1
MASS TRANSPORT
Multicellular organisms cannot exchange gases, nutrients and waste products directly with the environment because their surface area to volume ratio is too small, and diffusion is only effective over short distances. However all cells within the organism need a supply of oxygen and glucose. Wastes such as urea and carbon dioxide need to be excreted. Hormones such as insulin need to be transported around the organism. In order to ensure that these substances are transported effectively around the body, organisms larger than an earthworm use mass transport. This is the movement of relatively large amounts of material at relatively high speed. In most animals, mass transport forces liquid to flow along a system of tubes.
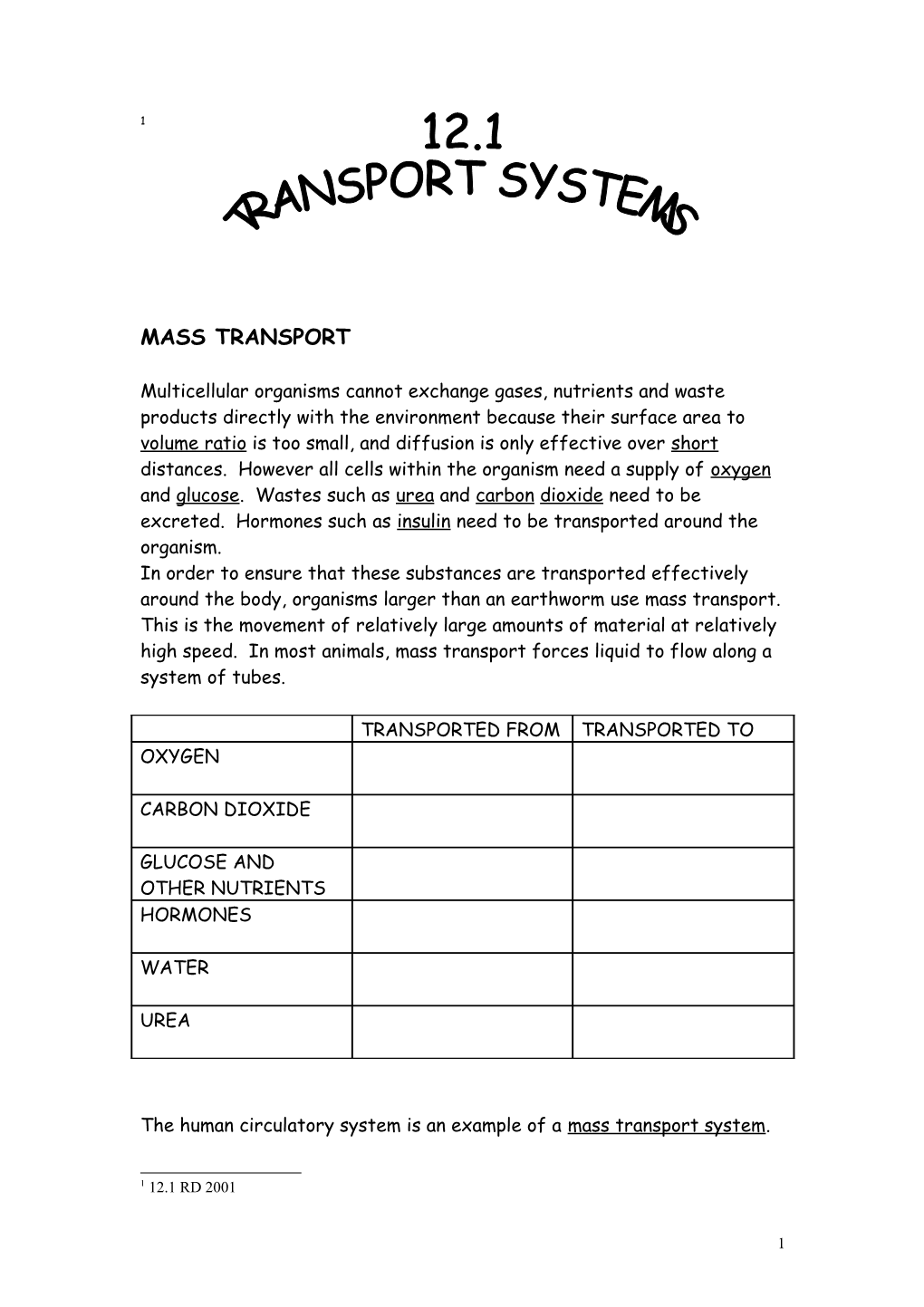
TRANSPORTED FROM TRANSPORTED TO OXYGEN
CARBON DIOXIDE
GLUCOSE AND OTHER NUTRIENTS HORMONES
WATER
UREA
The human circulatory system is an example of a mass transport system.
1 12.1 RD 2001
1 MAMMALIAN CIRCULATORY SYSTEM
In humans the mass transport system is called the circulatory system. The heart ( a muscular pump) forces blood through a series of blood vessels called arteries, capillaries and veins. As blood flows through these vessels substances are exchanged between the blood and the tissues.
