Pharmacotherapy of Community Acquired Pneumonia (CAP) Elizabeth Nolte, PharmD Candidate 2007
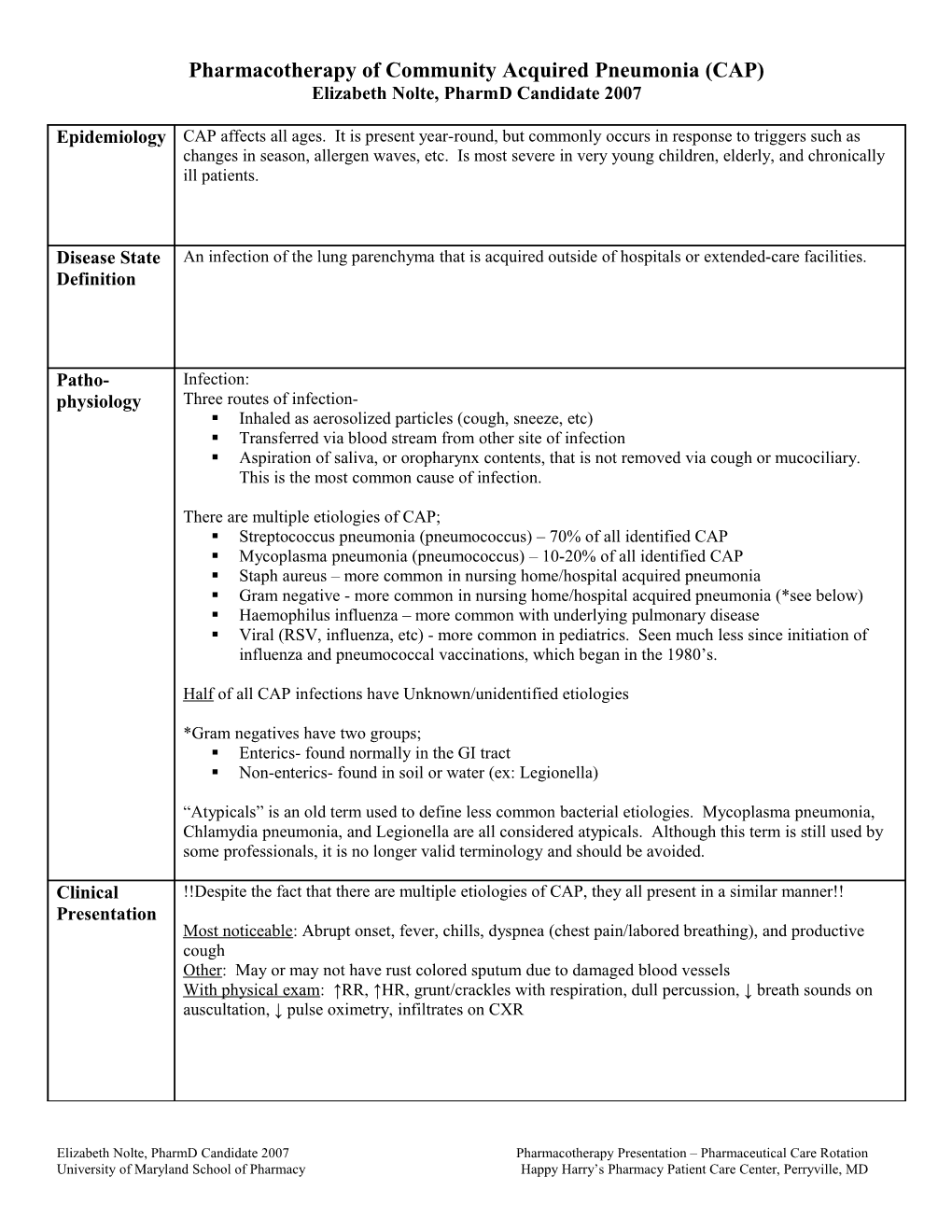
Epidemiology CAP affects all ages. It is present year-round, but commonly occurs in response to triggers such as changes in season, allergen waves, etc. Is most severe in very young children, elderly, and chronically ill patients.
Disease State An infection of the lung parenchyma that is acquired outside of hospitals or extended-care facilities. Definition
Patho- Infection: physiology Three routes of infection- . Inhaled as aerosolized particles (cough, sneeze, etc) . Transferred via blood stream from other site of infection . Aspiration of saliva, or oropharynx contents, that is not removed via cough or mucociliary. This is the most common cause of infection.
There are multiple etiologies of CAP; . Streptococcus pneumonia (pneumococcus) – 70% of all identified CAP . Mycoplasma pneumonia (pneumococcus) – 10-20% of all identified CAP . Staph aureus – more common in nursing home/hospital acquired pneumonia . Gram negative - more common in nursing home/hospital acquired pneumonia (*see below) . Haemophilus influenza – more common with underlying pulmonary disease . Viral (RSV, influenza, etc) - more common in pediatrics. Seen much less since initiation of influenza and pneumococcal vaccinations, which began in the 1980’s.
Half of all CAP infections have Unknown/unidentified etiologies
*Gram negatives have two groups; . Enterics- found normally in the GI tract . Non-enterics- found in soil or water (ex: Legionella)
“Atypicals” is an old term used to define less common bacterial etiologies. Mycoplasma pneumonia, Chlamydia pneumonia, and Legionella are all considered atypicals. Although this term is still used by some professionals, it is no longer valid terminology and should be avoided.
