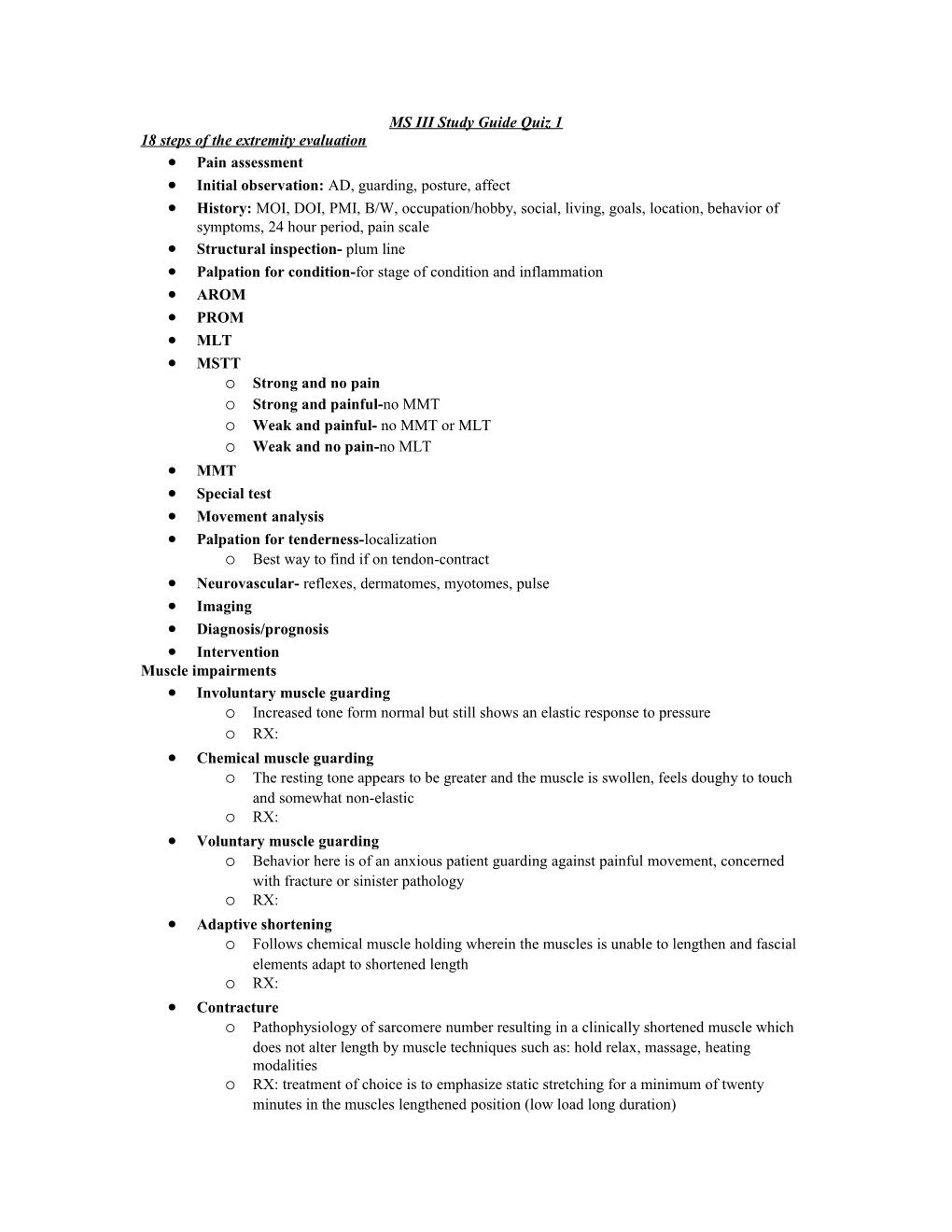
MS III Study Guide Quiz 1 18 steps of the extremity evaluation Pain assessment Initial observation: AD, guarding, posture, affect History: MOI, DOI, PMI, B/W, occupation/hobby, social, living, goals, location, behavior of symptoms, 24 hour period, pain scale Structural inspection- plum line Palpation for condition-for stage of condition and inflammation AROM PROM MLT MSTT o Strong and no pain o Strong and painful-no MMT o Weak and painful- no MMT or MLT o Weak and no pain-no MLT MMT Special test Movement analysis Palpation for tenderness-localization o Best way to find if on tendon-contract Neurovascular- reflexes, dermatomes, myotomes, pulse Imaging Diagnosis/prognosis Intervention Muscle impairments Involuntary muscle guarding o Increased tone form normal but still shows an elastic response to pressure o RX: Chemical muscle guarding o The resting tone appears to be greater and the muscle is swollen, feels doughy to touch and somewhat non-elastic o RX: Voluntary muscle guarding o Behavior here is of an anxious patient guarding against painful movement, concerned with fracture or sinister pathology o RX: Adaptive shortening o Follows chemical muscle holding wherein the muscles is unable to lengthen and fascial elements adapt to shortened length o RX: Contracture o Pathophysiology of sarcomere number resulting in a clinically shortened muscle which does not alter length by muscle techniques such as: hold relax, massage, heating modalities o RX: treatment of choice is to emphasize static stretching for a minimum of twenty minutes in the muscles lengthened position (low load long duration) Spasm o Involuntary twitch may be provoked on examination, especially a provocation such as a spring o Quick contraction with muscle spindle response Joint passive range and end feel Classical motion (active and passive) o Goniometric range o endfeel Accessory motion (component and joint play) o Directions of restriction o Normal vs. abnormal motion o End-feel o Grading of motion (0-6 scale) . 0-ankylosis . 1-considerable restriction-hypomobile (no thrust technique) . 2- slight restriction-hypomobile (can mob 1-5) . 3-normal=no mob . 4-slight increase-hypermobile (dynamic muscular control) . 5-considerable increase-hypermobile (loss of dynamic control) . 6-unstable (probably needs surgical intervention due to no dynamic control) Stage of condition immediate o the few minutes immediately post injury o first aid by the patient most effective acute o condition is worsening o goal is to limit worsening sub acute o commencing to improve o FRAGILE Settled o Stabilized o Corrective treatments are well tolerated o No signs of inflammation Chronic o At approximately 12-15 weeks primary healing is finished o Pain behaviors have developed o Patient despondent o Attorney may be involved Rate healing 50% of healing is in the first 2 weeks 80% of healing is in the first 6 weeks 100% of healing has occurred by the 12th week Stage of Reactivity: tissue high tissue reactivity- pain before tissue resistance (e.g. oscillations) moderate tissue reactivity- pain with resistance at end range (e.g. oscillate-stretch-oscillate) low tissue reactivity- no pan at resistance (e.g. stretch) Stage of reactivity: subject high subject reactivity- patient cannot carry out functional activity because of the complaints moderate subject reactivity-patient can carry out functional activity but expresses complaints during activity. Patient will most likely experience post activity complaints low reactivity-patient can carry out functional activities without complaint during the activity. Patient may or may not experience post activity complaints