Strucutre of the Circulatory system
2 MAMMALIAN HEART
The heart is divided into two muscular pumps.
The right side of the heart collects deoxygenated blood from the body tissues and pumps it to the lungs.
The left side of the heart collects oxygenated blood from the lungs and pumps it to the body tissues.
The human circulatory system is called a double circulatory system.
Why is it necessary to have two circulatory systems?
Each side of the heart has two chambers called the atria and the ventricles. There are valves between each chamber of the heart in order to ensure that the blood flows in one direction only.
Structure of the heart
3 STRUCUTRE FUNCTION
THE CARDIAC CYCLE
4 Pressure changes during the Cardiac Cycle
5 BLOOD VESSELS There are three main types of blood vessel
Arteries which carry blood away from the heart Veins which carry blood towards the heart Capillaries which connect the two together
Structure of Arteries Veins and Capillaries
6 Arteries The walls of arteries contain a thick layer of elastic tissue which is stretched by the pressure produced by ventricular systole. During ventricular diastole, the elastic recoil of the artery walls helps to maintain blood flow along the artery.
The arteries branch to form arterioles. In arterioles the thickest layer of the wall consists of muscle fibres. These muscles act as controls to the flow of blood to certain tissues by contracting (to restrict blood flow) and relaxing (to increase blood flow).
As the arteries sub divide further, the pressure in the blood vessels decreases because the total cross sectional area of all the smaller vessels is greater than that of the larger vessels.
Capillaries Capillary walls are made up of a single layer of endothelial cells. The blood flow and velocity are slowest in the capillaries. Exchange of materials such as carbon dioxide, oxygen and soluble food molecules occurs between the blood and the tissues in the capillaries. The capillaries have small gaps between adjacent endothelial cells called fenestrations which allow even faster rates of diffusion.
Veins The walls of veins contain both elastic and muscle tissue. The pressure of the blood is low so veins have valves to prevent back flow of blood. Three mechanisms keep the blood in the veins flowing towards the heart;
The small residual pressure of blood coming from the capillaries
The reduced pressure in the atria at atrial diastole At atrial diastole the muscles in the atrial wall relax and the atria increases in volume. This reduces the pressure and creates a suction force in the vena cava and other main veins that draws blood towards the heart.
The action of the leg muscles and valves in the veins When the leg muscles contract to move the legs the contractions squeeze the veins in the legs, pushing the blood upwards. Valves in the legs prevent the blood moving downwards.
7 Graph showing pressure changes in the blood vessels
SUMMARY TABLE - FEATURES OF BLOOD VESSELS
ARTERIES CAPPILARIES VEINS STRUCTURE OF THE WALL
THICKNESS OF THE WALL
DIRECTION OF BLOOD FLOW
PRESSURE
TOTAL CROSS SECTIONAL AREA CARBON DIOXIDE CONTENT OXYGEN CONTENT
PERMEABILITY
8 EXCHANGE OF MATERIALS
Many materials are exchanged between the body tissues and the blood.
MATERIAL DESCRIPTION SOURCE TRANSPORTED TO AMINO ACIDS
MONO- SACCHARIDES WATER
CARBON DIOXIDE OXYGEN
UREA
MINERAL IONS
HORMONES
TRANSPORT OF OXYGEN AND CARBON DIOXIDE IN THE BLOOD
Components of Blood Blood is made up of the following components
Plasma
Water
Red Blood Cells
White Blood Cells
Platelets
9 TRANSPORTING OXYGEN
Oxygen is transported by the blood in two ways
By the plasma (dissolved oxygen) however oxygen is quite insoluble so little oxygen is transported in this way.
By the red blood cells
Structure of the Red Blood Cell
Adaptations of the red blood cell for carrying oxygen
1. Surface area
2. No nucleus
3. Haemoglobin
Haemoglobin transports oxygen around the blood. It is this that gives red blood cells their colour. Haemoglobin contains proteins and an iron containing haem group. This haem group can bind reversibly to four oxygen molecules. There are up to 250 million haem molecules per red blood cell, therefore each red blood cell can carry up to 100 million molecules of oxygen.
In oxygen rich situations (such as at the lungs) haemoglobin can bind with oxygen to form oxyheamoglobin. In oxygen poor situations (such as at the tissues ) oxyhaemoglobin dissociates (splits up and releases the oxygen). These reactions can be summarised as
10 Oxygen Dissociation Curve
To understand why haemoglobin is an efficient molecule for transporting oxygen we need to consider the oxygen dissociation curve.
The percentage of haemoglobin molecules that combine with oxygen to from oxyhaemogloin varies with the external concentration (or partial pressure)of oxygen.
At high oxygen levels such as in the lungs haemoglobin readily binds with oxygen. Even if the oxygen level starts to fall haemoglobin still combines with oxygen meaning that the blood that leaves the lungs is almost always completely saturated with oxygen.
At lower concentrations of oxygen, the affinity of haemoglobin for oxygen falls steeply. The oxyhaemoglobin dissociates from oxygen when oxygen levels are low such as at the tissues. The steepness of the curve on the dissociation curve means that a slight fall in oxygen concentration in the tissues produces a large increase in the rate of oxyhaemoglobin breakdown. This delivers oxygen quickly and efficiently to the tissues that need it.
