Literature Update for CERGA January – April 2010
Contents
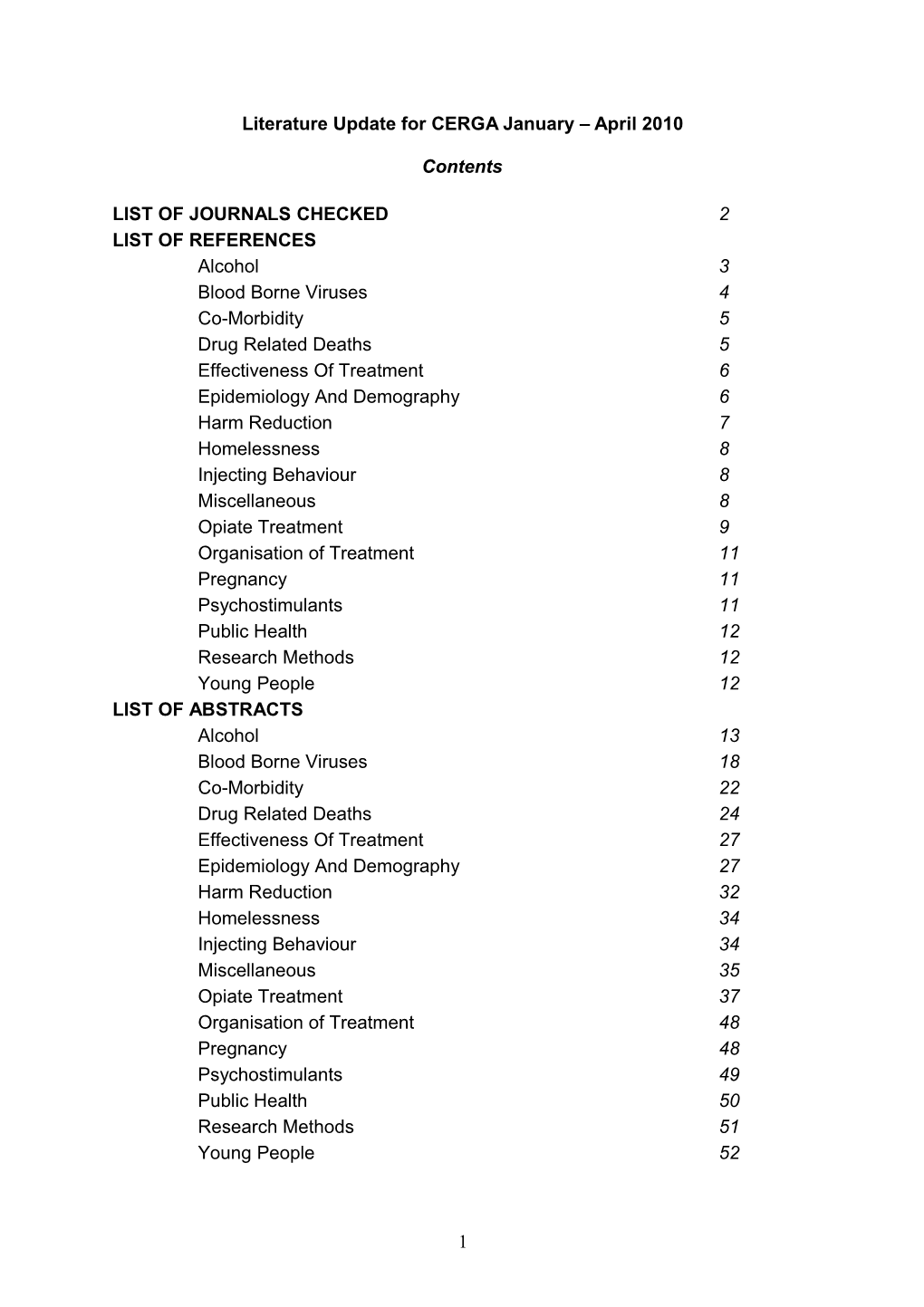
LIST OF JOURNALS CHECKED 2 LIST OF REFERENCES Alcohol 3 Blood Borne Viruses 4 Co-Morbidity 5 Drug Related Deaths 5 Effectiveness Of Treatment 6 Epidemiology And Demography 6 Harm Reduction 7 Homelessness 8 Injecting Behaviour 8 Miscellaneous 8 Opiate Treatment 9 Organisation of Treatment 11 Pregnancy 11 Psychostimulants 11 Public Health 12 Research Methods 12 Young People 12 LIST OF ABSTRACTS Alcohol 13 Blood Borne Viruses 18 Co-Morbidity 22 Drug Related Deaths 24 Effectiveness Of Treatment 27 Epidemiology And Demography 27 Harm Reduction 32 Homelessness 34 Injecting Behaviour 34 Miscellaneous 35 Opiate Treatment 37 Organisation of Treatment 48 Pregnancy 48 Psychostimulants 49 Public Health 50 Research Methods 51 Young People 52
1 Number of issues per year Journal Title Volumes and Issues Checked Addiction Volume 105, issues (1) January, (2) February, (3) March, (4) April. 6
Addictive Behaviours Volume 35, issues (1) January, (2) February, (3) March, (4) April. 12
Addictive Disorders Volume 9 (1) March. 4 Alcohol and Alcoholism Volume 45 issues (1) January/February, (2) March. 6
Alcoholism Clinical & Volume 34 issues (1) January Experimental Research (2) February, (3) March. 12
Drug and Alcohol Dependence Volume 106, (1) January Volume 107, (2)/(3) March 21 Volume 108, (1)/(2) April.
Drug and Alcohol Review Volume 29, issues (1) January, (2) March. 6
Drugs: Education, Prevention Volume 17, issues 1 and 2. & Policy 2
Forensic Science International Volume 194, (1) January, Volume 196, (3) March. 30
International Journal of Drug Volume 21, issues (1) January, Policy (2) March. 6
Journal of Addictive Diseases Volume 29, (1). 4
Journal of Substance Abuse Volume 38, issues (1) January, Treatment (2) March, 8 Volume 39, (3) April.
The American Journal of Drug Volume 36, (1) January. and Alcohol Abuse 6
2 List of References
Alcohol
1. Alcohol Intake and Systemic Markers of Inflammation—Shape of the Association According to Sex and Body Mass Index Alcohol Alcohol 2010 45: 119-125 Andreia Oliveira, Fernando Rodríguez-Artalejo and Carla Lopes
2. Analysis of the Factors Determining Survival of Alcoholic Withdrawal Syndrome Patients in a General Hospital Alcohol & Alcoholism 2010 45(2): 151–158 R. Monte, R. Rabuñal, E. Casariego, H. López-Agreda, A. Mateos and S. Pértega
3. Methodological Assessment of Economic Evaluations of Alcohol Treatment: What Is Missing? Alcohol Alcohol 2010 45: 53-63 Carolina Barbosa, Christine Godfrey and Steve Parrott
4. Planned and Unplanned Discharge from Alcohol Services in Scotland, 2004–2008 Alcohol Alcohol 2010 45: 64-69 Rosemary Newham, Christopher Russell and John B. Davies
5. Ecological Associations of Alcohol Outlets With Underage and Young Adult Injuries Alcoholism: Clinical Experimental Research 2010 34 (3): 519-527 Paul J. Gruenewald, Bridget Freisthler, Lillian Remer, Elizabeth A. LaScala, Andrew J. Treno and William R. Ponicki
6. Effect of motivational interviewing on reduction of alcohol use Drug and Alcohol Dependence 2010 107 (1): 23-30 Adeline Nyamathi , Steven Shoptaw, Allan Cohen, Barbara Greengold, Kamala Nyamathi, Mary Marfisee, Viviane de Castro, Farinaz Khalilifard, Daniel George and Barbara Leake
7. Moderators and mediators of two brief interventions for alcohol in the emergency department Addiction 2010 105 (3): 452-465 Nancy P. Barnett, Timothy R. Apodaca, Molly Magill, Suzanne M. Colby, Chad Gwaltney, Damaris J. Rohsenow and Peter M. Monti
8. Predictors of hangover during a week of heavy drinking on holiday Addiction 2010 105 (3): 476-483 Morten Hesse and Sébastien Tutenges
9. The dimensionality of alcohol use disorders and alcohol consumption in a cross-national perspective
3 Addiction 2010 105 (2): 240-254 Guilherme Borges, Yu Ye, Jason Bond, Cheryl J. Cherpitel, Mariana Cremonte, Jacek Moskalewicz, Grazyna Swiatkiewicz and Maritza Rubio- Stipec
10. Efficacy of repetitive transcranial magnetic stimulation in alcohol dependence: a sham-controlled studyadd_ Addiction 2010 105 (1): 59-557 455 Biswa R. Mishra, S. Haque Nizamie, Basudeb Das & Samir K. Praharaj
11. Age-Related Gray Matter Shrinkage in a Treatment Naïve Actively Drinking Alcohol-Dependent Sample Alcoholism: Clinical and Experimental Research 2010 34 (1): 175-182 George Fein, Ryan Shimotsu, Jerome Barakos
Blood Borne Viruses
12. Hepatitis B virus among injecting drug users in Sydney, Australia: Prevalence, vaccination and knowledge of status Drug and Alcohol Independence 2010 108 (1-2): 134-137 Carolyn A. Day, Bethany White, Gregory J. Dore, Ingrid van Beek, Craig Rodgers, Philip Cunningham, Alex Wodak and Lisa Maher
13. Needle sharing in regular sexual relationships: An examination of serodiscordance, drug using practices, and the gendered character of injecting Drug and Alcohol Dependence 2010 107: 182–187 Joanne Bryant, Loren Brener, Peter Hull, Carla Treloar
14. Antibody response to hepatitis B vaccine in substance use disorder patients Drug and Alcohol Dependence 2010 107 (1): 39-43 Hildi J. Hagedorn, Nancy A. Rettmann, Eric W. Dieperink, Janet Durfee and Bashar Aqel
15. The Relationship between Performance on the Shipley Institute of Living Scale (SILS) and Hepatitis C Infection among Active Injection Drug Users in Baltimore, Maryland The American Journal of Drug and Alcohol Abuse 2010 36: 61–65 Stevan Geoffrey Severtson, Mary M. Mitchell, Alicia Hubert, William Latimer and John Hopkins
16. Can hepatitis C virus prevalence be used as a measure of injection- related human immunodeficiency virus risk in populations of injecting drug users? An ecological analysis Addiction 2010 105 (2): 311-318 Peter Vickerman, Matthew Hickman, Margaret May, Mirjam Kretzschmar and Lucas Wiessing
4 17. The outcome of a rapid hepatitis B vaccination programme in a methadone treatment clinic Addiction 2010 105 (2): 329-334 Parameswaran Ramasamy, Nicholas Lintzeris, Yvonne Sutton, Helen Taylor, Carolyn A. Day and Paul S. Haber
18. Combined effects of alcohol and hepatitis C: A secondary analysis of alcohol use biomarkers and high-risk behaviors from two medication trials for alcohol dependence Addictive Behaviours 2010 35 (2): 123-128 Jennifer G. Plebani, Carlos F. Tirado, Helen M. Pettinati, Kyle M. Kampman, Joseph R. Volpicelli, David W. Oslin
Co-Morbidity
19. Relationship between anxiety disorders and opiate dependence— A systematic review of the literature: Implications for diagnosis and treatment Journal of Substance Abuse Treatment 2010 38 (3): 220-230 Melina Fatséas, Cécile Denis, Estelle Lavie and Marc Auriacombe
20. Randomized controlled trial of cognitive–behavioural therapy for coexisting depression and alcohol problems: short-term outcome_ Addiction 2010 105(1): 87-997 9 Amanda L. Baker, David J. Kavanagh, Frances J. Kay-Lambkin, Sally A. Hunt, Terry J. Lewin, Vaughan J. Carr & Jennifer Connolly
21. Childhood trauma and health outcomes in adults with comorbid substance abuse and mental health disorders Addictive Behaviours 2010 35 (1): 68-71 Nancy S. Wu, Laura C. Schairer, Elinam Dellor and Christine Grella
22. The association between violence and lifetime suicidal thoughts and behaviors in individuals treated for substance use disorders Addictive Behaviours 2010 35 (2): 111-115 Mark A. Ilgen, Mandi L. Burnette, Kenneth R. Conner, Ewa Czyz, Regan Murray and Stephen Chermack
Drug related deaths
23. Interpretation of hair findings in children after methadone poisoning Forensic Science International 2010 196 (1-3): 51-54 Pascal Kintz, Julie Evans, Marion Villain and Vincent Cirimele
24. Non-fatal overdose in the 12 months following treatment for substance use disorders Drug and Alcohol Dependence 2010 107 (1): 51-55
5 Peter C. Britton, James D. Wines Jr and Kenneth R. Conner
25. Over 1200 drugs-related deaths and 190,000 opiate-user-years of follow- up: Relative risks by sex and age group Addiction Research and Theory 2010 1 (2): 194–207 Sheila M. Bird
26. Denial in alcohol and other drug use disorders: A critique of theory Addiction Research & Theory 2010 18 (2): 181-193 Patricia Ann Stoddard Dare and Leaanne Derigne
27. An evaluation of a heroin overdose prevention and education campaign Drug and Alcohol Review 2010 29: 5–11 Danielle Horyniak, Peter Higgs, Jennifer Lewis, Rebecca Winter, Paul Dietze and Campbell Aitken
Effectiveness of treatment
28. Effect of co-occurring disorders and intimate partner violence on substance abuse treatment outcomes Journal of Substance Abuse Treatment 2010 38 (3): 231-244 Sherry Lipsky, Antoinette Krupski, Peter Roy-Byrne, Barbara Lucenko, David Mancuso and Alice Huber
Epidemiology and Demography
29. Healthcare and Medical Graduates of 2009: Their Reactions to Four Key Proposals in the Scottish Government’s Strategy for Tackling Alcohol Misuse Alcohol Alcohol 2010 45: 200-206 Jan S. Gill, Caroline Gibson and Maggie Nicol
30. Gender-related differences in the pharmacokinetics of opiates Forensic Science International 2010 194 (1-3): 28-33 Maja Djurendic-Brenesel, Neda Mimica-Dukic, Vladimir Pilija and Milos Tasic
31. Patterns of illegal drug use among an adult alcohol dependent population: Results from the National Survey on Drug Use and Health Drug and Alcohol Dependence 2010 106 (2-3): 119-125 S.L. Hedden, S.S. Martins, R.J. Malcolm, L. Floyd, C.E. Cavanaugh nd W.W. Latimer
32. The nature and extent of illegal drug and alcohol-related litter in Scottish social housing community: A photographic investigation Addiction Research and Theory 2010 18 (1): 71–83 Alasdair J. M. Forsyth and Neil Davidson
6 33. Substance use among late adolescent urban youths: Mental health and gender influences Addictive Behaviours 2010 35 (1): 30-34 Traci M. Schwinn, Steven P. Schinke and Danielle N. Trent
34. Comorbidity of generalized anxiety disorder and alcohol use disorders among individuals seeking outpatient substance abuse treatment Addictive Behaviours 2010 35 (1): 42-45 Joshua P. Smith and Sarah W. Book
35. Mortality and cause of death among 1705 illicit drug users: A 37 year follow up Drug and Alcohol Review 2010 29 (1): 21-27 Marlene Stenbacka, Anders Leifman, Anders Romelsjö
36. Impact of Self-Reported Life Events on the Profile of Opioid Dependence Syndrome The American Journal of Drug and Alcohol Abuse 2010 36: 7–12 Hamdy F. Moselhy, Ehsan Fahmy, Victor Samy Mikhael and Hussein El- Sheikh
37. Opiate and crack cocaine use: A new understanding of prevalence Drugs: education, prevention and policy 201017 (2): 135–147 Gordon Hay, Maria Gannon, Jane Macdougall, Catherine Eastwood, Kate Williams and Tim Millar
38. Linkage Analysis of Alcohol Dependence Symptoms in the Community Clinical and Experimental Research 2010 34 (1): 158-163 Narelle K. Hansell, Arpana Agrawal, John B. Whitfield, Katherine I. Morley, Scott D. Gordon, Penelope A. Lind, Michele L. Pergadia, Grant W. Montgomery, Pamela A. F. Madden, Richard D. Todd, Andrew C. Heath, Nicholas G. Martin
Harm Reduction
39. Route transition interventions: Potential public health gains from reducing or preventing injecting International Journal of Drug Policy 2010 21 (2): 125-128 Jamie Bridge
40. Normalization and harm reduction: Research avenues and policy agendas International Journal of Drug Policy 2010 21 (2): 137-139 Patricia G. Erickson and Andrew D. Hathaway
41. ‘Does anyone know where to get fits from around here?’ Policy implications for the provision of sterile injecting equipment through pharmacies in Sydney, Australia Drugs: Education, Prevention, and Policy 2010 17 (1): 72-83
7 Carla Treloar, Max Hopwood and Joanne Bryant
42. The impact of a supervised injecting facility on ambulance call-outs in Sydney, Australia Addiction 2010 105 (4): 676-683 Allison M. Salmon, Ingrid van Beek, Janaki Amin, John Kaldor and Lisa Maher
43. Syringe exchange, injecting and intranasal drug use Addiction 2010 105(1): 155-158754747 155.158 Don C. Des Jarlais, Kamyar Arasteh, Courtney McKnight, Martin Ringer & Samuel R. Friedman
Homelessness
44. Biological markers of problem drinking in homeless patients Addictive Behaviours 35 (3): 260-262 Henrik Thiesen and Morten Hesse
Injecting Behaviour
45. Impact of injecting drug use on mortality in Danish HIV-infected patients: a nation-wide population-based cohort study Addiction 2010 105 (3): 529-535 Mette V. Larsen, Lars H. Omland, Jan Gerstoft, Carsten S. Larsen, Janne Jensen, Niels Obel and Gitte Kronborg
Miscellaneous
46. Tobacco, cocaine, and heroin: Craving and use during daily life Addictive Behaviours 2010 35 (4): 318-324 David H. Epstein, Gina F. Marrone, Stephen J. Heishman, John Schmittner and Kenzie L. Preston
47. The abuse potential of the synthetic cannabinoid nabilone Addiction 2010 105 (3): 494-503 Mark A. Ware and Emmanuelle St Arnaud-Trempe
48. The 10 most important things known about addictionadd_2673 613 Addiction 2010 105 (1): 6-13 Doug Sellman
49. Guilty until proven innocent: A qualitative study of the management of chronic non-cancer pain among patients with a history of substance abuse Addictive Behaviours 35 (3): 270-272 Alex Baldacchino, Gail Gilchrist, Rod Fleming and Jonathan Bannister
8 Opiate Treatment
50. Preference for buprenorphine/naloxone and buprenorphine among patients receiving buprenorphine maintenance therapy in France: A prospective, multicenter study Journal of Substance Abuse Treatment 2010 38 (1): 83-89 Jean-Pierre Daulouède, Yves Caer, Pascal Galland, Pierre Villeger, Emmanuel Brunelle, Jérôme Bachellier, Jean-Michel Piquet, Jean Harbonnier, Yves Leglise and Pascal Courty
51. A heroin prescription trial: Case studies from Montreal and Vancouver on crime and disorder in the surrounding neighbourhoods International Journal of Drug Policy 2010 21: 28–35 Benoit Lasniera, Serge Brochub, Neil Boyd and Benedikt Fischerd
52. Why don’t out-of-treatment individuals enter methadone treatment programmes? International Journal of Drug Policy 2010 21: 36–42 James A. Peterson, Robert P. Schwartz, Shannon Gwin Mitchell, Heather Schacht Reisinger, Sharon M. Kelly, Kevin E. O’Grady, Barry S. Brown and Michael H. Agar
53. A cost-benefit and cost-effectiveness analysis of Vancouver’s supervised injection facility International Journal of Drug Policy 2010 21: 70–76 Martin A. Andresen and Neil Boyd
54. Dissolution of a harm reduction track for opiate agonist treatment: Longitudinal impact on treatment retention, substance use and service utilization International Journal of Drug Policy 2010 21: 82–85 Bryan Hartzler, Ann J. Cotton, Donald A. Calsyn, Rachael Guerra and Edward Gignoux
55. Methadone Maintenance Dosing Guideline for Opioid Dependence, a Literature Review Journal of Addictive Diseases 2010 29: 1–14 Ayman Fareed, Jennifer Casarella, Richard Amar, Sreedevi Vayalapalli and Karen Drexler
56. Provision of Ancillary Medications During Buprenorphine Detoxification Does Not Improve Treatment Outcomes Journal of Addictive Diseases 2010 29 (1): 23-29 Maureen Hillhouse, Catherine P. Domier, David Chim and Walter Ling
57. Obstructive sleep apnea is more common than central sleep apnea in methadone maintenance patients with subjective sleep complaints Drug and Alcohol Dependence 2010 108 (1-2): 77-83 Katherine M. Sharkey, Megan E. Kurth, Bradley J. Anderson, Richard P. Corso, Richard P. Millman and Michael D. Stein
9 58. Alcohol usage and associated treatment outcomes for opiate users entering treatment in Ireland Drug and Alcohol Dependence 2010 107(1): 55-61 R.D. Stapleton and C.M. Comiskey
59. Long-term outcomes of office-based buprenorphine/naloxone maintenance therapy Drug and Alcohol Dependence 2010 106 (1): 56-60 T.V. Parran, C.A. Adelman, B. Merkin, M.E. Pagano, R. Defranco, R.A. Ionescu and A.G. Mace
60. Mood Disturbance and Withdrawal Severity in Substitution Treatment for Opioid Dependence: Their Association and Impact on Continued Illicit Drug Use Addictive Disorders & Their Treatment 2010 9 (1): 1-7 Kettler, Lisa, Nikic, Mathew, Newcombe, David and Ali, Robert
61. The acceptability of combined methadone-naloxone treatment: Consumer and provider views on the potential utility of methadone- naloxonedar_118 138..143 Drug and Alcohol Review 2010 29: 138–143 James Shearer, Kristie Mammen and James Bell
62. Drug injecting in patients in New Zealand Methadone Maintenance Drug and Alcohol Review 2010 29: 41–46 Treatment programs: An anonymous survey Graeme Judson, Rupert Bird, Patrick O’connor, Tim Bevin, Richard Loan, Martin Schroder, Richard Mcgrath, Mark Weatherall, Helen Moriarty& Geoff Robinson
63. The Andalusian trial on heroin-assisted treatment: A 2 year follow- updar_100.80 Drug and Alcohol Review 2010 29: 75–80 Eugenia Oviedo-Joekes, Joan C. March, Manuel Romero & Emilio Perea- Milla5