Tissue injury, healing and rehabilitation Articular capsule dense irregular connective tissue- type I collagen, ground substance (proteoglycans and elastin) synovium o innermost layer of the joint capsule o also the component of bursa and tendon sheaths o histology: synoviocytes o produces synovial fluid Recurrence Rate of dislocations o Dislocations of GH joint is notorious for its high rate of recurrence o Recurrence rates have range from 47% to 100% o The pattern appears to be that patients less than 40 years old have a high rate of recurrence Adhesions o Inflammation o Fibroblast production=potential for adhesion formation o Bi-product of healing Stress-strain curve o Toe region-taking up slack o Elastic region- elongating but able to return back to original shape o Plastic region- mob III and IV for prolonged effect o Necking- will not return back to shape and good for adhesions o Failure point Ligament Made up of dense regular connective tissue Type I collagen, ground substance and elastin Grades of sprains o I- pain without laxity o II- pain with some laxity o III- no pain complete laxity Healing process (extra-articular ligaments) o Blood clot-leukocytes and lymphocytes o Inflammatory-macrophages and fibroblasts o Proliferation-fibroblasts o Remodeling and maturation-normal ratios of water and collagen Differences in healing based upon location o Intra-articular- no tissue bridging the gap between torn ends . Example-ACL o Extra-articular- fibrin clot formation, scaffold, fibroblasts, collagen fiber replacement . Example- MCL, ATF Ligament injury-interventions ROM o Joint movement is beneficial as long as force is not too high . no research on what is too much force. Differs by patient and ligament o low cyclic loads on a ligament scar promote scar proliferation and material remodeling making the scar stronger and stiffer structurally effects of cross friction on ligament healing o helps align fibers but no overall change in tensile strength Tendon made of dense regular connective tissue type I collagen, ground substance and elastin functions o transmit force generated by muscle to bone o absorbs external forces to limit muscle damage stress tolerance o good for tensile o poor for shear ad compression itis vs. Osis o itis: inflammation o Osis: degeneration o Tendinosis-the same result of failed tendon-healing . Non-inflammatory . Degenerative . Avascular Healing process-same as ligament Continuum of tendon pathology o Reactive tendinopathy . Non-inflammatory proliferative response in the cell and matrix . Short term adaptive thickening of a portion of the tendon . Clinically: acutely overload tendon usually in younger person; may occur as a result of direct trauma o Tendon disrepair . Tendon disrepair describes the attempt at tendon healing . Similar to reactive tendinopathy but with greater matrix breakdown . Clinically: chronically overloaded tendons; usually in the young o Degenerative tendinopathy . Progression of both matrix and cell changes . Areas of cell death are apparent . Clinically Usually seen in the older person Can be seen in the younger person or elite athlete with a chronically overloaded tendon If extensive enough or placed under high load, rupture is likely o 97% of tendons that rupture have this progressive degenerative change overtime Eccentric Training for tendon injuries The intensity of the exercise program can be altered by load and speed of contraction Remember the force velocity curve Treatment with painful eccentric quadriceps training, but not with painful concentric quadriceps training significantly reduced tendon pain during activity and improved function in athletes with chronic painful jumper’s knee No change in symptoms with eccentric exercise performed during the competitive season Surgery vs. eccentric exercise- no sx until failed eccentric work