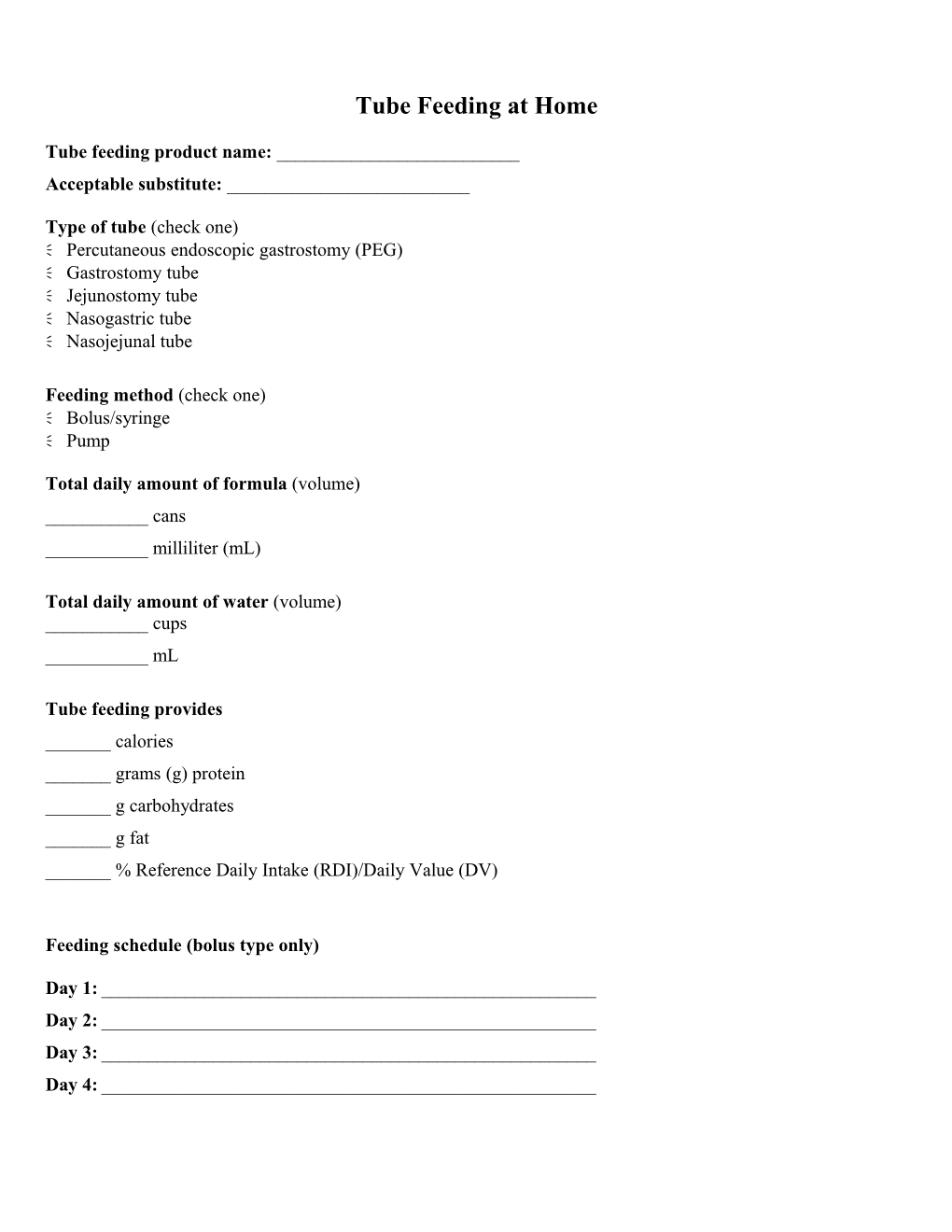
Tube Feeding at Home
Tube feeding product name: ______Acceptable substitute: ______
Type of tube (check one) Percutaneous endoscopic gastrostomy (PEG) Gastrostomy tube Jejunostomy tube Nasogastric tube Nasojejunal tube
Feeding method (check one) Bolus/syringe Pump
Total daily amount of formula (volume) ______cans ______milliliter (mL)
Total daily amount of water (volume) ______cups ______mL
Tube feeding provides ______calories ______grams (g) protein ______g carbohydrates ______g fat ______% Reference Daily Intake (RDI)/Daily Value (DV)
Feeding schedule (bolus type only)
Day 1: ______Day 2: ______Day 3: ______Day 4: ______Feeding schedule (pump type only)
Initial rate: ______Goal rate: ______
Instructions for advancing rate: ______Registered dietitian’s name/phone: ______Home health name/phone: ______Company/phone for tube-feeding supplies: ______
Preparing tube feeding Always clean hands and work area before administering tube feeding. It is best to sit upright or stand when receiving the tube feeding. If lying down, make sure the upper body is at least at a 45 angle to ensure that the tube feeding is flowing into the stomach more efficiently. Stay upright for 30 minutes after a feeding. Have tube feeding supplies ready. Wipe off the tops of the containers with a clean, wet paper towel. Gently shake the formula containers from side to side, not up and down. Do not put anything down the tube other than medications, water, and formula, unless directed to by your physician. Store unopened formula cans in a clean, dry area, off of the floor.