64. Abuse liability of intravenous buprenorphine/naloxone and buprenorphine alone in buprenorphine-maintained intravenous heroin abusers Addiction 2010 105 (4): 709-718 Sandra D. Comer, Maria A. Sullivan, Suzanne K. Vosburg, Jeanne Manubay, Leslie Amass, Ziva D. Cooper, Phillip Saccone and Herbert D. Kleber
65. The effect of time spent in treatment and dropout status on rates of convictions, cautions and imprisonment over 5 years in a primary care- led methadone maintenance service Addiction 2010 105 (4): 732-739 Phillip Oliver, Jenny Keen, Georgina Rowse, Elizabeth Ewins, Laura Griffiths, Nigel Mathers
10 66. Does opioid substitution treatment in prisons reduce injecting-related HIV risk behaviours? A systematic review Addiction 2010 105 (2): 216-223 Sarah Larney
67. Outcome of long-term heroin-assisted treatment offered to chronic, treatment-resistant heroin addicts in the Netherlands Addiction 2010 105 (2): 300-308 Peter Blanken, Vincent M. Hendriks, Jan M. van Ree and Wim van den Brink
68. Problems experienced by community pharmacists delivering opioid substitution treatment in New South Wales and Victoria, Australia Addiction 2010 105 (2): 335-342 Adam R. Winstock, Toby Lea and Janie Sheridan
69. Heroin-assisted treatment in Switzerland: a case study in policy change Addiction 2010 105 (1): 29-37 Ambros Uchtenhagen
Organisation of Treatment
70. Using enhanced and integrated services to improve response to standard methadone treatment: Changing the clinical infrastructure of treatment networks Journal of Substance Abuse Treatment 2010 38 (2): 170-177 Karin Neufeld, Michael Kidorf, Van King, Ken Stoller, Michael Clark, Jessica Peirce and Robert K. Brooner
Pregnancy
71. Brief screening questionnaires to identify problem drinking during pregnancy: a systematic review Addiction 2010 105 (4): 601-614 Ethel Burns, Ron Gray and Lesley A. Smith
Psychostimulants
72. Randomized controlled trial of dexamphetamine maintenance for the treatment of methamphetamine dependence_ Addiction 2010 105 (1): 146-154754 Marie Longo, Wendy Wickes, Matthew Smout, Sonia Harrison, Sharon Cahill & Jason M. White
11 Public Health
73. Prevention programs in the 21st century: what we do not discuss in public Addiction 2010 105 (4): 578-581 Harold Holder
74. How much alcohol do you buy? A comparison of self-reported alcohol purchases with actual sales Addiction 2010 105 (4): 649-654 Mats Ramstedt
75. Policy options for alcohol price regulation: the importance of modelling population heterogeneity Addiction 2010 105 (3): 383-393 Petra Sylvia Meier, Robin Purshouse, Alan Brennan
Research Methods
76. The reliability and validity of drug users' self reports of amphetamine use among primarily heroin and cocaine users Addictive Behaviours 2010 35 (4): 350-354 Lucy E. Napper, Dennis G. Fisher, Mark E. Johnson and Michele M. Wood
77. The challenge of external validity in policy-relevant systematic reviews: a case study from the field of substance misuse_ Addiction 2010 105(1): 136-1457 Mark Pearson & Ross Coomber
Young people
78. Impact of a Social Skills Intervention on the Hostile Attributions of Children With Prenatal Alcohol Exposure Alcoholism: Clinical Experimental Research 2010 34 (2): 231-241 Vivien Keil, Blair Paley, Fred Frankel and Mary J. O'Connor
79. Young people and drugs: Next generation of harm reduction International Journal of Drug Policy 2010 21 (2): 12-114 Simona Merkinaite, Jean Paul Grund and Allen Frimpong
80. Do parents and school matter? Protective factors for adolescent substance use Addictive Behaviours 2010 35 (1): 53-56 Bettina F. Piko and Eszter Kovács
81. Using sensation seeking to target adolescents for substance use interventions Addiction 2010 105 (3): 506-514 James D. Sargent, Susanne Tanski, Mike Stoolmiller and Reiner Hanewinkel
12 List of Abstracts
Alcohol
1. Alcohol Intake and Systemic Markers of Inflammation—Shape of the Association According to Sex and Body Mass Index Alcohol Alcohol 2010 45: 119-125 Andreia Oliveira, Fernando Rodríguez-Artalejo, and Carla Lopes
ABSTRACT Aims: To assess the association of alcohol intake with high-sensitivity C-reactive protein (hs-CRP), uric acid and leukocyte count in blood, and whether sex and body mass index (BMI) modify these associations. Methods: Individuals aged 18 years were randomly selected from the population of Porto, Portugal (70% of participation). A total of 840 women and 490 men with reliable information on inflammatory markers and alcohol intake, obtained from a validated food frequency questionnaire, were studied. Associations and their respective trends were estimated from generalized linear models, with adjustment for potential confounders. Analyses were stratified by sex and BMI. Results: In women, adjusted hs-CRP levels (mg/l) were 2.69 in non-drinkers, 2.25 in drinkers of >0– 15 g alcohol/day, 2.32 in drinkers of >15–30 g alcohol/day and 3.18 in drinkers of >30 g alcohol/day (P-value for the quadratic trend <0.001). In men, the association between alcohol intake and hs-CRP was positive and linear (P-value for the linear trend = 0.014). Alcohol intake was also positively and linearly associated with uric acid in each sex. Body weight modified these associations, which remained statistically significant only in normal-weight (BMI <25 kg/m2) women and overweight (BMI 25 kg/m2) men for hs-CRP, and in normal-weight individuals for uric acid. No significant association between alcohol intake and leukocyte count was found. Conclusions: The association of alcohol intake with hs-CRP was J-shaped in women but positive and linear-shaped in men. Alcohol intake was directly associated with uric acid in men and women. BMI modifies the effect of alcohol on hs-CRP and uric acid levels in each sex.
2. Analysis of the Factors Determining Survival of Alcoholic Withdrawal Syndrome Patients in a General Hospital Alcohol & Alcoholism 2010 45 (2): 151–158 R. Monte, R. Rabuñal, E. Casariego, H. López-Agreda, A. Mateos and S. Pértega
ABSTRACT Aim: To investigate the clinical variables associated with the risk of dying and the causes of death during the course of alcoholic withdrawal syndrome (AWS) in a general hospital. Methods: Cohort study of AWS patients admitted to Xeral Hospital in Lugo, Spain between 1987 and 2003. The characteristics of patients who died were contrasted with those who survived. The different clinical, epidemiological and biochemical variables reflective of alcohol consumption habits, basal health status and presentation features of the syndrome and its complications were all recorded. Results: There were 539 episodes of hospitalization for AWS in 436 patients (mean age 45.0, SD 12.0, 91.3% males), 71.1% of whom presented with delirium tremens. A total of 29 patients died, yielding a 6.6% mortality rate (95% confidence interval, CI: 4.2–9.1%). Eighteen patients (62%) died after being admitted to the intensive care unit (ICU). The following independent variables were associated with the risk of dying in a multivariate logistic regression model: cirrhosis [odds ratio (OR) 4.8 (95% CI 1.5– 14.6), P = 0.006]; presenting with delirium tremens at diagnosis [OR 3.5 (95% CI 1.3–8.9), P = 0.008]; the existence of an underlying chronic pathology other than liver disease [OR 2.5 (95% CI 1–6.1), P = 0.01]; and the need for orotracheal intubation [OR 2.9 (95% CI 1.1–7.9), P = 0.03], especially if pneumonia requiring ICU is added [OR 8 (95% CI 3–21.3), P < 0.001]. Receiver operating characteristic analysis revealed an area under the curve of 0.818 (95% CI 0.742–0.894). Conclusions: The factors determining survival after admission to a general hospital for alcoholic withdrawal syndrome depend on the intensity of clinical manifestations (delirium tremens, ICU, orotracheal intubation) and the presence of associated comorbidity.
13 3. Methodological Assessment of Economic Evaluations of Alcohol Treatment: What Is Missing? Alcohol Alcohol 2010 45: 53-63 Carolina Barbosa, Christine Godfrey, and Steve Parrott
ABSTRACT Aim: The aim of this study is to review the methodology that has been adopted in previous economic evaluations of alcohol treatment and offer research recommendations with a view to enhancing the consistency and harmonization of economic evaluations in the alcohol field. Methods: Published full economic evaluations of alcohol treatment were retrieved using a systematic search. The studies were analysed in terms of the identification, measurement and valuation methods used to assess the society-level consequences and the methods used to carry out the analysis of individual-level consequences and costs of the intervention. A taxonomy of alcohol-related consequences was developed and used as a framework for the methodology extraction. Results: Twenty- seven studies were selected. Almost half of the studies did not include society-level consequences in their analysis. Some consequences of alcohol treatment at a societal level, such as the impact of treatment on health-related quality of life of family and friends of the drinker, have never been considered in the economic analysis. There was no agreement regarding the individual health consequences used in the evaluations. Measures capturing life years and morbidity have not been extensively used in the alcohol field. The level of reporting treatment costs on the reviewed studies is generally well detailed. Conclusion: The literature is still rather sparse in this area and further research is required to fulfil the gaps. If a common methodology is adopted in future economic evaluations of alcohol treatment, more stable cost-effectiveness estimates will be produced and informed decisions for resources allocation to alcohol treatments will be possible.
4. Planned and Unplanned Discharge from Alcohol Services in Scotland, 2004– 2008 Alcohol Alcohol 2010 45: 64-69. Rosemary Newham, Christopher Russell, and John B. Davies
ABSTRACT Aims: Available data suggests that the rate of unplanned discharge from alcohol treatment services is an international problem reflective, perhaps, of ambivalence surrounding treatment in general. Given Scotland's escalating prevalence of alcohol misuse, a preliminary study of Scottish dropout rates would make a useful contribution to the international scene. Methods: A retrospective analysis of discharge statuses (planned/unplanned/disciplinary) of entries to alcohol treatment services between 1 April 2004 and 31 March 2008 was conducted on data provided by 10 regional Drug and Alcohol Action Teams (DAATs) and three individual treatment providers. Results: Of 48,299 cases, 52.23% (n = 25,231) were unplanned discharges. Data showed a general increasing trend in the rate of planned discharges across the examined 4-year period, from 41.66% in 2004–2005 to 51.94% in 2007–2008. Inspection of the data revealed marked regional variations in ratios of planned to unplanned discharge, with only four of the 10 regions examined reporting a planned discharge rate >50%. Conclusion: More than one of every two entries to alcohol misuse services between 2004 and 2008 resulted in an unplanned discharge. The trend of improvement over the examined 4-year period was not consistent for all regions. A comparison of this figure with available US and Welsh data is made. The importance of these data in assessing the cost-effectiveness of alcohol treatment services and implications for policy making is discussed.
5. Ecological Associations of Alcohol Outlets With Underage and Young Adult Injuries
14 Alcoholism: Clinical Experimental Research. 2010 34: 519-527 Paul J. Gruenewald, Bridget Freisthler, Lillian Remer, Elizabeth A. LaScala, Andrew J. Treno, and William R. Ponicki
KEYWORDS Alcohol Outlets • Underage Drinking • Young Adult Drinking • Drinking-Related Problems • Hospital Discharges
ABSTRACT Objective: This paper argues that associations between rates of 3 specific problems related to alcohol (i.e., accidents, traffic crashes, and assaults) should be differentially related to densities of alcohol outlets among underage youth and young adults based upon age-related patterns of alcohol outlet use. Methods: Zip code-level population models assessed local and distal effects of alcohol outlets upon rates of hospital discharges for these outcomes. Results: Densities of off-premise alcohol outlets were significantly related to injuries from accidents, assaults, and traffic crashes for both underage youth and young adults. Densities of bars were associated with more assaults and densities of restaurants were associated with more traffic crash injuries for young adults. Conclusions: The distribution of alcohol-related injuries relative to alcohol outlets reflect patterns of alcohol outlet use.
6. Effect of motivational interviewing on reduction of alcohol use Drug and Alcohol Dependence 2010 107 (1): 23-30 Adeline Nyamathi , Steven Shoptaw, Allan Cohen, Barbara Greengold, Kamala Nyamathi, Mary Marfisee, Viviane de Castro, Farinaz Khalilifard, Daniel George and Barbara Leake
KEYWORDS Alcohol use; Methadone-maintained; Motivational interviewing; Nurse-led hepatitis health promotion
ABSTRACT Background Methadone-maintained (MM) clients who engage in excessive alcohol use are at high risk for HIV and hepatitis B virus (HBV) infection. Nurse-led hepatitis health promotion (HHP) may be one strategy to decrease alcohol use in this population. Objective To evaluate the impact of nurse-led HHP, delivered by nurses compared to motivational interviewing (MI), delivered by trained therapists in group sessions or one-on-one on reduction of alcohol use. Methods A three-arm randomized, controlled trial, conducted with 256 MM adults attending one of five MM outpatient clinics in the Los Angeles area. Within each site, moderate-to-heavy alcohol-using MM participants were randomized into one of three conditions: (1) nurse-led hepatitis health promotion group sessions (n = 87); (2) MI delivered in group sessions (MI-group; n = 79), or (3) MI delivered one-on-one sessions (MI-single, n = 90). Results Self-reported alcohol use was reduced from a median of 90 drinks/month at baseline to 60 drinks/month at 6-month follow-up. A Wilcoxon sign-rank test indicated a significant reduction in alcohol use in the total sample (p < .05). In multiple logistic regression analysis controlling for alcohol consumption at baseline and other covariates, no differences by condition were found. Discussion As compared to two programs delivered by MI specialists, a culturally-sensitive and easy to implement nurse-led HHP program produced similar reductions in alcohol use over 6 months. Employing nurse-led programs may allow cost savings for treatment programs as well as a greater integration of alcohol reduction counseling along with a more comprehensive focus on general health- related issues than previously conducted.
15 7. Moderators and mediators of two brief interventions for alcohol in the emergency department Addiction 2010 105 (3): 452-465 Nancy P. Barnett, Timothy R. Apodaca, Molly Magill, Suzanne M. Colby, Chad Gwaltney, Damaris J. Rohsenow and Peter M. Monti
KEYWORDS Alcohol • brief intervention • emergency room
ABSTRACT Objective To evaluate moderators and mediators of brief alcohol interventions conducted in the emergency department. Methods Patients (18–24 years; n = 172) in an emergency department received a motivational interview with personalized feedback (MI) or feedback only (FO), with 1- and 3-month booster sessions and 6- and 12-month follow-ups. Gender, alcohol status/severity group [ALC+ only, Alcohol Use Disorders Identification Test (AUDIT+) only, ALC+/AUDIT+], attribution of alcohol in the medical event, aversiveness of the event, perceived seriousness of the event and baseline readiness to change alcohol use were evaluated as moderators of intervention efficacy. Readiness to change also was evaluated as a mediator of intervention efficacy, as were perceived risks/benefits of alcohol use, self-efficacy and alcohol treatment seeking. Results Alcohol status, attribution and readiness moderated intervention effects such that patients who had not been drinking prior to their medical event, those who had low or medium attribution for alcohol in the event and those who had low or medium readiness to change showed lower alcohol use 12 months after receiving MI compared to FO. In the AUDIT+ only group those who received MI showed lower rates of alcohol-related injury at follow-up than those who received FO. Patients who had been drinking prior to their precipitating event did not show different outcomes in the two interventions, regardless of AUDIT status. Gender did not moderate intervention efficacy and no significant mediation was found. Conclusions Findings may help practitioners target patients for whom brief interventions will be most effective. More research is needed to understand how brief interventions transmit their effects.