Haemoglobin has an S shaped dissociation curve which means that it becomes fully saturated with oxygen in the lungs but readily gives up the oxygen to respiring tissues.
11 The Bohr Effect
The efficiency of oxygen dissociation at the tissues is further enhanced by the Bohr Effect. At high carbon dioxide concentrations such as those which occur in the tissues, the dissociation curve shifts to the right. This is called the Bohr Effect. This shift means that oxyhaemoglobin gives up its oxygen even more readily at actively respiring tissues.
Foetal haemoglobin Foetal haemoglobin must have a higher affinity for oxygen than adult haemoglobin, as the foetus needs to take oxygen directly from the mothers’ blood. The dissociation curve for foetal haemoglobin is shifted to the left of adult haemoglobin.
Living in Anaerobic conditions Organisms such as Tubifex worms (which live in the mud at the bottom of lakes and rivers) have oxygen dissociation curves which are shifted to the left compared with human dissociation curves.
12 TRANSPORT OF CARBON DIOXIDE
Carbon dioxide is carried in two ways by the blood
By the plasma – carbon dioxide is much more soluble than oxygen so 5% of the carbon dioxide produced by the tissues is transported in solution in the plasma. Some of the carbon dioxide in the plasma is converted into carbonic acid which then dissociates to form hydrogen ions and hydrogen carbonate ions
SUMMARY
CO + H O H CO H + HCO
This reaction occurs very slowly.
By the red blood cells The red blood cells also carry carbon dioxide. The above reaction also occurs in the red blood cells but the rate of the reaction is increased by the presence of the enzyme carbonic anhydrase.
SUMMARY CARBONIC ANHYDRASE CO + H O H CO H + HCO
The hydrogen carbonate ions produced in the red blood cell diffuse into the plasma down a concentration gradient. This should result in an excess of positively charged ions inside the red blood cells and an excess of negatively charged ions in the plasma. This would change the pH of the blood and so is prevented by the simultaneous movement of negativelty charged chloride ions from the plasma into the red blood cell. This is called the chloride shift It keeps the red cells and plasma electrically neutral.
When carbon dioxide reacts with the haemoglobin it is called carboxyhaemoglobin.
At the lungs a reverse series of reactions occurs and carbon dioxide is breathed out.
13 SUMMARY
Haemoglobin is also very important in buffering the blood. This means keeping the pH of the blood constant by taking up any excess hydrogen ions preventing the blood from becoming too acidic.
EXCHANGE OF OTHER SUBSTANCES
Exchange of other materials occurs between the endothelial cells of the capillaries between the blood and the tissues. Water is forced out of the capillaries by the pressure of the blood, it later re-enters the capillaries by osmosis. Monosaccharides, mineral ions and waste products such as urea are exchanged between the capillaries and the tissues by facilitated diffusion.
14 TISSUE FLUID
Every cell is bathed in fluid called tissue fluid. The exchanges that occur between the blood and the cells determine the composition of the tissue fluid. Not all of the contents of the blood pass into the tissue fluid. Red blood cells, platelets and plasma proteins remain inside the blood capillaries and so the tissue fluid is composed mainly of blood plasma. The materials which are dissolved in this blood plasma depend on the position of the tissue fluid in the body e.g. tissue fluid surrounding the cells of the small intestine contain a high concentration of monosaccharides and amino acids for the few hours following a meal. Tissue fluid also contains some white blood cells which squeeze through gaps between endothelial cells (fenestrations). These white cells help to combat infection by ingesting microbes and producing antibodies.
Tissue fluid is formed when water is forced out of capillaries by hydrostatic pressure. This is the pressure which is generated by the pumping force of the heart. Water is forced out of the capillaries at the arterial end. There is a net movement of water into the tissues. However the protein molecules which are too large to leave the capillary remain in the blood making the water potential inside the capillary very negative. At the venous end of the capillary the water potential has become so negative that the tendency for water to move into the capillary by osmosis is greater than the hydrostatic pressure (which has reduced due to loss of water from the capillary) forcing water out of the capillary. At the venous end there is a net movement of water into the capillary.
15 THE LYMPHATIC SYSTEM
The pressure differences mean that more water is forced out of the capillaries by hydrostatic pressure than is reabsorbed by osmosis. The excess water drains into small capillary like vessels called lymph capillaries. The fluid inside a lymph capillary is called lymph. It has the same composition as tissue fluid but contains more lipids as lipids diffuse into lacteals and then the lymphatic system at the small intestine. Lymph vessels form a network called the lymphatic system. The system contains lymph nodes which filter bacteria and viruses from the lymph. White blood cells at these nodes destroy the bacteria. Eventually the lymph is returned to blood at the subclavian veins.
COMPARISON OF BLOOD, TISSUE FLUID, LYMPH AND PLASMA.
contents How is it formed Blood Tissue fluid Plasma Lymph
16