Transverse friction massage the lesion must be brought within reach of the operator’s finger the tissue to receive the massage should be appropriately tensioned o muscle-relaxed o tendon without sheath-most accessible position o tendon with sheath-taut o ligament-performed along tendon at end of each available ROM . ex: MCL needs to be massaged in flexion and extension treatment is applied by the operator’s fingertip the technique is to move the entire hand with the patient’s skin and the operators finger moving as one In general the finger, hand, and forearm should comprise a straight line parallel to the movement imparted
Subjective Examination Go over history and interview questions Maitland article o Parallel questioning- ask questions that builds on conversation so patient flow continues o Keying- hone in on keywords so that you can address them appropriately o Biasing-know its place in conversations . Positive- do you feel that the last two treatments have helped you? . Neutral- has t here been any change in your symptoms as result of the last two treatments? . Negative- have the last two treatments made you worse in any way? o Immediate response-spontaneous questions to build onto commentary o Types of communication . Verbal – choice of words, the way these words are said, tone Use words in the same way the patient uses them Assume nothing Avoid asking two questions in one sentence The question should be as short as possible pausing . Non verbal- facial expressions, body language Raised eyebrow Tilt of head Frown Crossed arm o Errors in communication . Don’t repeat the same question . Apologize and rephrase Types of intervention o Direct intervention . Therapeutic exercise . Functional training in self care and home management . Functional training in community and work . Manual therapy techniques . Electrotherapeutic modalities . Physical agents and mechanical modalities o Patient/client related instruction . Written, pictorial, and or video instruction o Coordination, communication, documentation . Coordination/communication with patient, family, caregivers and other health care professionals . Documentation as required by the state practice act Decision making reference Physiological Normal EF Abnormal EF Normal physiological No RX Swelling, adhesion, ROM cartilage, laxity, muscle Abnormal physiological Muscle, laxity, bone All 9 end feels ROM Physiological motion Normal accessory Abnormal accessory Normal physiological No RX Laxity, cartilage, ROM adhesion, effusion Abnormal physiological Edema, muscle, bone All 8 but muscle ROM MS study guide quiz #2 Required reading:Cook, JL is tendon pathology a continuum? Continuum of tendon pathology o Reactive tendinopathy . Non-inflammatory proliferative response in the cell and matrix . Short term adaptive thickening of a portion of the tendon . Clinically: acutely overload tendon usually in younger person; may occur as a result of direct trauma o Tendon disrepair . Tendon disrepair describes the attempt at tendon healing . Similar to reactive tendinopathy but with greater matrix breakdown . Clinically: chronically overloaded tendons; usually in the young o Degenerative tendinopathy . Progression of both matrix and cell changes . Areas of cell death are apparent . Clinically Usually seen in the older person Can be seen in the younger person or elite athlete with a chronically overloaded tendon If extensive enough or placed under high load, rupture is likely o 97% of tendons that rupture have this progressive degenerative change overtime