8. Predictors of hangover during a week of heavy drinking on holiday Addiction 2010 105 (3): 476-483 Morten Hesse and Sébastien Tutenges
KEYWORDS Binge drinking • hangover • heavy drinking • nightlife tourism • prospective study • youth
ABSTRACT Aims To investigate predictors of hangover during a week of heavy drinking in young adults. Design Observational prospective study. Methods A total of 112 young Danish tourists were interviewed on three occasions during their holiday. They completed the Acute Hangover Scale and answered questions about their alcohol consumption and rest duration. The incidence of hangover was analysed as the proportion of heavy drinkers (i.e. those reporting drinking more than 12 standard units of alcohol during the night before) scoring above the 90th percentile of light drinkers (i.e. those who had consumed fewer than seven standard units the night before). We estimated the course and predictors of hangover using random effects regression. Results The incidence of hangover was 68% after drinking more than 12 standard units in the whole sample. The severity of hangover increased significantly during a week of heavy drinking and there was a time × number of drinks interaction, indicating that the impact of alcohol consumed on hangover became more pronounced later in the week. Levels of drinking before the holiday did not predict hangover. Conclusions Hangovers after heavy drinking during holidays appear to be related both to amount drunk and time into the holiday.
16 9. The dimensionality of alcohol use disorders and alcohol consumption in a cross-national perspective Addiction 2010 105 (2): 240-254 Guilherme Borges, Yu Ye, Jason Bond, Cheryl J. Cherpitel, Mariana Cremonte, Jacek Moskalewicz, Grazyna Swiatkiewicz and Maritza Rubio-Stipec
KEYWORDS Alcohol use disorder • DSM-IV • ethnicity • heavy drinking • IRT analysis
ABSTRACT Aims To replicate the finding that there is a single dimension trait in alcohol use disorders and to test whether the usual 5+ drinks for men and 4+ drinks for women and other measures of alcohol consumption help to improve alcohol use disorder criteria in a series of diverse patients from emergency departments (EDs) in four countries. Design Cross-sectional surveys of patients aged 18 years and older that reflected consecutive arrival at the ED. The Composite International Diagnostic Interview Core was used to obtain a diagnosis of DSM-IV alcohol dependence and alcohol abuse; quantity and frequency of drinking and drunkenness as well as usual number of drinks consumed during the last year. Setting Participants were 5195 injured and non-injured patients attending seven EDs in four countries: Argentina, Mexico, Poland and the United States (between 1995–2001). Findings Using exploratory factor analyses alcohol use disorders can be described as a single, unidimensional continuum without any clear-cut distinction between the criteria for dependence and abuse in all sites. Results from item response theory analyses showed that the current DSM-IV criteria tap people in the middle–upper end of the alcohol use disorder continuum. Alcohol consumption (amount and frequency of use) can be used in all EDs with the current DSM-IV diagnostic criteria to help tap the middle–lower part of this continuum. Even though some specific diagnostic criteria and some alcohol consumption variables showed differential item function across sites, test response curves were invariant for ED sites and their inclusion would not impact the final (total) performance of the diagnostic system. Conclusions DSM-IV abuse and dependence form a unidimensional continuum in ED patients regardless of country of survey. Alcohol consumption variables, if added, would help to tap patients with more moderate severity. The DSM diagnostic system for alcohol use disorders showed invariance and performed extremely well in these samples.
10. Efficacy of repetitive transcranial magnetic stimulation in alcohol dependence: a sham-controlled studyadd Addiction 2010 105 (1): 59-557 45 Biswa R. Mishra, S. Haque Nizamie, Basudeb Das & Samir K. Praharaj
KEYWORDS Alcoholism, craving, dorsolateral pre-frontal cortex (DLPFC), efficacy, sham control, transcranial magnetic stimulation (TMS).
ABSTRACT Objective To study the anticraving efficacy of high-frequency repetitive transcranial magnetic stimulation (rTMS) of the right dorsolateral pre-frontal cortex (DLPFC) in patients with alcohol dependence. Methods We performed a prospective, single-blind, sham-controlled study involving 45 patients with alcohol dependence syndrome (according to ICD-10 DCR), with Clinical Institute of Withdrawal Assessment in Alcohol Withdrawal (CIWA-Ar) scores _10. Patients were allocated to active and sham rTMS in a 2 : 1 ratio, such that 30 patients received active and 15 patients sham rTMS to the right DLPFC (10 Hz frequency, 4.9 seconds per train, inter-train interval of 30 seconds, 20 trains per session, total 10 sessions). The Alcohol Craving Questionnaire (ACQ-NOW) was administered to measure the severity of alcohol craving at baseline, after the last rTMS session and after 1 month of the last rTMS session. Results Two way repeated-measures analysis of variance (ANOVA) showed significant reduction in the post-rTMS ACQ-NOW total score and factor scores in
17 the group allocated active rTMS compared to the sham stimulation. The effect size for treatment with time interaction was moderate (h2 = 0.401). Conclusions Right dorsolateral pre-frontal highfrequency rTMS was found to have significant anticraving effects in alcohol dependence. The results highlight the potential of rTMS which, combined with other anticraving drugs, can act as an effective strategy in reducing craving and subsequent relapse in alcohol dependence.
11. Age-Related Gray Matter Shrinkage in a Treatment Naïve Actively Drinking Alcohol-Dependent Sample Alcoholism: Clinical and Experimental Research 2010 34 (1): 175-182 George Fein, Ryan Shimotsu, Jerome Barakos
KEYWORDS Alcohol Dependence • Structural MRI • Brain Shrinkage • Gray Matter • Aging
ABSTRACT Background: We previously demonstrated, in a small sample, steeper age-related gray matter shrinkage in treatment naïve alcohol-dependent (TxN) men compared to nonalcoholic controls, but could not separate out the contributions of age and lifetime duration of alcohol use (which were highly correlated) to this effect. In the current study, we have quadrupled the sample size and expanded it to include both men and women to try to replicate and extend the previous findings and to separate the contributions of age and alcohol use to the phenomenon. Methods: In the current study, we examine cortical gray matter volumes in 18- to 50-year-old TxN (n = 84) versus age and gender comparable controls (n = 67). We used a new Region of Interest Analysis method which accounts for differences in sulcal and gyral enfolding between individuals ( Fein et al., 2009a). Results: We found greater age-related gray matter shrinkage in TxN than in controls. Partial correlation analysis showed that the effect was a function of age and not lifetime alcohol burden. Conclusions: Implications of the findings are discussed in terms of their contribution toward our knowledge of differences between different subpopulations of alcoholics and in terms of their implications for the morbidity of alcohol dependence in an aging national population.
Blood borne viruses
12. Hepatitis B virus among injecting drug users in Sydney, Australia: Prevalence, vaccination and knowledge of status Drug and Alcohol Independence 2010 108 (1-2): 134-137 Carolyn A. Day, Bethany White, Gregory J. Dore, Ingrid van Beek, Craig Rodgers, Philip Cunningham, Alex Wodak and Lisa Maher,
KEYWORDS Hepatitis B virus; Vaccination; Injecting drug users
ABSTRACT Background Despite the availability of an inexpensive and safe vaccine, injecting drug users (IDUs) remain at risk of hepatitis B virus (HBV) infection. This paper aimed to measure HBV prevalence and vaccination coverage and to assess knowledge and concordance of status among IDUs. Methods Participants were recruited through a primary health care and a drug treatment service and via street press in Sydney, Australia. Face-to-face interviews were conducted and serology collected. All received $30 for participation. Results 229 participants were recruited, serology was available for 209. Almost all those interviewed had been tested for HBV (95%) a median of four (IQR 2–10) times and 61% had been tested in the preceding year. Fifty-four percent had evidence of previous infection (anti-HBc) and 5% were HBsAg positive. Only 27% had serological evidence of vaccination immunity; however, 43% of the sample recalled
18 having being told by a health professional that they were vaccinated against HBV. Although only three participants reported they did not understand the results of their last HBV test, confusion was evident based on self-reported status. Conclusions Levels of understanding and vaccination coverage were low while evidence of prior infection was high among this IDU sample. This is cause for concern given the majority of participants were recruited through primary care and treatment services. Strategies to bolster vaccination among this group will be discussed.
13. Needle sharing in regular sexual relationships: An examination of serodiscordance, drug using practices, and the gendered character of injecting Drug and Alcohol Dependence 2010 107: 182–187 Joanne Bryant, Loren Brener, Peter Hull, Carla Treloar
KEYWORDS Injecting drug use (IDU); Heterosexual relationships; Risk behaviours; Serodiscordance; Gender
ABSTRACT Background This paper examines correlates of needle and other equipment sharing among injecting drug users (IDU) in regular heterosexual relationships. Methods A cross-sectional survey collected data from people obtaining sterile needles and syringes from pharmacies in New South Wales, Australia. 181 IDU in regular heterosexual relationships provided information about their own drug and injecting practices and those of their partners. Results Compared to female partners, male partners reported more frequent injecting, more commonly injected their partners, scored and prepared the drugs, and obtained the needles. Couples were less likely to share needles with each other if they reported a low-to-moderate connection with drug using networks compared to a moderate-to-high connection (AOR 0.4, 95% CI 0.19–0.95) or if the respondent partner reported sharing injecting equipment (needles and/or ancillary equipment) with friends in the last 6 months (AOR 3.2, 95% CI 1.34–7.86). Couples were more likely to share ancillary equipment with each other if they spent most or all of their injecting time together (AOR 4.1, 95% CI 1.40–11.31) or if the respondent reported sharing injecting equipment with friends (AOR 5.3, 95% CI 1.73–16.37). Couples with discordant hepatitis C status were no more or less likely than those with concordant status to share needles or ancillary injecting equipment. Conclusions Injecting practices in regular heterosexual relationships do not appear to be organised around hepatitis C status but are influenced by gender, the couples’ connection with other IDU, and extent to which they share the equipment with those outside of their relationship.
14. Antibody response to hepatitis B vaccine in substance use disorder patients Drug and Alcohol Dependence 2010 107 (1): 39-43 Hildi J. Hagedorn, Nancy A. Rettmann, Eric W. Dieperink, Janet Durfee and Bashar Aqel
KEYWORDS Hepatitis B vaccine; Substance use disorders; Substance abuse treatment programs; Hepatitis services; Veterans
ABSTRACT The objectives of this study were to assess the prevalence of prognostic factors previously known to be associated with poor antibody response to hepatitis B vaccination in a sample of veterans presenting for substance use disorders treatment at a Veterans Health Administration (VA) Medical
19 Center, assess vaccination response, and identify markers for poor response in this population. Results indicated that most participants had multiple prognostic factors previously known to be associated with poor antibody response including male gender, age over 40, smoking, and obesity. The rate of seroconversion in this sample was 51.9%. This is substantially lower than seen in healthy adults. Alcohol dependence was the only significant independent negative predictor of seroconversion in this sample. Substance use disorders treatment providers who are considering adding hepatitis B vaccination services to their clinics should be aware that the antibody response to the hepatitis B vaccination is inconsistent and that patients with particular demographic characteristics may be at heightened risk of poor antibody response.
15. The Relationship between Performance on the Shipley Institute of Living Scale (SILS) and Hepatitis C Infection among Active Injection Drug Users in Baltimore, Maryland The American Journal of Drug and Alcohol Abuse 2010 36: 61–65 Stevan Geoffrey Severtson, Mary M. Mitchell, Alicia Hubert, and William Latimer, John Hopkins
ABSTRACT Background: Hepatitis C represents a significant public health problem, particularly among injection drug users. Other than injection drug practices, little is understood about individual level characteristics that may place some injection drug users at particularly high risk. Objectives: The current study sought to examine two associations among active, regular heroin injection drug users. The first was to determine whether there was an association between two scales from the Shipley Institute of Living Scale (SILS: a neuropsychological measure used to estimate cognitive impairment/intellectual functioning) and self-reported preexisting conditions independent of years of drug use. The second was to examine whether performance on the scales was associated with hepatitis C infection. Methods: Data from 260 HIV negative injection drug users from the Baltimore metropolitan region were used. Participants completed a risk behavior interview, brief neuropsychological battery, and were tested for Hepatitis C. Results: Findings indicated that scale performances varied by self-reported learning disabilities and attention deficit disorder. Poorer performance on one scale was statistically significantly associated with greater hepatitis C prevalence on the vocabulary scale, the discrepancy scale showed a statistical trend. Conclusions: Cognitive impairment measured among this sample of injection drug use was related to pre-existing conditions and hepatitis C independent of years of drug use. Such impairment may exist prior to initiation of use and increase vulnerability to poor health outcomes among injection drug users. Scientific Significance: This study highlights the need for interventions targeting a possible high risk subpopulation of injection drug users.
16. Can hepatitis C virus prevalence be used as a measure of injection-related human immunodeficiency virus risk in populations of injecting drug users? An ecological analysis Addiction 2010 105 (2): 311-318 Peter Vickerman, Matthew Hickman, Margaret May, Mirjam Kretzschmar and Lucas Wiessing
KEYWORDS Ecological analysis • epidemiology • hepatitis C • HIV • injecting drug use • systematic review
ABSTRACT Background Human immunodeficiency virus (HIV) outbreaks occur among injecting drug users (IDUs), but where HIV is low insight is required into the future risk of increased transmission. The relationship between hepatitis C virus (HCV) and HIV prevalence among IDUs is explored to determine whether HCV prevalence could indicate HIV risk. Methods Systematic review of IDU HIV/HCV prevalence data and regression analysis using weighted prevalence estimates and time–series data.
20 Results HIV/HCV prevalence estimates were obtained for 343 regions. In regions other than South America/sub-Saharan Africa (SAm/SSA), mean IDU HIV prevalence is likely to be negligible if HCV prevalence is <30% (95% confidence interval 22–38%) but increases progressively with HCV prevalence thereafter [linearly (β = 0.39 and R2 = 0.67) or in proportion to cubed HCV prevalence (β = 0.40 and R2 = 0.67)]. In SAm/SSA, limited data suggest that mean HIV prevalence is proportional to HCV prevalence (β = 0.84, R2 = 0.99), but will be much greater than in non-SAm/SSA settings with no threshold HCV prevalence that corresponds to low HIV risk. At low HCV prevalences (<50%), time–series data suggest that any change in HIV prevalence over time is likely to be much smaller (<25%) than the change in HCV prevalence over the same time-period, but that this difference diminishes at higher HCV prevalences. Conclusions HCV prevalence could be an indicator of HIV risk among IDUs. In most settings, reducing HCV prevalence below a threshold (30%) would reduce substantially any HIV risk, and could provide a target for HIV prevention.
17. The outcome of a rapid hepatitis B vaccination programme in a methadone treatment clinic Addiction 2010 105 (2): 329-334 Parameswaran Ramasamy, Nicholas Lintzeris, Yvonne Sutton, Helen Taylor, Carolyn A. Day and Paul S. Haber
KEYWORDS HBV • IDU • methadone • seroconversion • vaccination
ABSTRACT Aim Injecting drug users are a high-risk population for hepatitis B (HBV), but are difficult to engage in vaccination programmes. This study examines the completion rates of a HBV vaccination schedule and seroconversion in a group of patients in methadone maintenance treatment. Methods Patients at a public methadone maintenance programme in Sydney, Australia, were screened for viral hepatitis (hepatitis A, B and C) and offered a rapid HBV vaccination schedule (0, 1 and 2 months). Hepatitis B surface antibody (antiHBs) was retested on completion of the vaccination schedule. Results A total of 143 patients [71.3% male, mean age 33.1 (standard deviation ± 8.3)] enrolled in the project. Forty-nine per cent of patients were HAV antibody (Ab) positive, 81.1% hepatitis C virus (HCV) antibody (Ab) positive and 38.9% antiHBs positive. Exposure to multiple hepatitis viruses was common, with 24.5% testing positive for all three viruses. Seventy-three (83%) of the 88 antiHBs negative patients completed the vaccination schedule. Post-vaccination serology indicated a seroconversion rate of 75.4% (55 of 73) of completors, or 62.5% of eligible participants (55 of 88). Conclusion While there was a high rate of completion of the rapid vaccination schedule in this population, a moderate seroconversion rate was achieved. Further work is required to identify an optimal vaccination schedule in opioid substitution patients.
18. Combined effects of alcohol and hepatitis C: A secondary analysis of alcohol use biomarkers and high-risk behaviors from two medication trials for alcohol dependence Addictive Behaviours 2010 35 (2): 123-128 Jennifer G. Plebani, Carlos F. Tirado, Helen M. Pettinati, Kyle M. Kampman, Joseph R. Volpicelli and David W. Oslin
KEYWORDS: Hepatitis C; Alcohol dependence; CDT (carbohydrate-deficient transferrin); GGT (gamma glutamyl transpeptidase); Risk-assessment
ABSTRACT Objectives The goal of this secondary analysis was to examine the combined effects of HCV infection and recent alcohol use on baseline biologic markers of alcohol consumption in two outpatient medication trials for
21 alcohol dependence. In addition, the relationship between Hepatitis C virus (HCV) infection and behavioral risk factors for HCV infection in these clinical populations were examined. Methods Data (n = 345) from two randomized, placebo-controlled trials of naltrexone and psychosocial treatment for alcohol dependence (Study I, n = 212) and comorbid alcohol and cocaine dependence (Study II, n = 133) were used to examine baseline measures of HCV risk behaviors (injection drug use, needle sharing), and biomarkers of alcohol use (AST, ALT, GGT and CDT) were compared by HCV serostatus first within each study and then across studies. Results Although groups had differing sociodemographic profiles (as indicated by race, marital status, level of education) subjects in Study I exhibited no statistically significant differences from the Study II cohort in HCV prevalence (12.7 vs. 20.0%, p = 0.07), lifetime history of injection drug use (13.8 vs. 22.0%, p = 0.74), lifetime history of needle sharing (9.1 vs. 18.0%, p = 0.62). As such, the data from both studies were analyzed together. Regardless of drinking status, HCV infection was significantly associated with an upward shift in the baseline level of ALT, AST, and GGT (p < 0.006 for all measures) and a downward shift in baseline CDT (p = 0.002). When using standard laboratory cutoff values to determine clinically significant elevations, HCV seropositivity was significantly associated with elevations in ALT, AST, GGT (p < 0.001), and with decreases in CDT (p = .002). Conclusions These data emphasize the importance of evaluating HCV infection and HCV risk behaviors at intake in medication trials for alcohol dependence and also raise questions regarding the use of cutoff scores for ALT, AST, GGT and CDT levels as biologic markers of alcohol use in subjects when HCV status is unknown.
Co-Morbidity
19. Relationship between anxiety disorders and opiate dependence— A systematic review of the literature: Implications for diagnosis and treatment Journal of Substance Abuse Treatment 2010 38 (3): 220-230 Melina Fatséas, Cécile Denis, Estelle Lavie and Marc Auriacombe
KEYWORDS: Opiate dependence; Anxiety disorders; Prevalence; Clinical recommendations; Substance-induced disorder
ABSTRACT Our objective was to evaluate the prevalence and temporal sequence of co-occurrence of anxiety disorders with opiate dependence in order to better define the relationship between these two disorders and to improve diagnosis and treatment. The search used Medline and Toxibase up to January 1, 2009, and was based on a systematic review method. Eighteen studies were found. Prevalence of anxiety disorders assessed by Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria was high in opiate-dependent treated persons (lifetime prevalence ranged from 26% to 35%). Among anxiety disorders, phobic disorders have been shown to often precede the onset of opiate dependence. The identification of substance-induced versus independent anxiety disorder has important treatment implication. The monitoring of anxiety symptoms after several weeks of abstinence may allow physicians to determine the relationship between dependence and anxiety and make a reliable diagnosis of any initial anxious disorder. Specific management of anxiety disorder may then be used.
