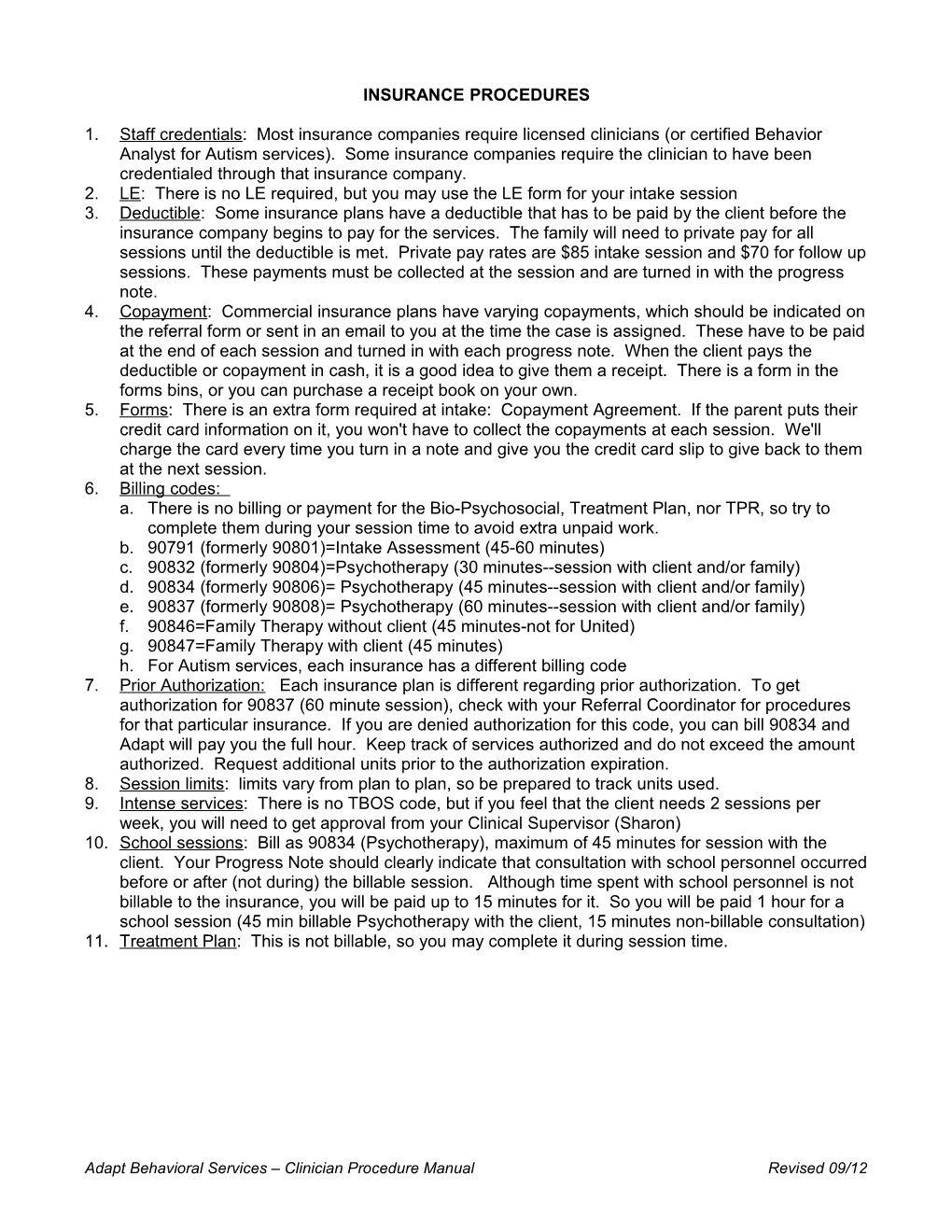
INSURANCE PROCEDURES
1. Staff credentials: Most insurance companies require licensed clinicians (or certified Behavior Analyst for Autism services). Some insurance companies require the clinician to have been credentialed through that insurance company. 2. LE: There is no LE required, but you may use the LE form for your intake session 3. Deductible: Some insurance plans have a deductible that has to be paid by the client before the insurance company begins to pay for the services. The family will need to private pay for all sessions until the deductible is met. Private pay rates are $85 intake session and $70 for follow up sessions. These payments must be collected at the session and are turned in with the progress note. 4. Copayment: Commercial insurance plans have varying copayments, which should be indicated on the referral form or sent in an email to you at the time the case is assigned. These have to be paid at the end of each session and turned in with each progress note. When the client pays the deductible or copayment in cash, it is a good idea to give them a receipt. There is a form in the forms bins, or you can purchase a receipt book on your own. 5. Forms: There is an extra form required at intake: Copayment Agreement. If the parent puts their credit card information on it, you won't have to collect the copayments at each session. We'll charge the card every time you turn in a note and give you the credit card slip to give back to them at the next session. 6. Billing codes: a. There is no billing or payment for the Bio-Psychosocial, Treatment Plan, nor TPR, so try to complete them during your session time to avoid extra unpaid work. b. 90791 (formerly 90801)=Intake Assessment (45-60 minutes) c. 90832 (formerly 90804)=Psychotherapy (30 minutes--session with client and/or family) d. 90834 (formerly 90806)= Psychotherapy (45 minutes--session with client and/or family) e. 90837 (formerly 90808)= Psychotherapy (60 minutes--session with client and/or family) f. 90846=Family Therapy without client (45 minutes-not for United) g. 90847=Family Therapy with client (45 minutes) h. For Autism services, each insurance has a different billing code 7. Prior Authorization: Each insurance plan is different regarding prior authorization. To get authorization for 90837 (60 minute session), check with your Referral Coordinator for procedures for that particular insurance. If you are denied authorization for this code, you can bill 90834 and Adapt will pay you the full hour. Keep track of services authorized and do not exceed the amount authorized. Request additional units prior to the authorization expiration. 8. Session limits: limits vary from plan to plan, so be prepared to track units used. 9. Intense services: There is no TBOS code, but if you feel that the client needs 2 sessions per week, you will need to get approval from your Clinical Supervisor (Sharon) 10. School sessions: Bill as 90834 (Psychotherapy), maximum of 45 minutes for session with the client. Your Progress Note should clearly indicate that consultation with school personnel occurred before or after (not during) the billable session. Although time spent with school personnel is not billable to the insurance, you will be paid up to 15 minutes for it. So you will be paid 1 hour for a school session (45 min billable Psychotherapy with the client, 15 minutes non-billable consultation) 11. Treatment Plan: This is not billable, so you may complete it during session time.
Adapt Behavioral Services – Clinician Procedure Manual Revised 09/12