S. Food and Drug Administration (FDA) and can be used if considered critical—that is, to be administered only “if the potential benefit justifies the potential risk to the fetus.” More stable macrocyclic agents (e.g., gadoteridol or gadobutrol) may be preferable to gadolinium. In reality, contrast administration for adnexal masses is used primarily to assess for the presence of solid components in a cystic mass and is used to a lesser extent to evaluate nonenhancement in a torsed mass. Such information can generally be derived from gray-scale and Doppler sonography; thus, it is unlikely that IV gadolinium would be considered critical for MRI of an adnexal mass in pregnancy.
6.3 Objectives of the Study: Characterization of uterine and adnexal masses as benign or malignant. To determine the origin, tissue content and characterization of sonographically indeterminate uterine and adnexal masses. Staging of cancer when a mass is noted to have malignant changes. To assist the surgeons in deciding on further line of management.
7. MATERIALS AND METHOD 7.1Sources of Data The main source of data for the study are patients from the following teaching hospitals attached to Bapuji Education Association, J.J.M. Medical College, Davangere . 1. Bapuji Hospital. 2. Chigateri General Hospital. 3. S.S. Institute of Medical Sciences and Research centre.
Technique: Imaging will be done with 1.5 tesla Philips Achieva machine using abdominal surface coils. The following sequences will be selected as required.
a) T1WI, T2WI AND STIR (in axial plane).
b) T2WI and STIR (in coronal plane).
c) T2WI and STIR (in sagittal plane). Contrast will be used as and when required. Gadolinium will be used as intravenous contrast material in a dose of 0.1 mmol/kg body weight.
Post contrast study includes T1W FAT SUPPRESSED Sequence (in axial, coronal and sagittal planes).
7.2 Method of collection of Data (including sampling procedures if any) All patients referred to the department of Radio diagnosis, J.J.M Medical college, Davangere with clinically suspected uterine and adnexal masses in a period of 2 years from Nov 2011 to November 2013 will be subjected for the study. The study will be conducted on a minimum of 30 cases focussing mainly on sonographically indeterminate uterine and adnexal masses. However, the scope of increasing the number of cases exists depending upon the availability within the study period.
Duration of study: 2 years.
Data Analysis: By proportional scale.
Inclusion criteria: All patients with clinically suspected uterine and adnexal masses with indeterminate diagnosis on sonography. For staging of known malignant conditions. Patients of all age groups.
Exclusion criteria: Mimicks of adnexal masses such as exophytic uterine leiomyoma and ectopic pregnancy. All Patients having cardiac pacemakers, prosthetic heart valves, cochlear implants or any metallic implants. Patients having history of claustrophobia. All patients who do not consent to be a part of the study. 7.3 Does the Study require any investigations or interventions to be conducted on patients or other humans or animals? If so please describe briefly. YES The study is mainly based on investigations as Radiology itself is a tool of investigation. Interventions would be done as and when it is indicated alone. The study involves only humans. Informed consent would be taken after explaining about and before any procedure.
7.4 Has ethical clearance been obtained from your institution in case of 7.3? YES Ethical clearance has been obtained from the Research and Dissertation Committee/ Ethical Committee of the institution for this study.
8. LIST OF REFERENCES 1. Dueholm M, Lundorf E, Hansen ES. Accuracy of magnetic resonance imaging and transvaginal ultrasonography in the diagnosis, mapping, and measurement of uterine myomas. Am J Obstet Gynecol 2002; 186: 409-415. 2. Ascher SM, Arnold LL, Patt RH. Adenomyosis: Prospective comparison of MR imaging and transvaginal sonography. Radiology. 1994; 190: 803-806. 3. Togashi K, Ozasa H, Konishi I. Enlarged uterus: Differentiation between adenomyosis and leiomyoma with MR imaging. Radiology. 1989; 171: 531- 534. 4. Yamashita Y, Mizutani H, Torashima M. Assessment of myometrial invasion by endometrial carcinoma: Transvaginal sonography V/s contrast- enhanced MR imaging. AJR Am J Roentgenol. 1993; 161: 595-599.