20. Randomized controlled trial of cognitive–behavioural therapy for coexisting depression and alcohol problems: short-term outcome_ Addiction 2010 105 (1): 87-997 9 Amanda L. Baker, David J. Kavanagh, Frances J. Kay-Lambkin, Sally A. Hunt, Terry J. Lewin, Vaughan J. Carr & Jennifer Connolly
22 KEYWORDS Alcohol dependence, CBT, co-morbidity, depression, integrated, treatment, RCT.
ABSTRACT Aims Alcohol use disorders and depression co-occur frequently and are associated with poorer outcomes than when either condition occurs alone. The present study (Depression and Alcohol Integrated and Single-focused Interventions; DAISI) aimed to compare the effectiveness of brief intervention, single-focused and integrated psychological interventions for treatment of coexisting depression and alcohol use problems. Methods Participants (n = 284) with current depressive symptoms and hazardous alcohol use were assessed and randomly allocated to one of four individually delivered interventions: (i) a brief intervention only (single 90-minute session) with an integrated focus on depression and alcohol, or followed by a further nine 1-hour sessions with (ii) an alcohol focus; (iii) a depression focus; or (iv) an integrated focus. Follow-up assessments occurred 18 weeks after baseline. Results Compared with the brief intervention, 10 sessions were associated with greater reductions in average drinks per week, average drinking days per week and maximum consumption on 1 day. No difference in duration of treatment was found for depression outcomes. Compared with single-focused interventions, integrated treatment was associated with a greater reduction in drinking days and level of depression. For men, the alcohol-focused rather than depression-focused intervention was associated with a greater reduction in average drinks per day and drinks per week and an increased level of general functioning. Women showed greater improvements on each of these variables when they received depression-focused rather than alcohol-focused treatment. Conclusions Integrated treatment may be superior to single-focused treatment for coexisting depression and alcohol problems, at least in the short term. Gender differences between single-focused depression and alcohol treatments warrant further study.
21. Childhood trauma and health outcomes in adults with comorbid substance abuse and mental health disorders Addictive Behaviours 2010 35 (1): 68-71 Nancy S. Wu, Laura C. Schairer, Elinam Dellor and Christine Grella
KEYWORDS: Adverse childhood events; Mental health; Substance abuse; Physical health problems
ABSTRACT This study describes the prevalence of childhood traumatic events (CTEs) among adults with comorbid substance use disorders (SUDs) and mental health problems (MHPs) and assesses the relation between cumulative CTEs and adult health outcomes. Adults with SUDs/MHPs (N = 402) were recruited from residential treatment programs and interviewed at treatment admission. Exposures to 9 types of adverse childhood experiences were summed and categorized into 6 ordinal levels of exposure. Descriptive analyses were conducted to assess the prevalence and range of exposure to CTEs in comparison with a sample from primary health care. Logistic regression analyses were conducted to examine the association between the cumulative exposure to CTEs and adverse health outcomes. Most of the sample reported exposure to CTEs, with higher exposure rates among the study sample compared with the primary health care sample. Greater exposure to CTEs significantly increased the odds of several adverse adult outcomes, including PTSD, alcohol dependence, injection drug use, tobacco use, sex work, medical problems, and poor quality of life. Study findings support the importance of early prevention and intervention and provision of trauma treatment for individuals with SUDs/MHPs.
22. The association between violence and lifetime suicidal thoughts and behaviors in individuals treated for substance use disorders Addictive Behaviours 2010 35 (2): 111-115 Mark A. Ilgen, Mandi L. Burnette, Kenneth R. Conner, Ewa Czyz, Regan Murray and Stephen Chermack
23 KEYWORDS: Suicide; Alcohol; Drugs; Violence; Addictions treatment
ABSTRACT Objective The present study examined the association between lifetime violent behavior and suicidal thoughts and attempts in a national sample of patients seeking substance use disorder (SUD) treatment. Method A large national sample of adults entering substance use disorder treatment (N = 6,233) was examined. After describing the correlates of prior suicidal thoughts and attempt(s) in this sample, we examined the association between self-report of lifetime violence and suicidal ideation, a single prior attempt and multiple prior attempts in patients seeking SUD treatment. Results In bivariate analyses, individuals with prior violence were more likely to report suicidal ideation, single and multiple suicide attempts than those without prior violence. These associations remained significant after controlling for demographic factors, symptoms of depression, and childhood victimization. In examinations of specific types of violence, more extreme forms of violence (i.e., murder, rape) were most strongly associated with risk of multiple suicide attempts. Conclusions Prior violence is consistently associated with greater risk for suicidal thoughts and behaviors in patients seeking SUD treatment. Treatment providers should be aware that those patients with some of the greatest violence in their past are also those at elevated risk for harm to themselves.
Drug related deaths
23. Interpretation of hair findings in children after methadone poisoning Forensic Science International 2010 196 (3): 51-54 Pascal Kintz, Julie Evans, Marion Villain and Vincent Cirimele
KEYWORDS: Hair; Contamination; Decontamination; Methadone; Child; Administration
ABSTRACT Methadone is not licensed for use in children though it can be employed for the management of neonatal opiate withdrawal syndrome. During the last 2 years, our laboratory has been asked to test for methadone and EDDP, its major metabolite, in hair from children that were admitted to hospital unconscious and where methadone had already been identified in a body fluid (4 cases) or where the children were deceased and evidence of methadone overdosage having already been established (2 cases). In all of these cases, segmental analysis revealed approximately the same amount of drug along the hair lock. As a consequence, contamination was considered as an issue and interpretation of the results was a challenge that deserves particular attention. After decontamination with dichloromethane and segmentation the hair was cut into small pieces, incubated overnight at 40 °C, liquid–liquid extracted and analysed with LC–MS/MS, using 2 transitions per compound. The LOQ for both methadone and EDDP was 10 pg/mg. In the first series involving children admitted to hospital, the following results were obtained: • case 1: 4 × 1 cm section, methadone at 0.05–0.08 ng/mg, no EDDP detected, • case 2: 4 × 1 cm section, methadone at 0.13–0.15 ng/mg, EDDP at 0.02 ng/mg, • case 3: 3 × 1.5 cm section, methadone at 0.07–0.09 ng/mg, EDDP at 0.01–0.03 ng/mg, • case 4: 6 × 2 cm section, methadone at 0.06–0.13 ng/mg, EDDP at 0.02–0.03 ng/mg. The following concentrations were obtained from the children who had died following a methadone overdose: • case 5: 2 × 2 cm section, methadone at 0.53–0.58 ng/mg, no EDDP detected, • case 6: 4 × 1 cm section, methadone at 0.44–0.77 ng/mg, EDDP at 0.04–0.06 ng/mg. The first observation is that all these concentrations are low by comparison with those observed in adults on methadone maintenance therapy. However, the more surprising observation is the relative homogenous concentrations along the hair locks in each specific case. This raises concerns around the possibility that contamination could have occurred prior to sampling and makes it hard to reach a conclusion regarding the possibility of repeated methadone exposure in the months prior the incidents.
24 In these cases it was impossible to conclude that the children were deliberately administered methadone. The results of the analysis of hair could indicate that they were in an environment where methadone was being used and where the drug was not being handled and stored with appropriate care. The homogenous concentrations found on segmental analyses could be indicative of external contamination that may have arisen not only from direct contamination with the drug but also via contamination with body fluids at the post mortem or from sweat produced close to the time of the incident. In view of these results we concluded that a single determination should not be used firmly to discriminate long-term exposure to a drug.
24. Non-fatal overdose in the 12 months following treatment for substance use disorders Drug and Alcohol Dependence 2010 107 (1): 51-55 Peter C. Britton , James D. Wines Jr and Kenneth R. Conner
KEYWORDS: Epidemiology; Overdose; Treatment; Risk factors; Sexual abuse; Intravenous drug abuse
ABSTRACT Background Overdose (OD) is a leading cause of mortality and morbidity for individuals with substance use disorders (SUDs), and there are limited prospective data on OD during the months following treatment for SUDs. Methods Variables associated with an OD in the 12 months after leaving an initial treatment episode were examined in an analysis of the Drug Abuse Treatment Outcomes Study (DATOS), a longitudinal naturalistic multisite study. Participants included 2966 patients with one or more SUDs. Non-fatal OD was ascertained by a positive response to “In the past 12 months, have you overdosed on drugs?” Multivariate logistic regression analyses were used to identify variables associated with OD. Results By 12 months, 93 (3.1%) participants reported one or more ODs. Variables associated with OD were lifetime history of OD, injection drug use (IDU), male sex, greater pain, and history of sexual abuse. Conclusions OD-risk appears to be increased by IDU, lifetime OD, sexual abuse history, and pain. The latter finding is novel for a prospective report and requires further study.
25. Over 1200 drugs-related deaths and 190,000 opiate-user-years of follow-up: Relative risks by sex and age group Addiction Research and Theory 2010 18 (2): 194–207 Sheila M Bird
KEYWORDS: Drugs-related deaths, heroin users, injectors, sex, age group, non-HIV mortality
ABSTRACT Heroin users/injectors’ risk of drugs-related death by sex and current age is weakly estimated both in individual cohorts of under 1000 clients, 5000 person-years or 50 drugs-related deaths and when using cross-sectional data. A workshop in Cambridge analysed six cohorts who were recruited according to a common European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) protocol from drug treatment agencies in Barcelona, Denmark, Dublin, Lisbon, Rome and Vienna in the 1990s; and, as external reference, opiate-user arrestees in France and Hepatitis C diagnosed ever-injectors in Scotland in 1993–2001, both followed by database linkage to December 2001. EMCDDA cohorts recorded approximately equal numbers of drugs-related deaths (864) and deaths from other non-HIV causes (865) during 106,152 person-years of follow-up. External cohorts contributed 376 drugs related deaths (Scotland 195, France 181) and 418 deaths from non-HIV causes (Scotland 221, France 197) during 86,417 person-years of follow-up (Scotland 22, 670, France 63, 747). EMCDDA
25 cohorts reported 707 drugs-related deaths in 81,367 man-years (8.7 per 1000 person years, 95% CI: 8.1–9.4) but only 157 in 24,785 person-years for females (6.3 per 1000 person-years, 95% CI: 5.4– 7.4). Except in external cohorts, relative risks by current age group were not particularly strong, and more modest in Poisson regression than in cross-sectional analyses: relative risk was 1.2 (95% CI: 1.0–1.4) for 35–44 year olds compared to 15–24 year olds, but 1.4 for males (95% CI: 1.2–1.6), and dramatically lower at 0.44 after the first year of follow-up (95% CI: 0.37–0.52).
26. Denial in alcohol and other drug use disorders: A critique of theory Addiction Research & Theory 2010 18 (2): 81-193 Patricia Ann Stoddard Dare, Leaanne Derigne
KEYWORDS: Denial, substance abuse, alcohol and other drug dependence, theory, addiction, stages of change
ABSTRACT Despite the centrality of the construct in the field of alcohol and other drug (AOD) addiction, denial remains poorly conceptualized. One reason for this narrow conceptualization is the recent unilateral devotion to the Transtheoretical Model (TTM). In an effort to demonstrate denial’s theoretical complexity, the TTM and five additional intuitively appealing theories of denial will be summarized. The strengths and weaknesses of each theory and possible treatment implications based on each theory will also be presented. The article concludes with a recommendation for future research to evaluate multiple theories of denial using consistent and rigorous research methodology in order to develop a comprehensive theory of denial. This will promote evolution of the deductive research process, and eventually lead to the development of empirically generated interventions which address the complex nature and etiology of denial.
27. An evaluation of a heroin overdose prevention and education campaign Drug and Alcohol Review 2010 29: 5–11 Danielle Horyniak, Peter Higgs, Jennifer Lewis, Rebecca Winter, Paul Dietze & Campbell Aitken
KEYWORDS: heroin overdose • health promotion • evaluation
ABSTRACT Introduction and Aims. Following detection of an upward trend in the frequency of fatal heroin overdoses in Victoria between 2001 and 2003, Victoria's Department of Human Services planned a campaign aimed at increasing injecting drug users' (IDU) awareness of overdose risks and prevention strategies. Stickers, wallet cards and posters featuring five key messages were distributed via needle and syringe programs (NSP) and other drug and alcohol services between November 2005 and April 2006. An evaluation of the campaign was commissioned to be conducted in late 2006. Design and Methods. The evaluation consisted of analysis of three independent data sets––quantitative data collected from IDU during the campaign period (n = 855 at baseline; and a range of 146–656 at follow up); qualitative interviews with IDU who were NSP clients during the campaign period (n = 16) and qualitative interviews with NSP staff and other key stakeholders (n = 9). Results. While key experts felt that the campaign messages had engendered lasting impact for at least some IDU, these positive impressions were not borne out by the NSP client data, with less than one quarter of all campaign messages being mentioned by a significantly higher proportion of clients during the post-campaign period compared with baseline. Key experts perceived the greatest weakness of the campaign to be the delay between issue identification and the introduction of campaign materials. Discussion and Conclusions. While IDU are generally responsive to health promotion campaigns, future initiatives in this domain should be designed and implemented rapidly and in ways that are sufficiently flexible to cope with shifts in drug markets which could influence the reception of key messages.[Horyniak D, Higgs P, Lewis J, Winter R, Dietze P, Aitken C. An evaluation of a heroin overdose prevention and education campaign. Drug Alcohol Rev 2009]
26 Effectiveness of treatment
28. Effect of co-occurring disorders and intimate partner violence on substance abuse treatment outcomes Journal of Substance Abuse Treatment 2010 38 (3): 231-244 Sherry Lipsky, Antoinette Krupski, Peter Roy-Byrne, Barbara Lucenko, David Mancuso and Alice Huber
KEYWORDS: Co-occurring disorders; Intimate partner violence; Substance use
ABSTRACT This retrospective cohort study examined risk factors for co-occurring substance use and mental disorders (COD) and the effect of COD and intimate partner violence (IPV) victimization among women and IPV-related arrest among men on 1-year substance abuse treatment outcomes. The study sample included clients admitted to Washington State publicly funded substance abuse treatment facilities in 2004–2007. COD was associated with a high substance use and IPV risk profile at admission. Having a COD decreased the odds of completing treatment by 30% among men and women and increased the risk of treatment reentry by 9% and 12% among men and women, respectively. IPV also decreased the odds of completing treatment among women and increased the risk of treatment reentry among men. Men with COD were less likely than those without COD to be arrested for substance-related crimes but more likely to be arrested for violence-related crimes in the follow-up period. Implications of these findings are discussed.
Epidemiology and Demography
29. Healthcare and Medical Graduates of 2009: Their Reactions to Four Key Proposals in the Scottish Government’s Strategy for Tackling Alcohol Misuse Alcohol Alcohol 2010 45: 200-206 Jan S. Gill, Caroline Gibson, and Maggie Nicol
ABSTRACT Aims: This study compares the views of final year medical, and nursing and allied health professional (NAHP) students in relation to four governmental proposals impacting on the sale and purchase of alcohol. Methods: Against a background of political will to address alcohol abuse in Scotland and moves within the National Health Service promoting a shifting of professional roles, self-completed questionnaires were administered in spring 2009 through course websites and lectures to final year medical and NAHP students. Results: Questionnaires were returned by 406 NAHPs and 121 medical students. Over three quarters of all students agreed with the proposed change to reduce the drink driving limit to 50 mg/100 ml blood. Less support was evident for the raising of the minimum legal purchase age for off-sales (37%), the banning of below cost price promotions of alcohol (47%) and minimum retail pricing (37%). However, there were differences between the NAHP and medical students in the case of the final two proposals; over 60% of the medical students agreed they would have a positive impact. For NAHPs, figures were 41% and 31%, respectively. Conclusions: Support for four key proposals outlined by the Scottish Government to address alcohol misuse varied. Only the suggestion to lower the drink driving limit received backing overall and within students in these professions. Effectiveness of proposed restrictions on the price of alcohol was less well regarded except by medical students. Evident gaps in knowledge around health guidelines, and the finding that almost half of NAHPs disagreed that they had the appropriate knowledge to advise patients about responsible drinking advice and alcohol misuse problems, suggest a need for improved undergraduate education and continued professional development with respect to public health aspects of alcohol use.
27 30. Gender-related differences in the pharmacokinetics of opiates Forensic Science International 2010 194 (1-3): 28-33 Maja Djurendic-Brenesel, Neda Mimica-Dukic, Vladimir Pilija and Milos Tasic
KEYWORDS: Gender differences; Opiates; Pharmacokinetics; GC–MS; Basal ganglia
ABSTRACT Previous studies have documented gender-related differences in a number of aspects of the pharmacology of opiates, including their analgesic activity, stimulative properties and generation of physical dependence. The current experiments were carried out with the aim to examine whether male–female differences exist in the blood and brain levels of opiates attained after their intraperitoneal injection to male and female Wistar rats. The tests were performed 5, 15, 45 and 120 min after the animal treatment with seized heroin. Gas chromatography–mass spectrometry (GC– MS) method was developed to quantitatively determine opiate alkaloids in blood and brain regions (known for their high concentration of μ-opiate receptors): cortex, brainstem, amygdala and basal ganglia. Maximal contents of opiates in blood of animals of both genders were found in the second measurement time (15 min), the values measured in the males being significantly higher, which suggests a faster passage of the opiates from blood to brain tissue in female animals. The highest content of opiates in the brain tissue of female animals was measured 15 min and with male animals 45 min after the treatment, which also indicates faster distribution of opiates from blood to brain in the female compared to male rats. The highest proportion of opiates was found in the basal ganglia of the animals of both genders. The obtained results offer the possibility of selecting this part of the brain tissue of both males and females as a representative sample for identifying and assessing contents of opiates.
31. Patterns of illegal drug use among an adult alcohol dependent population: Results from the National Survey on Drug Use and Health Drug and Alcohol Dependence 2010 106 (2-3): 119-125 S.L. Hedden, S.S. Martins, R.J. Malcolm, L. Floyd, C.E. Cavanaugh nd W.W. Latimer
KEYWORDS: Comorbidity; Latent class analysis; Epidemiology; Sexually transmitted disease; Risk factors
ABSTRACT The use of illegal drugs is common in alcohol dependence and significant psychological and social consequences are associated with the concurrent use of alcohol and illegal drugs. However, little literature has examined the patterns of concurrent-drug use in alcohol dependent individuals. A latent class analysis (LCA) was used to determine whether patterns of past year illegal drug use existed in a national sample of 6059 alcohol dependent respondents of the combined 2005, 2006 and 2007 National Survey on Drug Use and Health. Multinomial logistic regression was then used to determine whether demographic variables, mental health disturbance and social consequences were predictive of drug use classes. Results of the LCA demonstrated a 5-class solution with optimal fit deduced by Bayesian Information Criterion minima. The five classes included: a close to zero probability of illegal drug use (class 1: 65%), medium marijuana, medium sedatives/tranquilizers and high analgesics (class 2: 7%), high marijuana, medium cocaine use (class 3: 21%), high probabilities of marijuana, cocaine, sedatives and analgesic use (class 4: 6%) and a high concurrent-drug use except other hallucinogens (class 5: 1%). Regression results suggest that younger age, comorbidity, engaging in deviant behaviors, sexually transmitted infection and incarceration are associated with concurrent illegal drug use in alcohol dependent individuals. Findings advocate that more intense psychiatric and drug dependence treatment resources may be needed for concurrent-drug using alcohol dependent populations and provide evidence for targeted prevention and treatment interventions.