Checking gastric (stomach) residuals Residuals are the amount of food/formula left in the stomach after a period of time. Residuals are checked before each feeding is administered. Residuals are checked by placing the syringe into the feeding tube port (with the plunger already down) and slowly pulling back on the syringe until no more liquid comes out. If more than 200 mL of residuals are obtained at a check, place the contents back into the stomach and hold the feeding. Recheck the residuals in 1 hour. If the residuals have decreased, proceed with the next feeding. Controversy exists among professionals as to whether or not to check residuals at each feeding and at which level of residuals to hold the feeding. Check with your health care provider for guidance.
Bolus or syringe feeding procedure Remove the plunger from the syringe. Place the tip of the syringe into the feeding tube. Hold the syringe and the feeding tube straight up. Slowly pour the formula into the syringe. It should take about 15 to 20 minutes for one can of formula to run or flow into the feeding tube. Note: You should not need to use the syringe plunger to “push” the formula in. Lower the feeding tube with the syringe attached to make the formula run slower. Raise the feeding tube to allow the formula to run in faster. Disconnect the syringe from the feeding tube when the feeding is complete, and flush the tube with the prescribed amount of water. Close the feeding port. Remain upright for 30 minutes after the feeding. Make sure to cover, date, and refrigerate any opened, unused cans. Use or discard within 24 hours. Rinse and recycle empty cans. Remove partially used cans of formula from the refrigerator 30 minutes before a feeding to allow the formula to reach room temperature. Extreme temperature changes to the formula (hot/cold) may cause gastrointestinal distress (loose stools/diarrhea).
Pump-administered feeding procedure Each individual home health agency uses different products and equipment. Your home health nurse will provide instructions on the general use and care of the specific feeding pump ordered for you to use at home. Make sure to talk with your home health nurse about any concerns you may have about using the feeding pump.
Caring for the tube site Daily care and maintenance of your tube and tube site are important parts of your tube-feeding routine. Your home health nurse will give you specific instructions. Contact your home health nurse if you have any questions about how to care for or clean the tube and tube site.
Problem solving Contact your physician or home health nurse if you experience any of the following: A hard or distended (swollen) stomach Symptoms of dehydration, such as: – Weight loss of more than 2 pounds/week – A decrease in the usual amount of urine – Darker-colored or stronger-smelling urine – Thirst – Dry mouth or cracked lips – Large quantities of diarrhea that occur for more than 2 days – Vomiting that does not stop in 24 hours Constipation that does not resolve A clogged tube that does not unclog after trying to gently “push” warm water into the tube several times Any redness, swelling, pain, or drainage at the tube site Missed feedings for more than 1 day because of an intolerance Symptoms of aspiration, such as: – Unusual coughing or choking – Difficulty breathing – “Gurgling” or wet voice quality Unusual weakness, fever, or difficulty breathing
References and recommended readings Tools for living better on home IV & tube feedings. The Oley Foundation Web site. http://www.oley.org/tubetalks.html. Updated April 9, 2013. Accessed May 6, 2013.
University Health Network Clinical Nutrition. Tube feeding at home. http://www.uhn.ca/Patients_&_Visitors/health_info/topics/documents/core_clinical_services/clinical_nutrition/uhn flv026532-doc.pdf. Published May 2006. Accessed May 6, 2013. Review Date 5/13 G-0504