Eccentric Training for tendon injuries The intensity of the exercise program can be altered by load and speed of contraction Remember the force velocity curve Treatment with painful eccentric quadriceps training, but not with painful concentric quadriceps training significantly reduced tendon pain during activity and improved function in athletes with chronic painful jumper’s knee No change in symptoms with eccentric exercise performed during the competitive season Surgery vs. eccentric exercise- no sx until failed eccentric work Transverse friction massage the lesion must be brought within reach of the operator’s finger the tissue to receive the massage should be appropriately tensioned o muscle-relaxed o tendon without sheath-most accessible position o tendon with sheath-taut o ligament-performed along tendon at end of each available ROM . ex: MCL needs to be massaged in flexion and extension treatment is applied by the operator’s fingertip the technique is to move the entire hand with the patient’s skin and the operators finger moving as one In general the finger, hand, and forearm should comprise a straight line parallel to the movement imparted
Red flags for potential serious conditions in patients with ankle/foot problems Fractures o Ottowa Ankle Rules: . Must have pain along 4 aspects: Either malleoli distal posterior aspect 6cm Navicular Base of 5th met . Must have pain with WB 3 steps . Exceptions-alteration in sensation or cognition (i.e. drugs, dementia, TBI, CVA) o Fracture types . Jone’s fracture Located along the base of the 5th metatarsal along base diaphysis Due to PF/INV or spinning action Worried about peroneus brevis avulsion fracture . Dancer’s fracture Same location as Jone’s with involvement into the intermedullary space Correlated with avulsion fracture due to enhanced proprioceptive moment and decrease BOS (quick dancer training) Common in ballerina’s because they are on point and they spin at the same time . March fracture Along 2nd and 3rd metatarsal Common in military from poor shoeware and no shock absorption Usually starts out as a stress fracture and progresses into fracture . Lisfranc fracture mid tarsal fx cuneiform and base of metatarsals common in binding sports and pivoting activities location of fracture is poorly vascularized surgical intervention-NWB 8-12 weeks treatment o need op report . Treatment for fractures Look at kinetic chain (gluts, hamstrings, quads, lower leg) Decreased inflammation and swelling mobilize DVT o DVT and its sequel pulmonary embolism are the leading causes of preventable in- hospital mortality in the US o Existing data that underestimate the true incidence of DVT suggest that about 80 cases per 100k persons occur annually o About 600k hospitalizations per year occur for DVT in the US o Death from DVT is attributed to massive PE, which causes 200k deaths annually in the US, PE is the leading cause of preventable in-hospital mortality o DVT Well’s Score . Clinical feature Active cancer, Paralysis recently bedridden or surgery localized tenderness along deep venous system entire leg swollen calf swelling at least 3 cm larger than asymptomatic side pitting edema confined to symptomatic leg collateral superficial veins previously documented DVT an alternative dx is at least as likely as DVT=-2 scored: 2 points or more is likely DVT (~28% accuracy) . symptoms included: uncomfortable regardless of position tightness redness and swelling antalgic gait night pain Compartment syndrome o A condition in which increased pressure within a limited space compromises the circulation and function of the tissues within that space o Multi causal but most common in fractures o Due to external or internal restriction o Elevated tissue pressure within a closed fascial space . Reduces tissue perfusion-ischemia . Results in cell death-necrosis o Etiology . Compartment size Tight dressing; bandage/cast Localized external pressure; lying on limb Closure of fascial defects . Compartment content