28 32. The nature and extent of illegal drug and alcohol-related litter in Scottish social housing community: A photographic investigation Addiction Research and Theory 2010 18 (1): 71–83 Alasdair J. M. Forsyth And Neil Davidson
KEYWORDS: Drug-litter, needle-stick, off-trade, glass, community safety, advertising
ABSTRACT This article investigates the nature and extent of alcohol and other drug-related litter in a residential community. This was done by means of a survey of such litter conducted in the social housing ‘schemes’ of a Scottish town, piloting the use of interpretive photography to assess the threat that these pose in the community (n¼1239 pictures of such items). The survey found little evidence of hazardous illegal drug-related litter (number of sets of needles/syringes) in comparison to alcohol litter such as broken bottles. The photographs taken also illustrated the ways in which the risks posed by such litter could vary, according to the type of items concerned (e.g. plastic vs. glass, especially screwcap, bottles) and their locations. It is also suggested that brand identifiable alcohol litter may act as form of free advertising. These findings are discussed in terms of community safety, and the need to raise awareness of the issues surrounding alcohol-related glass in a community setting as has already been done with illegal drug litter. It is also recommended that certain off-trade alcohol distributers switch from glass to plastic bottles.
33. Substance use among late adolescent urban youths: Mental health and gender influences Addictive Behaviours 2010 35 (1): 30-34 Traci M. Schwinn, Steven P. Schinke and Danielle N. Trent
KEYWORDS: Adolescent; Drug use; Gender; Mental health; Urban; Moderate
ABSTRACT This paper explores gender and mental health influences on alcohol, tobacco, and illicit drug use among late adolescent urban youths. Specifically, we examine whether rates of substance use differ by gender, whether mental health indices differ by gender and are predictive of substance use, and whether gender moderates the relationship between mental health and substance use. Data from our non-clinical sample of 400 youths were collected primarily online. Analysis of cross-sectional data revealed no differences in substance use by gender. Indices of mental health differed by gender, with girls reporting greater symptoms of depression and anxiety. Ratings of hostility were similar for boys and girls. Alcohol, tobacco, and drug use were associated with greater symptoms of depression, anxiety, and hostility; this relationship, however, was not moderated by gender. Study findings provide evidence that among late adolescent youths living in urban areas, poorer mental health status is associated with increased substance use. Evidence of a moderating effect of gender on the relationship between mental health and substance use was not significant.
34. Comorbidity of generalized anxiety disorder and alcohol use disorders among individuals seeking outpatient substance abuse treatment Addictive Behaviours 2010 35 (1): 42-45 Joshua P. Smith and Sarah W. Book
KEYWORDS: Generalized anxiety disorder; Alcohol use disorders; Comorbidity; Worry; Outpatient substance abuse treatment
ABSTRACT The present study sought to address a gap in the literature by providing preliminary evidence of the prevalence and clinical characteristics of comorbid generalized anxiety disorder (GAD) and alcohol use disorders (AUD) in a front-line outpatient substance abuse clinic. Of 39 outpatients meeting criteria for an AUD, nearly half (46%) also met criteria for current GAD. The onset of GAD occurred prior to
29 AUD in 67% of comorbid cases, with an average time lag of 12.5 years among individuals with primary GAD. Participants with comorbid GAD–AUD endorsed higher levels of worry severity and worry- reduction alcohol expectancies, and 55.6% of comorbid participants had a history of suicide attempts. Groups did not differ on anxiety sensitivity, social anxiety, or depression. Comorbid participants were more likely to indicate that worry interfered with their substance abuse treatment, and to indicate interest in concurrent treatment targeting their worry. Study findings provide initial evidence that GAD may be a prevalent and relevant factor among individuals with AUD seeking outpatient substance abuse treatment.
35. Mortality and cause of death among 1705 illicit drug users: A 37 year follow up Drug and Alcohol Review 2010 29 (1): 21-27 Marlene Stenbacka, Anders Leifman, Anders Romelsjö
KEYWORDS alcohol • drug abuse • epidemiology • mortality
ABSTRACT Introduction and Aims. To examine the overall mortality and causes of deaths of a large cohort of users of illicit drugs in Stockholm over 37 years. Design and Methods. People with substance abuse were identified through records collected by different institutions in Stockholm in 1967. Subjects were followed in registers recording mortality and cause of death and in-patient care stays until 2003. Results. More than half (n = 860) of the 1705 identified substance abusers died at an average age of 47 years, 25–30 years younger than the general population. The standardised rate ratio (SRR) for mortality was 3.3 among men and 3.5 among women. Incidence of mortality per 1000 person-years was also increased, but somewhat lower for women. The difference between these two measures is mainly explained by a lower mortality among women in general. In-patient care stays with both alcohol and drug-related diagnoses were associated with higher risk of dying among women than men: SRR = 14.5 and SRR = 4.0, respectively. Accidents and suicide were the most common cause of death among the youngest subjects (15–24 years) and cardiovascular diseases and tumours among the oldest (≥55 years). Discussion and Conclusions. Accidents and suicide, especially at a young age, are two common causes of death that might be prevented by increased awareness in medical personnel, along with better treatment and supportive measures.[Stenbacka M, Leifman A, Romelsjö A. Mortality and cause of death among 1705 illicit drug users: A 37 year follow up. Drug Alcohol Rev 2009]
36. Impact of Self-Reported Life Events on the Profile of Opioid Dependence Syndrome The American Journal of Drug and Alcohol Abuse 2010 36: 7–12 Hamdy F. Moselhy, Ehsan Fahmy, Victor Samy Mikhael, and Hussein El-Sheikh
ABSTRACT Aim: The aim of this work was to investigate the impact of life events on the profile of opioid dependent patients. Method: Recruitment was achieved through outpatient drug treatment clinic in Birmingham, UK, and data were collected through semistructured interviews. One-hundred and twenty subjects with opioid dependence syndrome were interviewed, and 100 controls of non-drug- using family members and friends. Result: The mean age of the opioid group was 33.3 years, SD = 8.8. The majority individuals of the sample were White British (80.8%), unemployed (69.2%), and male (75%). The mean severity of dependence as measured by two scales indicated severe level of dependence according to the authors of each scale. The mean number of traumatic events for the opioid dependence group was 4.8, SD = 3.57 vs. 3.55; SD = 3.65 in control group with significant difference (t = 2.56, df = 218, p = .01). Significant predictors of severe opioid dependency were age of second exposure to events, change of residence, break-up with boy/girlfriend, and conflict with father. Conclusion: The data presented indicate that a significant group of opioid dependent patients
30 experience adverse life events in both childhood and adulthood. It is by attending to and addressing these issues that health care workers can alleviate ongoing distress and promote confidence.
37. Opiate and crack cocaine use: A new understanding of prevalence Drugs: education, prevention and policy 201017 (2): 135–147 Gordon Hay, Maria Gannon, Jane Macdougall, Catherine Eastwood, Kate Williams and Tim Millar
ABSTRACT Aims: The aim of this study was to establish prevalence estimates of problem drug use, defined as opiate and/or crack cocaine use by persons aged 15 to 64 years, for England and for each of the 149 administrative areas responsible for commissioning drug interventions. Methods: Indirect estimation techniques, the capture–recapture and multiple indicator methods, were used to obtain estimates. Information on problem drug users presenting to healthcare settings and/or recorded by the criminal justice system, and drug-related indicator data were used in the analyses. Findings: There were an estimated 332,090 problem drug users in England during 2005/06 (95% CI 324,546 to 346,345), equivalent to 9.97 (95% CI 9.74 to 10.40) problem drug users per thousand population aged 15 to 64 years. Prevalence varied by geographic region and age group: the highest rates were observed in London and for those aged 25 to 34 years. Conclusions: This study has produced estimates of the prevalence of problem drug use in England that are more robust, more precise, and suggest a higher prevalence than previous studies. The estimates provide a basis on which to formulate policy, plan services, and measure service performance.
38. Linkage Analysis of Alcohol Dependence Symptoms in the Community Clinical and Experimental Research 2010 34 (1): 158-163 Narelle K. Hansell, Arpana Agrawal, John B. Whitfield, Katherine I. Morley, Scott D. Gordon, Penelope A. Lind, Michele L. Pergadia, Grant W. Montgomery, Pamela A. F. Madden, Richard D. Todd, Andrew C. Heath, Nicholas G. Martin
KEYWORDS Alcohol Dependence Symptoms • Genetic Linkage Analysis • Community Sample
ABSTRACT Background: We have previously identified suggestive linkage for alcohol consumption in a community-based sample of Australian adults. In this companion paper, we explore the strength of genetic linkage signals for alcohol dependence symptoms. Methods: An alcohol dependence symptom score, based on DSM-IIIR and DSM-IV criteria, was examined. Twins and their nontwin siblings (1,654 males, 2,518 females), aged 21 to 81 years, were interviewed, with 803 individuals interviewed on 2 occasions, approximately 10 years apart. Linkage analyses were conducted on datasets compiled to maximize data collected at either the younger or the older age. In addition, linkage was compared between full samples and truncated samples that excluded the lightest drinkers (approximately 10% of the sample). Results: Suggestive peaks on chromosome 5p (LODs >2.2) were found in a region previously identified in alcohol linkage studies using clinical populations. Linkage signal strength was found to vary between full and truncated samples and when samples differed only on the collection age for a sample subset. Conclusions: The results support the finding that large community samples can be informative in the study of alcohol-related traits.
31 Harm Reduction
39. Route transition interventions: Potential public health gains from reducing or preventing injecting International Journal of Drug Policy 2010 21 (2): 125-128 Jamie Bridge
KEYWORDS: Illicit Drugs; Injecting; Chasing; NIROA; Route transitions
ABSTRACT Multiple factors are implicated in the diffusion of injecting drug use (IDU), including individual and demographic characteristics, drug markets, economics, social networks and political and cultural environments. However, studies show that individual transitions away from injecting are possible, and that a recent diffusion of non-injecting routes of administration (NIROA) has occurred in several countries. Injecting is more risk-laden than other routes of drug administration, yet relatively little attention has been paid to reducing or preventing injecting drug use by promoting NIROA. This commentary reviews the case for, and examples of, ‘route transition interventions’ which seek to do this. These include: prescribing oral substitutes; providing non-injecting equipment; providing safer smoking facilities; and training individuals to prevent transitions to injecting, promote NIROA, or prevent the initiation of new injectors. These initiatives have the potential—as yet largely unrealised— to offer public health gains and empower people to control and manage their drug use. Further research is needed to secure commitments at all levels to support this approach.
40. Normalization and harm reduction: Research avenues and policy agendas International Journal of Drug Policy 2010 21 (2): 137-139 Patricia G. Erickson and Andrew D. Hathaway
KEYWORDS: Normalization; Harm reduction; Cannabis; Drug policy
ABSTRACT An affinity between the evidence and arguments for drug normalization and the policy and programme directions favoured by harm reduction is often assumed but seldom critically examined. This commentary looks at parallels and contradictions emerging with respect to different cultures, social settings, types of problems and responses where the match is less than perfect. Mounting evidence of normalization has also led to backlash in some countries and the mobilization of forces reaffirming prohibition. We call for further research on normalization that focuses on substance use, risks, harms, and social context across a broader spectrum of the population, and in a variety of cultures. By emphasizing the most serious harms experienced by persons in the smallest segments of drug using populations, harm reduction often has neglected broader research and policy suggestions that might be implemented to benefit controlled, recreational drug users. Future policy development with respect to normalization will require more research and more serious discussion of its implications for informing the transition toward a global public health approach to substance use.
41. ‘Does anyone know where to get fits from around here?’ Policy implications for the provision of sterile injecting equipment through pharmacies in Sydney, Australia Drugs: Education, Prevention, and Policy 2010 17(1): 72-83 Carla Treloar, Max Hopwood, Joanne Bryant
ABSTRACT Background: Little is known about the factors that influence injecting drug users’ (IDUs) choice of outlet, and in particular why some IDUs might prefer to use pharmacies. Greater understanding of the influences on this choice will contribute to more sophisticated policy and programme responses for blood-borne virus prevention and for health and wellbeing programmes for people who inject drugs.
32 Method: In-depth interviews were conducted with 15 IDUs about their experiences of accessing injecting equipment from pharmacies that participated in the government-sponsored pharmacy needle and syringe scheme. Results: A range of factors influenced participants’ decisions about equipment access. The advantages of the pharmacy scheme access included convenience, relative anonymity, increased positive feelings of self-worth when accessing equipment from pharmacies where they had a good relationship with staff, less police surveillance and access to a greater range of equipment than available in publicly funded Needle and Syringe Programmes. The disadvantages of pharmacy access included the cost of equipment and complications related to methadone dosing and equipment access. Conclusion: Pharmacy access to injecting equipment is highly valued by IDUs. The results of this study direct attention to several elements of programme and policy in the area that would increase access to equipment from pharmacies relating to cost, need for exchange, police surveillance practices, out-of-hours access and anonymity.
42. The impact of a supervised injecting facility on ambulance call-outs in Sydney, Australia Addiction 2010 105 (4): 676-683 Allison M. Salmon, Ingrid van Beek, Janaki Amin, John Kaldor and Lisa Maher
KEYWORDS Ambulance attendance • drug consumption rooms • injecting drug use • MSIC • opioid-related overdose • overdose management • supervised injecting facilities
ABSTRACT Aims Supervised injecting facilities (SIFs) are effective in reducing the harms associated with injecting drug use among their clientele, but do SIFs ease the burden on ambulance services of attending to overdoses in the community? This study addresses this question, which is yet to be answered, in the growing body of international evidence supporting SIFs efficacy. Design Ecological study of patterns in ambulance attendances at opioid-related overdoses, before and after the opening of a SIF in Sydney, Australia. Setting A SIF opened as a pilot in Sydney's 'red light' district with the aim of accommodating a high throughput of injecting drug users (IDUs) for supervised injecting episodes, recovery and the management of overdoses. Measurements A total of 20 409 ambulance attendances at opioid-related overdoses before and after the opening of the Sydney SIF. Average monthly ambulance attendances at suspected opioid- related overdoses, before (36 months) and after (60 months) the opening of the Sydney Medically Supervised Injecting Centre (MSIC), in the vicinity of the centre and in the rest of New South Wales (NSW). Results The burden on ambulance services of attending to opioid-related overdoses declined significantly in the vicinity of the Sydney SIF after it opened, compared to the rest of NSW. This effect was greatest during operating hours and in the immediate MSIC area, suggesting that SIFs may be most effective in reducing the impact of opioid-related overdose in their immediate vicinity. Conclusions By providing environments in which IDUs receive supervised injection and overdose management and education SIF can reduce the demand for ambulance services, thereby freeing them to attend other medical emergencies within the community.
43. Syringe exchange, injecting and intranasal drug use Addiction 2010 105 (1): 155-158754747 155.158 Don C. Des Jarlais, Kamyar Arasteh, Courtney McKnight, Martin Ringer & Samuel R. Friedman
KEYWORDS Injecting drug use, intranasal drug use, syringe exchange.
ABSTRACT Objective To assess trends in injecting and non-injecting drug use after implementation of large-scale syringe exchange in New York City. The belief that implementation of syringe exchange will lead to
33 increased drug injecting has been a persistent argument against syringe exchange. Methods Administrative data on route of administration for primary drug of abuse among patients entering the Beth Israel methadone maintenance program from 1995 to 2007. Approximately 2000 patients enter the program each year. Results During and after the period of large-scale implementation of syringe exchange, the numbers of methadone program entrants reporting injecting drug use decreased while the numbers of entrants reporting intranasal drug use increased (P < 0.001). Conclusion While assessing the possible effects of syringe exchange on trends in injecting drug use is inherently difficult, these may be the strongest data collected to date showing a lack of increase in drug injecting following implementation of syringe exchange.
Homelessness
44. Biological markers of problem drinking in homeless patients Addictive Behaviours 35 (3): 260-262 Henrik Thiesen and Morten Hesse
KEYWORDS: Alcohol; Carbohydrate-deficient transferrin; Gamma-glutamyl transferrase; Misclassification; Diagnostic efficiency
ABSTRACT Objective In the search for optimal biomarkers of excessive drinking, a central limitation has been the lack of sensitivity of measures. Many patients have apparently normal values of liver markers despite a considerable alcohol intake. This study aimed to test a novel combined indicator of alcohol drinking. Material and methods Concentrations of carbohydrate-deficient transferrin (%CDT), γ glutamyl transferase (γGT), aspartate aminotransferase (ASAT), and mean corpuscular volume (MCV), together with a combined index of the %CDT and γGT, the Antilla Index (AI), were studied in 104 homeless patients with (n = 87) or without (n = 24) problem drinking according to the Fast Alcohol Screening Test. Results Concentrations of all markers were significantly higher in the alcoholic patients than in other homeless patients. The best agreement between liver markers and self-reported status was found between the combined %CDT and γGT index (kappa = 0.61, p < 0.001, sensitivity = 63%, specificity = 94%). Conclusions The combined AI is a relatively efficient measure of current drinking in homeless populations.
Injecting Behaviour
45. Impact of injecting drug use on mortality in Danish HIV-infected patients: a nation-wide population-based cohort study Addiction 2010 105 (3): 529-535 Mette V. Larsen, Lars H. Omland, Jan Gerstoft, Carsten S. Larsen, Janne Jensen, Niels Obel and Gitte Kronborg
KEYWORDS Cohort studies • HIV • HIV infection • injecting drug use • intravenous • mortality • substance abuse • survival • survival rate
ABSTRACT Objectives To estimate the impact of injecting drug use (IDU) on mortality in HIV-infected patients in the highly active antiretroviral therapy (HAART) era. Design Population-based, nation-wide prospective cohort study in Denmark (the Danish HIV Cohort Study).
34 Methods A total of 4578 HIV-infected patients were followed from 1 January 1997 or date of HIV diagnosis. We calculated mortality rates stratified on IDU. One-, 5- and 10-year survival probabilities were estimated by Kaplan–Meier methods, and Cox regression analyses were used to estimate mortality rate ratios (MRR). Results Of the patients, 484 (10.6%) were categorized as IDUs and 4094 (89.4%) as non-IDUs. IDUs were more likely to be women, Caucasian, hepatitis C virus (HCV) co-infected and younger at baseline; 753 patients died during observation (206 IDUs and 547 non-IDUs). The estimated 10-year survival probabilities were 53.2% [95% confidence interval (CI): 48.1–58.3] in the IDU group and 82.1% (95% CI: 80.7–83.6) in the non-IDU group. IDU as route of HIV infection more than tripled the mortality in HIV-infected patients (MRR: 3.2; 95% CI: 2.7–3.8). Adjusting for potential confounders did not change this estimate substantially. The risk of HIV-related death was not increased in IDUs compared to non-IDUs (MRR 1.1; 95% CI 0.7–1.7). Conclusions Although Denmark's health care system is tax paid and antiretroviral therapy is provided free of charge, HIV-infected IDUs still suffer from substantially increased mortality in the HAART era. The increased risk of death seems to be non-HIV-related and is due probably to the well- known risk factors associated with intravenous drug abuse.