5. Hricak H, Finck S, Honda G, Göranson H. MR imaging in the evaluation of benign uterine masses: Value of gadopentetate dimeglumine-enhanced T1- weighted images. AJR Am J Roentgenol 1992; 158: 1043-1050. 6. Pellerito JS, McCarthy SM, Doyle MB. Diagnosis of uterine anomalies: Relative accuracy of MR imaging, endovaginal sonography, and hysterosalpingography. Radiology 1992;183:795-800. 7. Carrington BM, Hricak H, Nuruddin RN. Mullerian duct anomalies: MR imaging evaluation. Radiology 1990; 176: 715-720. 8. Hricak H, Chen M, Coakley FV. Complex adnexal masses: detection and characterization with MR imaging multivariate analysis. Radiology 2000; 214: 39–46 9. Outwater EK, Dunton CJ. Imaging of the ovary and adnexa: clinical issues and applications of MR imaging. Radiology 1995; 194:1–18 10. Baltarowich OH, Kurtz AB, Pennell RG, Needleman L, Vilaro MM, Goldberg BB. Pitfalls in the sonographic diagnosis of uterine fibroids. AJR 1988; 151: 725–728 11. Caoili EM, Hertzberg BS, Kliewer MA, DeLong D, Bowie JD. Refractory shadowing from pelvic masses on sonography: a useful diagnostic sign for uterine leiomyomas. AJR 2000; 174: 97–101 12. Scoutt LM, McCarthy SM, Lange R, Bourque A, Schwartz PE. MR evaluation of clinically suspected adnexal masses. J Comput Assist Tomogr 1994; 18: 609–618 13. Weinreb JC, Barkoff ND, Megibow A, Demopoulos R. The value of MR imaging in distinguishing leiomyomas from other solid pelvic masses when sonography is indeterminate. AJR 1990; 154: 295–299 14. Kim JC, Kim SS, Park JY. Bridging vascular sign in the MR diagnosis of exophytic uterine leiomyoma. J Comput Assist Tomogr 2000; 24: 57–60. 15. Imaoka I, Wada A, Matsuo M, Yoshida M, KitagakiH, Sugimura K. MR imaging of disorders associated with female infertility: use in diagnosis, treatment, and management. Radio Graphics 2003; 23: 1401–1421.
16. Siegelman ES, Outwater EK. Tissue characterization in the female pelvis by means of MR imaging. Radiology 1999; 212: 5–18. 17. Kier R, Smith RC, McCarthy SM. Value of lipid and water-suppression MR images in distinguishing between blood and lipid within ovarian masses. AJR 1992; 158: 321–325. 18. Stevens SK, Hricak H, Campos Z. Teratomas versus cystic hemorrhagic adnexal lesions: differentiation with proton-selective fat-saturation MR imaging. Radiology 1993; 186: 481–488. 19. Outwater EK, Siegelman ES, Talerman A, Dunton C. Ovarian fibromas and cystadenofibromas: MRIfeatures of the fibrous component. J Magn Reson Imaging 1997; 7:465–471 20. Outwater EK, Siegelman ES, Kim B, Chiowanich P, Blasbalg R, Kilger A. Ovarian Brenner tumors: MR imaging characteristics. Magn Reson Imaging 1998; 16:1147–1153. 21. Outwater EK, Huang AB, Dunton CJ, Talerman A, Capuzzi DM. Papillary projections in ovarian neoplasms: appearance on MRI. J Magn Reson Imaging 1997; 7: 689–695. 22. Van Vierzen PB, Massuger LF, Ruys SH, Barentsz JO. Borderline ovarian malignancy: ultrasound and fast dynamic MR findings. Eur J Radiol 1998; 28: 136–142. 23. Jain KA, Jeffrey RB Jr. Evaluation of pelvic masses with magnetic resonance imaging and ultrasonography. J Ultrasound Med 1994; 13: 845–853. 24. Sohaib SA, Sahdev A, Van Trappen P, Jacobs IJ, Reznek RH. Characterization of adnexal mass lesions on MR imaging. AJR 2003; 180: 1297–1304. 25. Bromley B, Benacerraf B. Adnexal masses during pregnancy: accuracy of sonographic diagnosis and outcome. J Ultrasound Med 1997; 16: 447–452. 9. Signature of the Candidate
Study will conclude near possible diagnosis with near possible accuracy 10. Remarks of the Guide leading to better surgical management and welfare of the patients. 11. Name & Designation 11.1 Guide Dr. KIRAN KUMAR HEGDE S. M.D. PROFESSOR, DEPARTMENT OF RADIO- DIAGNOSIS, J.J.M. MEDICAL COLLEGE, DAVANGERE – 577 004.
11.2 Signature
11.3 Co-Guide (If any)
11.4 Signature
11.5 Head of the Department Dr. J .PRAMOD SETTY M.D., PROFESSOR AND HEAD, DEPARTMENT OF RADIO- DIAGNOSIS, J.J.M. MEDICAL COLLEGE, DAVANGERE – 577 004.
11.6 Signature
12 12.1 Remarks of the Chairman & the Principal
12.2 Signature