Bleeding; fx vas inj, bleeding disorders Capillary permeability: ischemia, trauma, burns, exercise, snake bite, drug injection o Tissue survival . Muscle 3-4 hours-reversible changes 6 hours-variable damage 8 hour-irreversible changes . Nerve 2 hours-looses nerve conduction 4 hours-neuropraxia 8 hours-irreversible changes o diagnosis: 16 gauge needle to evaluate pressure . standard:>20mmHg =surgery . study: >30mmHg= surgery; <30mmHg monitor o symptoms . exertional- pain with exertion that goes away with rest or as inflammation decreases common in deep posterior compartment . acute-usually due to direct trauma common in lateral or anterior lateral compartment o non surgical treatment: . elevation . diuretic . anti-inflammatory Diabetic neuropathy o DN has 4 categories but most common is peripheral neuropathy o diabetes is a gateway disease o pathophysiology . increase in glucose that changes structure on proteins and decreases capacity for tissues to maintain structure= decrease in function and increase in likelihood of failure . affects nerves o Signs and symptoms . Difficulty differentiating temperature or pain . Loss of balance . Loss of sensation o Intervention strategies . Improve balance of proximal structures and their firing strategies . Patient education on checking feet and shoes . Get eye exam every year as preventative Ankle 5/20/15 Rearfoot-consists of the talocural and subtalar joint Midtarsals-lazy joint and goes to position of ease (usually pronation) Moves in the same direction of the rearfoot Excessive pronation=can cause potential problem Study: runners all ran in neutral shoe found to have more injuries in those that were more supinated than those that were more pronated in the midfoot Forefoot- moves in the opposite direction as rearfoot and midtarsals Normal motion of the foot IC- hindfoot/midfoot=pronation; forefoot=supination LR- hindfoot/midfoot=pronation; forefoot=supination HO- hindfoot/midfoot=supination; forefoot=pronation Anatomy Talus o Wider more anteriorly than posteriorly (inverted triangle) o DF has greatest functional deficit-limited ROM in DF than in PF o More injuries happen in PF Navicular o Location for anterior tib and posterior tib Base of the 5th- - peroneus brevis attachment and location for possible fractures Sustenaculum talus- mainly vascularized structure Sesmoids-embedded in FHL o Leverage points to allow for greater force production o Inju bries include sesmoiditis and stress fractures Talocural joint o 1 mm shift of the talus could cause focal distribution and increase breakdown on the articular surface leading to increase degeneration . leads to surgical intervention fusion o mobilizations to this area will stretch the syndesmosis, ATF, and PTF o High ankle sprain . MOI- forced DF with pivot in any direction o Inversion ankle sprain . The fibula can move inferiorly and anteriorly due to laxity in the ATF ligament . Treatment Mobilization of fibula posteriorly and have patient DF to see if their symptoms and ROM improves Mulligan tape job Address eversion o Patients that lack eversion control will fall in opposite direction during SLS o Peroneus brevis is the strongest evertor o Peroneus longus attaches at the base of the 1st MTP and controls forefoot; supports medial longitudinal arch Proprioception- spatial awareness during gait so don't have to look at feet Strengthen gluteus maximus and hamstrings o Patients with chronic ankle sprains upon MMT of the glut and hamstring have weakness on ipsilateral side o Neural pattern? o Mechanical? . Assessment of the talocural joint Anterior drawer 2mm difference o performed better with gastrocnemius on stretch o you would feel minimal movement Talor tilt-invert it not o specific but you would be able to see drastic movement subtalar joint o very tight and stubborn joint o calcaneus is concave and convex Kinetic Chain Impact need to look at the foot when evaluating for SI, hip, lumbar, knee, and foot pathology hindfoot/midfoot-pronation; tibia- IR; knee- valgus; hip-IR hindfoot/midfoot-supination; tibia- ER; knee- varus; hip-ER