Miscellaneous
46. Tobacco, cocaine, and heroin: Craving and use during daily life Addictive Behaviours 2010 35 (4): 318-324 David H. Epstein, Gina F. Marrone, Stephen J. Heishman, John Schmittner and Kenzie L. Preston
KEYWORDS: Smoking; Nicotine; Cocaine; Heroin; Ecological momentary assessment; Craving
ABSTRACT Background Relationships among tobacco smoking, tobacco craving, and other drug use and craving may have treatment implications in polydrug-dependent individuals. Methods We conducted the first ecological momentary assessment (EMA) study to investigate how smoking is related to other drug use and craving during daily life. For up to 20 weeks, 106 methadone-maintained outpatients carried PalmPilots (PDAs). They reported their craving, mood, behaviors, environment, and cigarette-smoking status in 2 to 5 random-prompt entries/day and initiated PDA entries when they used cocaine or heroin or had a discrete episode of craving for cocaine or heroin. Results Smoking frequency increased linearly with random-prompt ratings of tobacco craving, cocaine craving, and craving for both cocaine and heroin. Smoking frequency was greater during discrete episodes of cocaine use and craving than during random-prompt reports of low craving for cocaine. This pattern was also significant for dual cocaine and heroin use and craving. Smoking and tobacco craving were each considerably reduced during periods of urine-verified abstinence from cocaine, and there was a (nonsignificant) tendency for morning smoking to be especially reduced during those periods. Conclusions This EMA study confirms that smoking and tobacco craving are strongly associated with the use of and craving for cocaine and heroin. Together with prior findings, our data suggest that tobacco and cocaine may each increase craving for (and likelihood of continued use of) themselves and each other. Treatment for tobacco dependence should probably be offered concurrently with (rather than only after) initiation of treatment for other substance-use disorders.
47. The abuse potential of the synthetic cannabinoid nabilone Addiction 2010 105 (3): 494-503 Mark A. Ware and Emmanuelle St Arnaud-Trempe
35 KEYWORDS Abuse • Canada • cannabinoid • nabilone • pain • survey
ABSTRACT Aim Nabilone is a synthetic cannabinoid prescription drug approved in Canada since 1981 to treat chemotherapy-induced nausea and vomiting. In recent years, off-label use of nabilone for chronic pain management has increased, and physicians have begun to express concerns about nabilone becoming a drug of abuse. This study evaluates the evidence for abuse of nabilone, which is currently ill-defined. Study design Scientific literature, popular press and internet databases were searched extensively for evidence of nabilone abuse. Focused interviews with medical professionals and law enforcement agencies across Canada were also conducted. Findings The scientific literature and popular press reviews found very little reference to nabilone abuse. Nabilone is perceived to produce more undesirable side effects, to have a longer onset of action and to be more expensive than smoked cannabis. The internet review revealed rare and isolated instances of recreational use of nabilone. The database review yielded little evidence of nabilone abuse, although nabilone seizures and thefts have occurred in Canada in the past few years, especially in Ontario. Most law enforcement officers reported no instances of nabilone abuse or diversion, and the drug has no known street value. Medical professionals reported that nabilone is not perceived to be a matter of concern with respect to its abuse potential. Conclusions Reports of nabilone abuse are extremely rare. However, follow-up of patients using nabilone for therapeutic purposes is prudent and should include assessment of tolerance and dependence. Prospective studies are also needed to definitively address the issue of nabilone abuse.
48. The 10 most important things known about addictionadd_2 Addiction 2010 105(1): 6-13 Doug Sellman
KEYWORDS: Addiction, comorbidity, compulsion, entheogens, knowledge, lifestyle change, motivational interviewing.
ABSTRACT If you were asked: ‘What are the most important things we know about addiction?’ what would you say? This paper brings together a body of knowledge across multiple domains and arranged as a list of 10 things known about addiction, as a response to such a question. The 10 things are: (1) addiction is fundamentally about compulsive behaviour; (2) compulsive drug seeking is initiated outside of consciousness; (3) addiction is about 50% heritable and complexity abounds; (4) most people with addictions who present for help have other psychiatric problems as well; (5) addiction is a chronic relapsing disorder in the majority of people who present for help; (6) different psychotherapies appear to produce similar treatment outcomes; (7) ‘come back when you’re motivated’ is no longer an acceptable therapeutic response; (8) the more individualized and broad-based the treatment a person with addiction receives, the better the outcome; (9) epiphanies are hard to manufacture; and (10) change takes time. The paper concludes with a call for unity between warring factions in the field to use the knowledge already known more effectively for the betterment of tangata whaiora (patients) suffering from addictive disorders.
49. Guilty until proven innocent: A qualitative study of the management of chronic non-cancer pain among patients with a history of substance abuse Addictive Behaviours 35 (3): 270-272 Alex Baldacchino, Gail Gilchrist, Rod Fleming and Jonathan Bannister
KEYWORDS: Chronic non cancer pain; Opioid prescribing; Substance abuse; Attitudes; Qualitative research
36 ABSTRACT Introduction Physicians are often reluctant to prescribe strong opioids for chronic non cancer pain (CNCP). No study has qualitatively examined physicians' beliefs about prescribing opioids for CNCP to patients with a history of substance abuse (PWHSA). Aims To describe physicians' attitudes and experience of prescribing opioids for CNCP to PWHSA. Design, setting and participants Nineteen individual interviews and two focus groups were conducted with GPs, Addiction Specialists, Pain Specialists and Rheumatologists. Results Physicians were “reluctant” to prescribe opioids to PWHSA experiencing CNCP for fear of addiction, misuse or diversion of medications. Many exhibited “distrust” that such patients were experiencing “genuine pain”, resulting in patients often being considered guilty until proven innocent. Such negative regard towards these patients was based on previous manipulative “drug seeking” encounters and often resulted in the under treatment of pain. Potential “flags” were identified that alerted physicians to the potential for abuse or diversion of their prescription including: doctor shopping, loosing prescriptions, frequent attendance and early requests for repeat prescriptions. Physicians reported different management approaches and stricter prescribing regimes for PWHSA to limit the potential of addiction, misuse and diversion. Examples of poor pain management were described where drug users had been under treated as a result of negative attitudes or inexperience of staff. Discussion Applying the chronic disease model to comorbid addiction and CNCP would ensure a health and social care system that makes it difficult to stigmatise patients experiencing these conditions and would facilitate the prescribing of opioid pain medication to patients who could benefit.
Opiate Treatment
50. Preference for buprenorphine/naloxone and buprenorphine among patients receiving buprenorphine maintenance therapy in France: A prospective, multicenter study Journal of Substance Abuse Treatment 2010 38 (1): 83-89 Jean-Pierre Daulouède, Yves Caer, Pascal Galland, Pierre Villeger, Emmanuel Brunelle, Jérôme Bachellier, Jean-Michel Piquet, Jean Harbonnier, Yves Leglise and Pascal Courty
KEYWORDS: Buprenorphine; Heroin; Misuse; Naloxone; Opioids
ABSTRACTMaintenance treatment with buprenorphine tablets (Subutex) has been associated with reductions in heroin use; however, concerns for intravenous misuse exist. A buprenorphine/naloxone formulation (Suboxone) was designed to reduce this misuse risk while retaining buprenorphine's efficacy and safety. This prospective, open-label, multicenter trial compared preferences for buprenorphine and buprenorphine/naloxone in 53 opioid-dependent patients stabilized on buprenorphine. Buprenorphine was first administered at the patient's current dose (Days 1–2), followed by a direct switch to buprenorphine/naloxone (Days 3–5). Global satisfaction rates were high and similar between buprenorphine and buprenorphine/naloxone; however, patients preferred the tablet taste, size, and sublingual dissolution time of buprenorphine/naloxone. At the end of the study, 54% of patients preferred buprenorphine/naloxone, 31% preferred buprenorphine, and 15% had no preference; most patients (71%) wished to continue treatment with buprenorphine/naloxone. This study did not identify any impediments to a direct buprenorphine-to-buprenorphine/naloxone switch and revealed some characteristics that may facilitate treatment with buprenorphine/naloxone.
51. A heroin prescription trial: Case studies from Montreal and Vancouver on crime and disorder in the surrounding neighbourhoods International Journal of Drug Policy 2010 21: 28–35
37 Benoit Lasniera, Serge Brochub, Neil Boyd and Benedikt Fischerd
KEYWORDS: Medical heroin prescription; Heroin users; Crime; Disorder
ABSTRACT BackgroundThis study evaluates whether the instauration of a heroin prescription trial (‘NAOMI’) generated an impact on the occurrence of crime and disorder in surrounding areas. The clinical trial was initiated in Vancouver and Montreal in 2005, with the aim of assessing the benefits of heroin- assisted treatment (HAT) in Canada. While experiences from other jurisdictions where HAT trials have been implemented clearly demonstrate substantial crime reduction effects for trial participants, there is overall concern that HAT clinics – similar to other interventions aiming at problematic street drug users – may induce a ‘honeypot’ effect, leading to increases in crime and/or disorder problems in the vicinity of interventions. It has been argued that HAT clinics will attract undesirable behaviour associated with cultures of street drug use and thereby produce negative impacts on the community. Methods This study examined the incidence of crime and disorder in the Vancouver and Montreal sites before and during the NAOMI trial (2002–2006), using police calls for service and arrest data. Data were analysed by autoregression analyses. Results The analysis suggested that most indicators remained stable during the pre- and implementation phase of the NAOMI trial in both sites. Conclusion While the attribution of observed crime and disorder trends to the specific clinical interventions in Montreal and Vancouver is difficult and many extrinsic factors may play a role, this study has not generated any clear evidence from institutional police data to suggest increases or decreases in community-based problems associated with HAT programs in Canada.
52. Why don’t out-of-treatment individuals enter methadone treatment programmes? International Journal of Drug Policy 2010 21: 36–42 James A. Peterson∗, Robert P. Schwartz, Shannon Gwin Mitchell, Heather Schacht Reisinger, Sharon M. Kelly, Kevin E. O’Grady, Barry S. Brown, Michael H. Agar
KEYWORDS: Heroin addicts; Methadone treatment; Out-of-treatment
ABSTRACT Background Despite the proven effectiveness of methadone treatment, the majority of heroin-dependent individuals are out-of-treatment. Methods Twenty-six opioid-dependent adults who met the criteria for methadone maintenance who were neither seeking methadone treatment at the time of study enrollment, nor had participated in such treatment during the past 12 months, were recruited from the streets of Baltimore, Maryland through targeted sampling. Ethnographic interviews were conducted to ascertain participants’ attitudes toward methadone treatment and their reasons for not seeking treatment. Results Barriers to treatment entry included: waiting lists, lack of money or health insurance, and requirements to possess a photo identification card. For some participants, beliefs about methadone such as real or rumored side effects, fear of withdrawal from methadone during an incarceration, or disinterest in adhering to the structure of treatment programmes kept them from applying. In addition, other participants were not willing to commit to indefinite “maintenance” but would have accepted shorter time-limited methadone treatment. Conclusion Barriers to treatment entry could be overcome by an infusion of public financial support to expand treatment access, which would reduce or eliminate waiting lists, waive treatment-related fees, and/or provide health insurance coverage for treatment. Treatment programmes could overcome some of the barriers by waiving their photo I.D. requirements, permitting time-limited treatment with the option to
38 extend such treatment upon request, and working with corrections agencies to ensure continued methadone treatment upon incarceration.
53. A cost-benefit and cost-effectiveness analysis of Vancouver’s supervised injection facility International Journal of Drug Policy 2010 21: 70–76 Martin A. Andresen, Neil Boyd
KEYWORDS: Supervised injection facility; Insite; Cost-benefit analysis
ABSTRACT Background A supervised injection facility (SIF) has been established in North America: Insite, in Vancouver, British Columbia. The purpose of this paper is to conduct a cost-effectiveness and cost-benefit analysis of this SIF using secondary data gathered and analysed in 2008. In using these data we seek to determine whether the facility's prevention of infections and deaths among injecting drug users (IDUs) is of greater or lesser economic cost than the cost involved in providing this service – Insite – to this community. Methods Mathematical modelling is used to estimate the number of new HIV infections and deaths prevented each year. We use the number of these new HIV infections and deaths prevented, in conjunction with estimated lifetime public health care costs of a new HIV infection, and the value of a life, in order to calculate an identifiable portion of the societal benefits of Insite. The annual costs of operating the SIF are used to measure the social costs of Insite. In using this information, we calculate cost- effectiveness and benefit-cost ratios for the SIF. Results Through the use of conservative estimates, Vancouver's SIF, Insite, on average, prevents 35 new cases of HIV and almost 3 deaths each year. This provides a societal benefit in excess of $6 million per year after the programme costs are taken into account, translating into an average benefit-cost ratio of 5.12:1. Conclusion Vancouver's SIF appears to be an effective and efficient use of public health care resources, based on a modelling study of only two specific and measurable benefits—HIV infection and overdose death.
54. Dissolution of a harm reduction track for opiate agonist treatment: Longitudinal impact on treatment retention, substance use and service utilization International Journal of Drug Policy 2010 21: 82–85 Bryan Hartzler, Ann J. Cotton, Donald A. Calsyn, Rachael Guerra and Edward Gignoux
KEYWORDS: Harm reduction; Opiate agonist treatment; Contingency management
ABSTRACT Background There is great need to sustain harm reduction programmes for opiate-dependent persons, given variable retention of opioid agonist treatment (OAT) enrolees. Resource challenges may lead some health organizations to discontinue such programmes, though just as programmatic evaluation may determine efficacy and cost-effectiveness so to does it aid in examining impacts of programme dissolution. Methods This retrospective evaluation investigated impacts of the dissolution of a ‘Minimal Services’ (MS) harm reduction programme for substance-abusing OAT clientele at an urban U.S. Veterans Affairs Medical Centre. Targeted clinical data concerning treatment retention, substance use and service utilization was abstracted from medical records of MS-assignees (N = 32) and a matched comparison group of
39 standard OAT enrolees. Chart reviewers gathered data for a two-year period encompassing baseline, transitional, and dissolution study phases. Results Relative to matched-controls, MS-assignees exhibited: (1) disproportionately poor treatment retention over the two-year period; (2) high and temporally stable rates of documented substance use across study phases, and (3) increased utilization of resource-laden VAMC services after MS dissolution. Conclusion Collective results suggest MS programme dissolution was associated with adverse conditions for assignees and the larger treatment setting, and reinforce the need for pragmatic, humane treatment policies to facilitate retention of opiate-dependent persons.
55. Methadone Maintenance Dosing Guideline for Opioid Dependence, a Literature Review Journal of Addictive Diseases 2010 29: 1–14 Ayman Fareed, Jennifer Casarella, Richard Amar, Sreedevi Vayalapalli and Karen Drexler
KEYWORDS: Methadone, doing guideline, literature revie
ABSTRACT To date, methadone dosing is still an issue of debate and controversy among clinicians who are involved in methadone maintenance programs. The authors conducted a literature review to update clinicians about this issue and provide recommendations for proper methadone dosing. Studies eligible for inclusion in the review were retrieved from the PubMed database by searching for reports published between 1990 and September 2008 using the major medical subject headings Methadone (all fields) and dose. Only articles written in English were included. Additional reports were identified from the reference lists of retrieved articles and by manual review of the tables of contents of journals on drug of abuse included in the psychiatry and substance abuse subject category listing 2008 of the Journal Citation Reports. Abstracts of medical meetings were excluded. Twenty-four articles were included in the review. Twelve are randomized, controlled, or double-blind clinical trials, 10 are non-randomized and observational studies, and 2 are meta-analyses. Currently, the consensus is to have a goal for methadone dosing in the range of 60 to 100 mg daily. For patients who continue to use illicit opiates while prescribed this dose range, clinicians may consider doses greater than 100 mg daily. However, this is not the current consensus but rather is based on the limited promising data the authors have; it could be considered if the benefits outweigh the risks for some patients.
56. Provision of Ancillary Medications During Buprenorphine Detoxification Does Not Improve Treatment Outcomes Journal of Addictive Diseases 2010 29 (1): 23-29 Maureen Hillhouse, Catherine P. Domier, David Chim and Walter Ling
KEYWORDS: Opioid dependence; buprenorphine; withdrawal; ancillary medications; treatment
ABSTRACT For individuals dependent on opioids, recovery efforts begin with a period of withdrawal that typically includes discomfort from symptoms, possibly precipitating a return to drug use. The study described here investigated whether the provision of ancillary medications for opioid withdrawal symptoms affected treatment outcomes in 139 participants receiving buprenorphine in a 13-day detoxification trial. Outcome measures include the number of opioid-free urine samples collected and retention in treatment. Ancillary medications were provided to 70% of participants: 59% received medication for insomnia, 45% for anxiety, 40% for bone pain, 35% for nausea, and 28% for diarrhea. Findings indicate no difference in the number of opioid-free urine samples between the group receiving ancillary medication and the group who did not, although tests of specific ancillary medications indicate that those who received diarrhea medication had fewer opioid-free urines than those who did
40 not (P = .004). Results also indicate that participants attended fewer days of treatment if they received anxiety, nausea, or diarrhea medication compared to no medication (all P values < .05).
57. Obstructive sleep apnea is more common than central sleep apnea in methadone maintenance patients with subjective sleep complaints Drug and Alcohol Dependence 2010 108(1-2): 77-83 Katherine M. Sharkey, Megan E. Kurth, Bradley J. Anderson, Richard P. Corso, Richard P. Millman and Michael D. Stein
KEYWORDS: Methadone; Opiate dependence; Sleep; Sleep apnea; Central sleep apnea; Obstructive sleep apnea; Sleep-disordered breathing
ABSTRACT Objectives Opioid-dependent patients treated with methadone have subjective sleep complaints and disrupted sleep on polysomnography (PSG). Previous studies of sleep-disordered breathing (SDB) in this population have focused on central sleep apnea (CSA). Our objectives were to: (1) characterize obstructive sleep apnea (OSA) and CSA in patients in methadone maintenance treatment (MMT) for opioid dependence; (2) examine factors associated with SDB in this population; and (3) investigate whether SDB was related to severity of subjective sleep complaints in MMT patients with subjective sleep disturbances. Methods We analyzed OSA and CSA from one night of home PSG in 71 patients who were in MMT for at least 3 months and had a Pittsburgh Sleep Quality Inventory (PSQI) score >5. Results OSA (defined as obstructive apnea–hypopnea index (OAHI) ≥ 5) was observed in 35.2% of our sample. OSA was associated with higher body mass index, longer duration in MMT, and non- Caucasian race. CSA (defined as central apnea index (CAI) ≥ 5) was observed in 14.1% of the sample. CSA was not associated with methadone dose or concomitant drug use. Subjective sleep disturbance measured with the PSQI was not related to OSA or CSA. Conclusions SDB was common in this sample of MMT patients and OSA was more common than CSA. Given the lack of association between presence of SDB and severity of subjective sleep difficulties, factors other than sleep apnea must account for complaints of disturbed sleep in this population.