Clinical !!Despite the fact that there are multiple etiologies of CAP, they all present in a similar manner!! Presentation Most noticeable: Abrupt onset, fever, chills, dyspnea (chest pain/labored breathing), and productive cough Other: May or may not have rust colored sputum due to damaged blood vessels With physical exam: ↑RR, ↑HR, grunt/crackles with respiration, dull percussion, ↓ breath sounds on auscultation, ↓ pulse oximetry, infiltrates on CXR
Elizabeth Nolte, PharmD Candidate 2007 Pharmacotherapy Presentation – Pharmaceutical Care Rotation University of Maryland School of Pharmacy Happy Harry’s Pharmacy Patient Care Center, Perryville, MD Risk Factors The alveoli are normally sterile. When normal defense mechanisms are overwhelmed, and secretions/bacteria are allowed into the lower respiratory tract, infection occurs.
Aspiration is seen often while sleeping, especially in patients who; . Abuse alcohol or narcotics, . Have an underlying neurological disorder, such as Parkinson’s disease, . Have pulmonary disease (obstructive or chronic bacterial infections), asthma, or a history of smoking.
Other risk factors = exposure to infected persons, sepsis, diabetes mellitus, immune compromised, age (<2 or >50), or serious organ damage (particularly the heart and liver).
History of pulmonary viral infections can also trigger a secondary bacterial pneumonia infection. This is a common cause in pediatric patients.
Diagnosis Confirm infection; 1. Chest radiograph 2. Sputum exam & Gram stain w/ or w/o culture 3. Physical exam, ROS, and risk factors 4. Other tests- limited to no benefit (WBC, blood culture, pulse oximetry, etc)
Desired Once CAP is confirmed, assessment is needed- Therapeutic . Determine etiology Outcomes* . Determine severity (to hospitalize or not; oral therapy versus iv) Ask- Is the patient over 50 years old? Does the patient have neoplastic disease, congestive heart failure, cerebrovascular disease, liver failure, or renal failure? Does the patient show altered mental status, pulse >125 beats/min, RR > 30/min, systolic BP < 90 mmHg, or temperature <35° or >40° C? Assess laboratory values. . If there is a reason why patient developed CAP, determine if that also needs therapy.
*Reference of To maintain body temperature between 97-100° F. Guidelines Used To eradicate bacterial cause of CAP (if possible. With chronic pulmonary infections or COPD- To reduce bacterial growth and return patient to normal levels) To prevent complications from CAP symptoms (keep patient hydrated, provide nutrition, provide respiratory support if needed) To prevent complications of pharmacological therapy regimen To prevent CAP recurrence if risk factors suggest that patient is prone to respiratory infections To initiate pharmacologic therapy within 8 hours if admitted into a hospital
*IDSA Guidelines for Community Acquired Pneumonia. Available from http://www.journals.uchicago.edu/IDSA/guide/AP63_811.K.pdf [cited 2006 June 30]. **Dipiro JT, Talbert RL, Yee GC, et.al. Pharmacotherapy: A Pathophysiology Approach. 5th ed. New York: McGraw-Hill; 2002.
Elizabeth Nolte, PharmD Candidate 2007 Pharmacotherapy Presentation – Pharmaceutical Care Rotation University of Maryland School of Pharmacy Happy Harry’s Pharmacy Patient Care Center, Perryville, MD Treatment Pharmacological; Options** Tylenol- fever reduction Albuterol via MDI or nebulizer – increase ease of breathing (Non-drug and Antibiotics- must consider geographical area and patient related variables (resistance!), as well as Drug Therapy ability of antibiotic to penetrate alveoli and mucous. – include all . Doxycyclin therapeutic . Macrolides classes/agents . Combination Penicillins available and . 2nd/3rd Generation Cephalosporins preferences . Fluoroquinolones per treatment . Various other antibiotics guidelines) Non-pharmacological; Humidified oxygen – if hypoxic Hydrate Nutritional support Pneumococcal vaccination – if prone to recurrent CAP infections
**See Treatment **per CDC- Avoid use of fluoroquinolones as first line therapy in order to preserve efficacy and Options Table prevent development of resistance. Try using other efficacious options first. Monitoring Subjective Efficacy: Patient to self monitor daily- (Efficacy and Wheezing Toxicity Difficulty breathing Parameters) Pain with breathing Chills Cough
Objective Efficacy: Health professional monitor hourly if hospitalized or at follow-up visit if treated out-patient: Temperature RR HR Health professional monitor daily if hospitalized: Urinary output CBC (leukocytes, WBC) Health professional monitor monthly if chronic pulmonary complications exist: CXR
Toxicity: ** Refer to Pharmacological Treatment Options for CAP Handout
Elizabeth Nolte, PharmD Candidate 2007 Pharmacotherapy Presentation – Pharmaceutical Care Rotation University of Maryland School of Pharmacy Happy Harry’s Pharmacy Patient Care Center, Perryville, MD SEVERITY ASSESSMENT FOR COMMUNITY ACQUIRED PNEUMONIA
Risk-Class Mortality Rates for Patients With Pneumonia Validation Cohort Risk Class No. of Points No. of Patients Mortality (%) Recommended Site of Care I No predictors 3034 0.1 Outpatient II ≤70 5778 0.6 Outpatient III 71-90 6790 2.8 Outpatient or brief inpatient IV 91-130 13,104 8.2 Inpatient V >130 9333 29.2 Inpatient
Elizabeth Nolte, PharmD Candidate 2007 Pharmacotherapy Presentation – Pharmaceutical Care Rotation University of Maryland School of Pharmacy Happy Harry’s Pharmacy Patient Care Center, Perryville, MD