58. Alcohol usage and associated treatment outcomes for opiate users entering treatment in Ireland Drug and Alcohol Dependence 2010 107(1): 55-61 R.D. Stapleton and C.M. Comiskey,
KEYWORDS: Alcohol use; Opiates; Treatment; Cocaine; Outcome
ABSTRACT Evidence has shown that frequency and quantity of drug usage are reduced after treatment but the effect of opioid addiction treatment on alcohol consumption remains unclear. As part of the national Research Outcome Study in Ireland Evaluating drug treatment effectiveness (ROSIE, see www.nuim.ie/rosie) comprehensive drug and alcohol data on 404 opiate users were collected. This study recruited and followed up at 1 and 3 years a prospective cohort of 404 users entering a new treatment episode. Descriptive and inferential statistics were computed and logistic modelling was used to identify key factors effecting outcomes. The cohort represented 8.2% of all new treatments. Follow-up interview rate at 3 years was 88%. Analysis revealed that those who abstained from alcohol use at 3 years were less likely to be using heroin at 3 years than non-abstainers. In addition, those who abstained from alcohol use at 3 years were also less likely to be using methadone, benzodiazepines and cocaine at 3 years than alcohol users. Outcomes for medium and heavy drinkers were found not to be as good as alcohol abstainers.
41 Finally males tended to reduce the frequency and level of alcohol usage after entering treatment more than females. Results demonstrate to clinicians that an alcohol strategy is a key component of opiate treatment planning and a comprehensive and regular assessment of the client's alcohol and drug use profile is essential if treatment interventions are to have maximum impact on outcomes.
59. Long-term outcomes of office-based buprenorphine/naloxone maintenance therapy Drug and Alcohol Dependence 2010 106 (1): 56-60 T.V. Parran, C.A. Adelman, B. Merkin, M.E. Pagano, R. Defranco, R.A. Ionescu and A.G. Mace
KEYWORDS: Buprenorphine; Office-based; Abstinence; Outcomes; Follow-up; Socioeconomic status
ABSTRACT Background Buprenorphine/naloxone was approved by the FDA for office-based opioid maintenance therapy (OMT), with little long-term follow-up data from actual office-based practice. 18-Month outcome data on the office-based use of buprenorphine/naloxone (bup/nx) and the impact of socioeconomic status and other patient characteristics on the duration and clinical effects of bup/nx are reported. Methods This retrospective chart review and cross-sectional telephone interview provide treatment retention of opioid-dependent patients receiving bup/nx-OMT in an office-based setting. 176 opioid-dependent patients from two different socioeconomic groups (high and low SES) were begun on bup/nx, started intensive outpatient treatment, and followed-up after a minimum of 18 months (18–42 months) by telephone interview to assess treatment outcome. Results 110 subjects (67%) completed the interview, 77% remained on bup/nx with no difference in retention between high and low SES groups. Those on bup/nx at follow-up were more likely to report abstinence, to be affiliated with 12-step recovery, to be employed and to have improved functional status. Conclusions Bup/nx-OMT is a viable treatment option and when coupled with a required abstinence oriented addiction counseling program is effective in promoting abstinence, self-help group attendance, occupational stability, and improved psychosocial outcomes in both low SES and high SES patient populations over an 18–42-month period.
60. Mood Disturbance and Withdrawal Severity in Substitution Treatment for Opioid Dependence: Their Association and Impact on Continued Illicit Drug Use Addictive Disorders & Their Treatment 2010 9 (1): 1-7 Kettler, Lisa, Nikic, Mathew, Newcombe, David and Ali, Robert
ABSTRACT Objectives: This study explored the relationship between withdrawal severity and mood disturbance, and their links with continued illicit drug use during the first 3 months of opioid substitution treatment (ST). Methods: Sixteen participants undergoing opioid ST with methadone (n=7) or buprenorphine (n=9) were recruited through outpatient units in South Australia. In a within-groups repeated measures design, the Opiate Treatment Index was administered at baseline and again at 3 months. Participants also completed the Methadone Symptoms Checklist and the Profile of Mood States at baseline and fortnightly throughout the 3-month measurement period. Results: Withdrawal severity and mood disturbance were observed to co-vary over the 3 months. Statistically significant reductions in both withdrawal severity and mood disturbance were observed. The direction of association between withdrawal severity and mood disturbance was positive and was
42 statistically significant at all measurement points. Continued use of illicit drugs was associated with higher levels of both mood disturbance and withdrawal severity. Conclusions: Withdrawal severity and mood disturbance co-vary over time and have important implications for treatment outcomes in ST.
61. The acceptability of combined methadone-naloxone treatment: Consumer and provider views on the potential utility of methadone-naloxonedar_118 138..143 Drug and Alcohol Review 2010 29: 138–143 James Shearer, Kristie Mammen & James Bell
KEYWORDS methadone-naloxone • qualitative research • consumer views • treatment provider views
ABSTRACT Introduction and Aims. The aim of the study was to investigate the acceptability of methadone- naloxone through interviews with potential consumers and treatment providers about their attitudes and beliefs about combining methadone with naloxone. Design and Methods. Qualitative study with structured surveys and individual interviews with nine consumers and 11 treatment providers. Results. Fear and issues around trust were identified as barriers to consumer acceptance of methadone- naloxone. Respect for the choices that consumers made about their treatment and drug use, and clear and open communication were identified as necessary to win consumer acceptance. Both groups had concerns about the safety and efficacy of methadone-naloxone compared with methadone, but also most identified potential benefits from a new opioid treatment option. Discussion and Conclusions. For both groups, the acceptability of methadone-naloxone depended upon an informed assessment of risks and benefits best addressed by further research into the efficacy, tolerability and safety of methadone-naloxone.[Shearer J, Mammen K, Bell J. The acceptability of combined methadone-naloxone treatment: Consumer and provider views on the potential utility of methadone-naloxone. Drug Alcohol Rev 2009]
62. Drug injecting in patients in New Zealand Methadone Maintenance Drug and Alcohol Review 2010 29: 41–46 Treatment programs: An anonymous survey Graeme Judson, Rupert Bird, Patrick O’connor, Tim Bevin, Richard Loan, Martin Schroder, Richard Mcgrath, Mark Weatherall, Helen Moriarty& Geoff Robinson
KEYWORDS non-government organisation • sustainability • alcohol • drug
ABSTRACT Introduction and Aims. The study aimed to identify issues for sustainability of non-government organisations in the alcohol and other drugs sector (AODS) in Australia within the current neoliberal context. Design and Methods. Six key-informant group consultations were conducted in Sydney, Melbourne, Darwin (Australia). Participants were professionals working in the AODS from non- government AOD organisations, government departments, philanthropic organisations and academic institutions (n = 40). Qualitative data were collected according to a discussion guide. Results. Issues related to problems with workforce capacity, independence, governance and funding. Factors contributing to these issues related to the competitive tendering funding model, for example: accountability requirements and tied funding. Discussion and Conclusions. Issues identified by the AODS were mostly similar to those identified by the broader non-government organisations sector. There is much to learn from outside the AODS. Strategies to improve sustainability will include workforce development, improving governance and developing relationships within the sector and with government. These require a commitment to innovation and will entail movement of resources from service provision in the short term to organisational development for the long term.[Spooner C,
43 Dadich A. Issues for sustainability of non-government organisations in the alcohol and other drugs sector. Drug Alcohol Rev 2009]
63. The Andalusian trial on heroin-assisted treatment: A 2 year follow-updar Drug and Alcohol Review 2010 29: 75–80_100 Eugenia Oviedo-Joekes, Joan C. March, Manuel Romero & Emilio Perea-Milla5
KEYWORDS opioid dependence • heroin-assisted treatment • cohort follow-up • Spain
ABSTRACT Introduction and Aims. In 2003, a randomised controlled trial comparing injected diacetylmorphine and oral methadone was carried out in Andalusia, Spain. The subsequent follow-up study evaluated the health and drug use status of participants, 2 years after the completion of the trial. Design and Methods. This follow-up cohort study was carried out between March and August 2006. Data collected included information on socio-demographics, drug use, health and health-related quality of life. We compared data collected before randomisation and at 2 years for the following three groups: those currently on heroin-assisted treatment (C-HAT), those who have discontinued HAT (D-HAT), and those who have never received HAT (N-HAT). Results. From the total 62 randomised participants in 2003, 54 (87%) were interviewed for this study. Participants were distributed as follow: C-HAT 44.4% (24), N-HAT 22.2% (12) and D-HAT 33.3% (18). Illicit heroin use had a statistically significant decrease in the three groups from baseline to 2 years post trial. Mean days of heroin use were 2.42 (SD = 3.02); 6.56 (SD = 9.48) and 13.92 (SD = 12.59) for the C-HAT, D-HAT and N-HAT groups, respectively. Those currently on HAT were the only group that sustained at 2 years, their marked improvement in health after 9 months of treatment during the trial period. Discussion and Conclusions: Patients who received HAT showed better outcomes compared with those not on HAT. The results of this study strengthen the evidence showing that HAT can improve and stabilise the health of long-term heroin users with severe comorbidities and high mortality.[Oviedo-Joekes E, March JC, Romero M, Perea-Milla E. The Andalusian trial on heroin assisted treatment: A 2 year follow-up. Drug Alcohol Rev 2009]
64. Abuse liability of intravenous buprenorphine/naloxone and buprenorphine alone in buprenorphine-maintained intravenous heroin abusers Addiction 2010 105 (4): 709-718 Sandra D. Comer, Maria A. Sullivan, Suzanne K. Vosburg, Jeanne Manubay, Leslie Amass, Ziva D. Cooper, Phillip Saccone and Herbert D. Kleber
KEYWORDS Abuse liability • breakpoint • buprenorphine/naloxone • drug liking • heroin • intravenous • opioid dependence • progressive-ratio • self-administration
ABSTRACT Background Sublingual buprenorphine is an effective maintenance treatment for opioid dependence, yet intravenous buprenorphine misuse occurs. A buprenorphine/naloxone formulation was developed to mitigate this misuse risk. This randomized, double-blind, cross-over study was conducted to assess the intravenous abuse potential of buprenorphine/naloxone compared with buprenorphine in buprenorphine-maintained injection drug users (IDUs). Methods Intravenous heroin users (n = 12) lived in the hospital for 8–9 weeks and were maintained on each of three different sublingual buprenorphine doses (2 mg, 8 mg, 24 mg). Under each maintenance dose, participants completed laboratory sessions during which the reinforcing and subjective effects of intravenous placebo, naloxone, heroin and low and high doses of buprenorphine and buprenorphine/naloxone were examined. Every participant received each test dose under the three buprenorphine maintenance dose conditions. Results Intravenous buprenorphine/naloxone was self-administered less frequently than buprenorphine or heroin (P < 0.0005). Participants were most likely to self-administer drug
44 intravenously when maintained on the lowest sublingual buprenorphine dose. Subjective ratings of 'drug liking' and 'desire to take the drug again' were lower for buprenorphine/naloxone than for buprenorphine or heroin (P = 0.0001). Participants reported that they would pay significantly less money for buprenorphine/naloxone than for buprenorphine or heroin (P < 0.05). Seven adverse events were reported; most were mild and transient. Conclusions These data suggest that although the buprenorphine/naloxone combination has intravenous abuse potential, that potential is lower than it is for buprenorphine alone, particularly when participants received higher maintenance doses and lower buprenorphine/naloxone challenge doses. Buprenorphine/naloxone may be a reasonable option for managing the risk for buprenorphine misuse during opioid dependence treatment.
65. The effect of time spent in treatment and dropout status on rates of convictions, cautions and imprisonment over 5 years in a primary care-led methadone maintenance service Addiction 2010 105 (4): 732-739 Phillip Oliver, Jenny Keen, Georgina Rowse, Elizabeth Ewins, Laura Griffiths, Nigel Mathers
KEYWORDS Crime • heroin • methadone • methadone maintenance treatment • MMT • primary care
ABSTRACT Background Methadone maintenance treatment (MMT) in primary care settings is used increasingly as a standard method of delivering treatment for heroin users. It has been shown to reduce criminal activity and incarceration over periods of periods of 12 months or less; however, little is known about the effect of this treatment over longer durations. Aims To examine the association between treatment status and rates of convictions and cautions (judicial disposals) over a 5-year period in a cohort of heroin users treated in a general practitioner (GP)-led MMT service. Design Cohort study. Setting The primary care clinic for drug dependence, Sheffield, 1999–2005. Participants The cohort comprised 108 consecutive patients who were eligible and entered treatment. Ninety were followed-up for the full 5 years. Intervention The intervention consisted of MMT provided by GPs in a primary care clinic setting. Measurements Criminal conviction and caution rates and time spent in prison, derived from Police National Computer (PNC) criminal records. Findings The overall reduction in the number of convictions and cautions expected for patients entering MMT in similar primary care settings is 10% for each 6 months retained in treatment. Patients in continuous treatment had the greatest reduction in judicial disposal rates, similar to those who were discharged for positive reasons (e.g. drug free). Patients who had more than one treatment episode over the observation period did no better than those who dropped out of treatment. Conclusions MMT delivered in a primary care clinic setting is effective in reducing convictions and cautions and incarceration over an extended period. Continuous treatment is associated with the greatest reductions.
66. Does opioid substitution treatment in prisons reduce injecting-related HIV risk behaviours? A systematic review Addiction 2010 105 (2): 216-223 Sarah Larney
KEYWORDS Buprenorphine • heroin dependence • HIV • methodone • prisons • review
ABSTRACT
45 Objectives To review systematically the evidence on opioid substitution treatment (OST) in prisons in reducing injecting-related human immunodeficiency virus (HIV) risk behaviours. Methods Systematic review in accordance with guidelines of the Cochrane Collaboration. Electronic databases were searched to identify studies of prison-based opioid substitution treatment programmes that included assessment of effects of prison OST on injecting drug use, sharing of needles and syringes and HIV incidence. Published data were used to calculate risk ratios for outcomes of interest. Risk ratios were not pooled due to the low number of studies and differences in study designs. Results Five studies were included in the review. Poor follow-up rates were reported in two studies, and representativeness of the sample was uncertain in the remaining three studies. Compared to inmates in control conditions, for treated inmates the risk of injecting drug use was reduced by 55– 75% and risk of needle and syringe sharing was reduced by 47–73%. No study reported a direct effect of prison OST on HIV incidence. Conclusions There may be a role for OST in preventing HIV transmission in prisons, but methodologically rigorous research addressing this question specifically is required. OST should be implemented in prisons as part of comprehensive HIV prevention programmes that also provide condoms and sterile injecting and tattooing equipment.
67. Outcome of long-term heroin-assisted treatment offered to chronic, treatment-resistant heroin addicts in the Netherlands Addiction 2010 105 (2): 300-308 Peter Blanken, Vincent M. Hendriks, Jan M. van Ree and Wim van den Brink
KEYWORDS Diamorphine • heroin • heroin-assisted treatment • long-term outcome • opioid dependence
ABSTRACT Aims To describe 4-year treatment retention and treatment response among chronic, treatment- resistant heroin-dependent patients offered long-term heroin-assisted treatment (HAT) in the Netherlands. Design Observational cohort study. Setting and intervention Out-patient treatment in specialized heroin treatment centres in six cities in the Netherlands, with methadone plus injectable or inhalable heroin offered 7 days per week, three times per day. Prescription of methadone plus heroin was supplemented with individually tailored psychosocial and medical support. Participants Heroin-dependent patients who had responded positively to HAT in two randomized controlled trials and were eligible for long-term heroin-assisted treatment (n = 149). Measurements Primary outcome measures were treatment retention after 4 years and treatment response on a dichotomous, multi-domain response index, comprising physical, mental and social health and illicit substance use. Findings Four-year retention was 55.7% [95% confidence interval (CI): 47.6–63.8%]. Treatment Response was significantly better for patients continuing 4 years of HAT compared to patients who discontinued treatment: 90.4% versus 21.2% [difference 69.2%; odds ratio (OR) = 48.4, 95% CI: 17.6–159.1]. Continued HAT treatment was also associated with an increasing proportion of patients without health problems and who had stopped illicit drug and excessive alcohol use: from 12% after the first year to 25% after 4 years of HAT. Conclusions Long-term HAT is an effective treatment for chronic heroin addicts who have failed to benefit from methadone maintenance treatment. Four years of HAT is associated with stable physical, mental and social health and with absence of illicit heroin use and substantial reductions in cocaine use. HAT should be continued as long as there is no compelling reason to stop treatment.
68. Problems experienced by community pharmacists delivering opioid substitution treatment in New South Wales and Victoria, Australia Addiction 2010 105 (2): 335-342 Adam R. Winstock, Toby Lea and Janie Sheridan
46 KEYWORDS Buprenorphine • community pharmacy • methadone • opioid substitution therapy • prescriber • problems • termination
ABSTRACT Aims To explore service provision and the range of problems that New South Wales (NSW) and Victoria (VIC) community pharmacists providing opioid substitution treatment (OST) have experienced with clients and prescribers. Design Cross-sectional postal survey. Setting All community pharmacies providing OST in NSW (n = 593) and VIC (n = 393), Australia. Participants Completed questionnaires were received from 669 pharmacists (68% response rate). Measurements The questionnaire addressed pharmacy characteristics, recent problems experienced with clients including refusal to dose, provision of credit for dispensing fees, termination of treatment, responses of pharmacists to problems experienced with clients, as well as problems experienced with OST prescribers. Findings In the preceding month, 41% of pharmacists had refused to dose a client for any reason, due most commonly to expired prescriptions (29%), or ≥3 missed doses (23%). Terminating a client's treatment in the past month was reported among 14% of respondents, due most commonly to inappropriate behaviour and missed doses. Treatment termination was reported by a significantly higher proportion of pharmacists in VIC (P < 0.001). Treatment termination in last month was predicted having more clients (P < 0.001), the provision of buprenorphine treatment (P = 0.008), having a separate dosing area (P = 0.021), and being a female pharmacist (P = 0.013). Past month refusal to dose was predicted by the pharmacy being in VIC (P < 0.001) and having more clients (P < 0.001). Problems experienced most commonly in the past month with prescribers were difficulty contacting prescriber (21%) and provision of takeaway doses to clients considered unstable by the pharmacist (19%) (higher in VIC: both P < 0.001). Conclusions This study highlights the range of problems experienced by community pharmacists in the delivery of OST and the consequences for people in treatment. Particular attention should be focused upon considering number of clients per pharmacy and improving professional communication between pharmacists and prescribers.
69. Heroin-assisted treatment in Switzerland: a case study in policy change Addiction 2010 105 (1): 29-37 Ambros Uchtenhagen
KEYWORDS Drug policy • drug treatment • harm reduction • heroin • heroin prescribing • opiate substitution treatment
ABSTRACT Background Switzerland introduced a pragmatic national drug policy when the former conservative abstinence-orientated politics proved unable to cope with an escalating number of users and related negative consequences for public health and public order. The high visibility of 'needle parks' and the size of the acquired immune deficiency disorder (AIDS) epidemic called for a new approach and for national leadership. Aims To describe the intentions, the process and the results of setting up the new treatment approach of prescribing heroin to treatment resistant heroin addicts, as an example of drug policy change. Materials and Methods A systematic collection of relevant documents is analysed and used as evidence for describing the process of policy change. Results Measures to reduce the negative consequences of continued use and to prevent the spread of AIDS were started mainly by private initiatives and soon taken up officially in the 'four-pillar' drug policy (including harm reduction, prevention, treatment and law enforcement). Medical prescription of heroin to chronic, treatment-resistant heroin addicts was one of the innovations, based on extensive scientific and political preparation. Detailed documentation and evaluation, ample communication of results, adaptations made on the basis of results and extensive public debate helped to consolidate the new policy and heroin-assisted treatment, in spite of its limitations as an observational cohort study. All necessary steps were taken to proceed from a scientific experiment to a routine procedure. Discussion Comparable policy changes have been observed in a few other countries, such as The Netherlands and Germany, based on the Swiss experience, with equally positive results of heroin-
47 assisted treatment. These experiments were designed as randomised controlled trials, comparing intravenous heroin against oral methadone, thereby demonstrating the specific value of pharmaceutical diamorphine for maintenance treatment in opiate dependence. The positive impact of policy change and the positive outcomes of heroin-assisted treatment were acknowledged increasingly nationally and internationally, but made it difficult to continue the process of adapting policy to new challenges, due to the low visibility of present drug problems and to changing political priorities. Conclusion A major change in drug policy was effectively realised under typical conditions of a federalist country with a longstanding tradition of democratic consensus building. Facilitating factors were the size and visibility of the heroin problem, the rise of the Aids epidemic, and a pragmatic attitude of tolerating private initiatives opening the way to official policy change.
Organisation of Treatment
70. Using enhanced and integrated services to improve response to standard methadone treatment: Changing the clinical infrastructure of treatment networks Journal of Substance Abuse Treatment 2010 38 (2): 170-177 Karin Neufeld, Michael Kidorf, Van King, Ken Stoller, Michael Clark, Jessica Peirce and Robert K. Brooner
KEYWORDS: Opioid dependence; Substance abuse treatment; Treatment systems
ABSTRACT Outcomes are presented from opioid-dependent outpatients (N = 81) participating in a new community-based initiative designed to improve access to enhanced substance abuse and psychiatric services in a publicly supported methadone maintenance treatment network in Baltimore, MD. The initiative, entitled Community Access to Specialized Treatment (CAST), is located at the Addiction Treatment Services, a program within this network. Network programs referred patients engaged in unremitting drug use who are at risk for discharge to CAST, where they received methadone substitution, individual and group counseling within an adaptive platform, behavioral contingencies to reinforce adherence, and on-site psychiatric evaluation and care. Patients returned to their referring program after producing at least two consecutive weeks of drug-negative urine samples and full counseling adherence. CAST was well utilized by the community. Patients had high rates of adherence to scheduled individual and group counseling services (93% and 73%, respectively); 43% of referrals successfully completed the program in an average of 101 days. This community-wide service delivery approach is a novel alternative to integrating intensive substance abuse and psychiatric care at each program within a treatment network.
Pregnancy
71. Brief screening questionnaires to identify problem drinking during pregnancy: a systematic review Addiction 2010 105 (4): 601-614 Ethel Burns, Ron Gray and Lesley A. Smith
KEYWORDS Alcohol • prenatal • questionnaires • screening • sensitivity • specificity • systematic review
ABSTRACT Aims Although prenatal screening for problem drinking during pregnancy has been recommended, guidance on screening instruments is lacking. We investigated the sensitivity, specificity and predictive value of brief alcohol screening questionnaires to identify problem drinking in pregnant women.
48 Methods Electronic databases from their inception to June 2008 were searched, as well as reference lists of eligible papers and related review papers. We sought cohort or cross-sectional studies that compared one or more brief alcohol screening questionnaire(s) with reference criteria obtained using structured interviews to detect 'at-risk' drinking, alcohol abuse or dependency in pregnant women receiving prenatal care. Results Five studies (6724 participants) were included. In total, seven instruments were evaluated: TWEAK (Tolerance, Worried, Eye-opener, Amnesia, Kut down), T-ACE [Take (number of drinks), Annoyed, Cut down, Eye-opener], CAGE (Cut down, Annoyed, Guilt, Eye-opener], NET (Normal drinker, Eye-opener, Tolerance), AUDIT (Alcohol Use Disorder Identification Test), AUDIT-C (AUDIT- consumption) and SMAST (Short Michigan Alcohol Screening Test). Study quality was generally good, but lack of blinding was a common weakness. For risk drinking sensitivity was highest for T- ACE (69-88%), TWEAK (71–91%) and AUDIT-C (95%), with high specificity (71–89%, 73–83% and 85%, respectively). CAGE and SMAST performed poorly. Sensitivity of AUDIT-C at score ≥3 was high for past year alcohol dependence (100%) or alcohol use disorder (96%) with moderate specificity (71% each). For life-time alcohol dependency the AUDIT at score ≥8 performed poorly. Conclusion T-ACE, TWEAK and AUDIT-C show promise for screening for risk drinking, and AUDIT- C may also be useful for identifying alcohol dependency or abuse. However, their performance as stand-alone tools is uncertain, and further evaluation of questionnaires for prenatal alcohol use is warranted.
Psychostimulants
72. Randomized controlled trial of dexamphetamine maintenance for the treatment of methamphetamine dependence_ Addiction 2010 105 (1): 146-154754 Marie Longo, Wendy Wickes, Matthew Smout, Sonia Harrison, Sharon Cahill & Jason M. White
KEYWORDS Dependence, dexamphetamine, maintenance, methamphetamine, pharmacotherapy, randomized controlled trial, treatment.
ABSTRACT Aim To investigate the safety and efficacy of once-daily supervised oral administration of sustained- release dexamphetamine in people dependent on methamphetamine. Design Randomized, double- blind, placebo-controlled trial. Participants Forty-nine methamphetamine-dependent drug users from Drug and Alcohol Services South Australia (DASSA) clinics. Intervention Participants were assigned randomly to receive up to 110 mg/day sustained release dexamphetamine (n = 23) or placebo (n = 26) for a maximum of 12 weeks, with gradual reduction of the study medication over an additional 4 weeks. Medication was taken daily under pharmacist supervision. Measurements Primary outcome measures included treatment retention, measures of methamphetamine consumption (self-report and hair analysis), degree of methamphetamine dependence and severity of methamphetamine withdrawal. Hair samples were analysed for methamphetamine using liquid chromatography-mass spectrometry. Findings Treatment retention was significantly different between groups, with those who received dexamphetamine remaining in treatment for an average of 86.3 days compared with 48.6 days for those receiving placebo (P = 0.014). There were significant reductions in self-reported methamphetamine use between baseline and follow-up within each group (P < 0.0001), with a trend to a greater reduction among the dexamphetamine group (P = 0.086). Based on hair analysis, there was a significant decrease in methamphetamine concentration for both groups (P < 0.0001). At follow-up, degree of methamphetamine dependence was significantly lower in the dexamphetamine group (P = 0.042). Dexamphetamine maintenance was not associated with serious adverse events. Conclusions The results of this preliminary study have demonstrated that a maintenance pharmacotherapy programme of daily sustained release amphetamine dispensing under pharmacist supervision is both feasible and safe. The increased retention in the dexamphetamine group, together with the general decreases in methamphetamine use, degree of dependence and withdrawal symptom severity, provide preliminary evidence that this may be an efficacious treatment option for methamphetamine dependence.
49 Public Health
73. Prevention programs in the 21st century: what we do not discuss in public Addiction 2010 105 (4): 578-581 Harold Holder
KEYWORDS Prevention research • selection bias • self-report • statistical analyses
ABSTRACT Prevention research concerning alcohol, tobacco and other drugs faces a number of challenges as the scientific foundation is strengthened for the future. Seven issues which the prevention research field should address are discussed: lack of transparency in analyses of prevention program outcomes, lack of disclosure of copyright and potential for profit/income during publication, post-hoc outcome variable selection and reporting only outcomes which show positive and statistical significance at any follow-up point, tendency to evaluate statistical significance only rather than practical significance as well, problem of selection bias in terms of selecting subjects and limited generalizability, the need for confirmation of outcomes in which only self-report data are used and selection of appropriate statistical distributions in conducting significance testing. In order to establish a solid scientific base for alcohol, tobacco and drug prevention, this paper calls for discussions, disclosures and debates about the above issues (and others) as essential. In summary, the best approach is always transparency.
74. How much alcohol do you buy? A comparison of self-reported alcohol purchases with actual sales Addiction 2010 105 (4): 649-654 Mats Ramstedt
KEYWORDS Alcohol purchase • coverage rate • self-report • Sweden • unrecorded alcohol • validity of survey data
ABSTRACT Background Unrecorded alcohol has increased in the Nordic countries during recent years, above all in terms of cross-border trade. This implies that trends and levels of per capita consumption would look different without estimates of this source of alcohol, estimates that in Sweden and other countries are made through surveys. Aim The overall aim is to analyse the validity of Swedish survey estimates of alcohol bought in the cross-border trade and possibly to develop weights that can be applied to such estimates. Data and method The analysis consists of comparing self-reported purchases of spirits, wine, cider/alcopops and beer at retail monopoly (Systembolaget) during 2008 (n = 18 000) with actual sales during the same period overall and monthly. Findings Of the recorded amount of purchases at Systembolaget, 87% was reported in the survey, compared with the 40–60% usually found for self-reported consumption. Significant differences across beverages were revealed, showing a lower coverage rate for beer and spirits and a higher coverage rate for wine and cider. Changes in purchases of all beverages were captured fairly well, at least changes taking place from one month to another. Conclusions Self-reported alcohol purchases achieve a higher coverage rate than found typically in studies based on self-reported use of alcohol. If adjustments are to be made to correct for underreporting in self-reported data on alcohol purchases, different weights should be applied to different beverages. Furthermore, at least major changes in how much alcohol is purchased in the population can be monitored using well-designed population surveys.
50 75. Policy options for alcohol price regulation: the importance of modelling population heterogeneity Addiction 2010 105 (3): 383-393 Petra Sylvia Meier, Robin Purshouse, Alan Brennan
KEYWORDS Alcohol • alcohol policy • consumption patterns • economic evaluation • methodology • modelling • price
ABSTRACT Context and aims Internationally, the repertoire of alcohol pricing policies has expanded to include targeted taxation, inflation-linked taxation, taxation based on alcohol-by-volume (ABV), minimum pricing policies (general or targeted), bans of below-cost selling and restricting price-based promotions. Policy makers clearly need to consider how options compare in reducing harms at the population level, but are also required to demonstrate proportionality of their actions, which necessitates a detailed understanding of policy effects on different population subgroups. This paper presents selected findings from a policy appraisal for the UK government and discusses the importance of accounting for population heterogeneity in such analyses. Method We have built a causal, deterministic, epidemiological model which takes account of differential preferences by population subgroups defined by age, gender and level of drinking (moderate, hazardous, harmful). We consider purchasing preferences in terms of the types and volumes of alcoholic beverages, prices paid and the balance between bars, clubs and restaurants as opposed to supermarkets and off-licenses. Results Age, sex and level of drinking fundamentally affect beverage preferences, drinking location, prices paid, price sensitivity and tendency to substitute for other beverage types. Pricing policies vary in their impact on different product types, price points and venues, thus having distinctly different effects on subgroups. Because population subgroups also have substantially different risk profiles for harms, policies are differentially effective in reducing health, crime, work-place absence and unemployment harms. Conclusion Policy appraisals must account for population heterogeneity and complexity if resulting interventions are to be well considered, proportionate, effective and cost-effective.
Research Methods
76. The reliability and validity of drug users' self reports of amphetamine use among primarily heroin and cocaine users Addictive Behaviours 2010 35 (4): 350-354 Lucy E. Napper, Dennis G. Fisher, Mark E. Johnson and Michele M. Wood
KEYWORDS: Amphetamine; Reliability; Validity; Self-report
ABSTRACT Relatively few studies have addressed the psychometric properties of self-report measures of amphetamine use. This study examines the reliability and validity of the Risk Behavior Assessment's (RBA) lifetime and recent amphetamine-use questions. To evaluate validity, 4027 out-of-treatment primarily cocaine and heroin users provided urine samples that were compared to self-report data; to evaluate reliability, 218 completed the RBA at two time points, 48 h apart. In the overall sample, self- reports demonstrated moderately high validity, with a 95% accuracy rate (kappa = .54). When analysis was restricted to recent amphetamine users validity was slightly lower (71.5% accuracy; kappa = .41). Test–retest data indicated good reliability for self-reports of ever having used amphetamine (kappa = .79), and amphetamine use in the past 30 days (.75 < r < .91). Out-of- treatment drug users provided accurate self-reports of amphetamine use. Reliable and valid measures are essential for describing and predicting trends in amphetamine use, evaluating the effectiveness of interventions, and developing policies and programs.
51 77. The challenge of external validity in policy-relevant systematic reviews: a case study from the field of substance misuse_ Addiction 2010 105 (1): 136-1457 Mark Pearson & Ross Coomber
KEYWORDS Environmental influences, guidance development, policy, substance misuse in the young, systematic review methods.
ABSTRACT Aim To critically evaluate the methods utilized in the conduct of a systematic review in the field of substance misuse Design Participant-observation in the review process, semi-structured interviews with review team members and management and structured observation of the process of guidance development. Setting An ‘arm’s-length’ government body. Participants Review team members, management and the committee responsible for producing evidence based guidance for policy and practice. Measurements Data from interviews and (participant-) observation were reflected upon critically in order to increase understanding of the systematic review process. Findings The application of systematic review methods produced an evidence base that did not inform the development of guidance to the extent that it could have done: (i) an emphasis upon internal research validity produced an evidence base with an emphasis on short-term interventions at the level of the individual; (ii) criteria for appraising the external validity of studies were not developed sufficiently; and (iii) the systematic review of evidence and development of guidance are strongly reliant upon the judgement of reviewers and committee members. Conclusions Prioritizing internal validity in a systematic review risks producing an evidence base that is not informed adequately by the wider determinants of health and which does not give sufficient consideration to external validity. The use of appropriate methods requires that commissioners of systematic reviews are clear at the outset how the review is proposed to be utilized. Review methods such as meta-ethnography and realist synthesis could contribute to making the frameworks within which judgements are made more explicit.
Young people
78. Impact of a Social Skills Intervention on the Hostile Attributions of Children With Prenatal Alcohol Exposure Alcoholism: Clinical Experimental Research 2010 34 (2): 231-241 Vivien Keil, Blair Paley, Fred Frankel, and Mary J. O'Connor
KEYWORDS Prenatal Alcohol Exposure • Social Skills • Hostile Attributions
ABSTRACT Background: Prenatal alcohol exposure (PAE) has been linked to a wide array of developmental deficits, including significant impairments in social skills. Given the extensive body of evidence linking social information-processing patterns with social behavior, it is possible that social information- processing may represent one mechanism of behavioral change. The present investigation sought to answer the question of whether a well-established social skills intervention decreased the hostile attributions of children with PAE. Further, was there a differential impact of the intervention on hostile attributions in the context of peer provocation versus group entry scenarios? Methods: Participants consisted of 100 children (51% male) with PAE between the ages of 6 and 12 years. Participants were randomly assigned to either a social skills intervention, Children's Friendship Training (CFT), or to a Delayed Treatment Control (DTC) condition. Results: Analyses indicated that the social skills intervention resulted in a significantly lower proportion of hostile attributions in peer group entry, but not peer provocation, scenarios. This decrease was maintained over a 3-month follow-up period. Conclusions: Deficits in social information-processing among individuals with PAE can be improved through social skills intervention, and these changes may lead to more positive developmental outcomes.
52 79. Young people and drugs: Next generation of harm reduction International Journal of Drug Policy 2010 21 (2): 12-114 Simona Merkinaite, Jean Paul Grund and Allen Frimpong
KEYWORDS: Young people; Harm reduction; Drug injecting
ABSTRACT Globally, young people under 25 accounted for an estimated 45% of all new HIV infections in 2007. Across the Eastern Europe and Central Asia region as many as 25% of injecting drug users (IDUs) are younger than 20. The Eurasian Harm Reduction assessment of young peoples’ (under 25) drug use, risk behaviours and service availability and accessibility confirms, young people at risk of injecting, or those already experimenting with injecting drugs, find themselves isolated from health and prevention services, which increases the risks for health and social harms, while the approach towards young peoples’ use rely heavily on law enforcement. Denying young drug users’ access to life-saving drug treatment and other harm reduction services contributes to the risk environment surrounding their use and violates their right to health and well-being as identified in the Convention on the Rights of the Child. Governments, health care providers and harm reduction services should work together to create an environment in which young people can access needed services, including non-judgmental and low-threshold approaches offered by harm reduction programs.
80. Do parents and school matter? Protective factors for adolescent substance use Addictive Behaviours 2010 35 (1): 53-56 Bettina F. Piko and Eszter Kovács
KEYWORDS: Substance use; Protective factors; Parental monitoring; Social support; School climate
ABSTRACT Protective factors may promote successful development by neutralizing the effects of negative risk factors. This paper is focused on possible protective factors of adolescent substance in a sample of high school students (N = 881) in Szeged, Hungary. Data were collected in 2008. Self-administered questionnaires were applied that measured smoking, binge drinking, marijuana use and parental and school-related protective factors. Multiple regression analysis revealed that parental monitoring was a universal protective factor for adolescents. Acceptance and respect of parents' values may serve as a protection against binge drinking among adolescents. High academic achievement was a predictor of smoking and binge drinking, talking about problems with teachers and being happy with school were predictors of marijuana use. Future research is needed to clarify the altered role of parent–child relationship in adolescents' substance use.
81. Using sensation seeking to target adolescents for substance use interventions Addiction 2010 105 (3): 506-514 James D. Sargent, Susanne Tanski, Mike Stoolmiller and Reiner Hanewinkel
KEYWORDS Adolescent • binge drinking • false positive rate • longitudinal • predictive validity • receiver operating characteristic curve • sensation seeking • sensitivity • smoking
ABSTRACT Aims This study examines the predictive validity of sensation seeking as a predictor of adolescent substance use, in order to optimize targeting for substance use prevention programs. Design Longitudinal study. Setting Random-digit dial telephone survey. Participants A total of 6522 US adolescents aged 10–14 years at baseline, resurveyed at 8-month intervals for three subsequent waves.
53 Measurements Two outcomes were assessed—onset of binge drinking (more than five drinks in a short time) and established smoking (>100 cigarettes life-time). Sensation seeking level was assessed at baseline. Logistic regression was used to predict onset of substance use at any follow-up wave as a function of sensation seeking. The receiver operating characteristics curve was used to illustrate how well sensation seeking predicted substance use as a function of different cut-off points for defining high sensation seeking, and area under the receiver operating characteristics curve (AROC) was the metric of predictive validity. Findings Of 5834 participants with one or more follow-up assessments, 5634 reported no binge drinking and 5802 were not established smokers at baseline, of whom 717 (12.7% of 5634) reported binge drinking and 144 (2.5% of 5802) reported established smoking at one or more follow-up interviews. Sensation seeking predicted binge drinking moderately well [AROC = 0.71 (95% confidence interval 0.69, 0.73)] and was a significantly better predictor of established smoking onset [AROC = 0.80 (0.76, 0.83)]. For binge drinking, predictive validity was significantly lower in blacks; for established smoking it was significantly higher for Hispanics. Implications for two targeting interventions are discussed. Conclusions Sensation seeking works moderately well at identifying adolescents at risk for onset of binge drinking and established smoking. This study offers a guide for determining the appropriate targeting cut-off value, based on intervention efficacy, costs and risks.
54