5/22/15 lecture ankle/foot continued… Best exam step for Ankle Sprain P4C, PROM Accessory, P4T Interventions o Address intrinsics sitting and WB o BAPS board provides great biofeedback Need to evaluate CAM angle Important for runners; are they running in the same direction? need to know where they run and when they have pain beach along the wet sand has a 10-15% angle L LE on incline= cause pronation at the hindfoot, tibia IR, knee valgus and flexion, limb will be shortened R LE=cause supination at the hindfoot, tibia ER, knee varus and extension, limb will be extended Possible treatment for structural alignment Treatment for calcaneal eversion- place felt on medial aspect of hindfoot to bring them into more supination and to help with structural alignment Treatment for midfoot drop-want to place pad under navicular Compensations for the midtarsal joint Rigid hindfoot o Midfoot will be more hypermobile and have increase in pronation o Will look like they have relatively flat feet Plantar fasciitis-assess calcaneus for excessive supination to take off pressure of navicular Rigid midfoot o Will lead to talocural laxity (hindfoot) with talus medial and posterior glide Forefoot Posterior tibialis- has 7 attachments o Inferior navicular tubercle o Met heads 2-4 o All 3 cuneiforms Peroneus longus- 1st ray met head attachment Posterior tibialis tendinopathy o More common in female than male due to wider hips and valgus at the knee that drive down onto foot o Common in late 40-60s post menopausal o Progressive dysfunction . Tenosynovitis without deformity . Tenosynovitis with functional deformity . Structural deformity-dysfunction o Study . Stage 1- normal mobility and length of tendon Management o NSAIDs o Refer for orthoses . Stage 2-foot breaks down and more mobility and elongation of the tendon Management o Refer for appropriate orthoses or ortho referral o Surgery if conservative treatment fails . Stage 3- foot becomes rigid and tendon becomes elongated and actively insufficient Management o Trail of appropriate orthoses or ortho referral o Fusion if fails . Everyone on conservative treatment program improved, but eccentrics made more improvements o Treatments: . gastroc/soleus stretch . mobilizations . orthosis Achilles tendon Gastrocnemius and soleus contribute separately to the formation of the tendon The tendon twists as it descends The gastrocnemius usually makes up the more lateral and posterior portion of the tendon Some authors believe that the twist creates a watershed area (wringing out a towel) of hypovascularity 2-6 cm above the tendons insertion First MTP joint 80-85 degrees of extension needed for running 60-65 degrees of extension needed for walking windlass effect- the effect of the plantar fascia as the first MTP goes into extension to create inversion and elevation (heel raise) o must have these things for efficient windlass effect . equal height . WB through MTP . Calcaneal inversion . Arch elevates (MLA) o Why does the calcaneus invert? PF tensions and pulls on medial tubercle of calcaneus . If patient doesn't bear weight on first MTP then calcaneus will not invert o Why WB on first MTP? . Peroneus longus attaches there and should done MTP into ground . Starts windlass effect-pre tensions the plantar fascia Plantar fasciitis- decrease in windlass effect o Quadratus plantae sticks to PF o Could be due to bone spurs- treatment is surgeons chipping off the spur instead of removing it Metatarsalgia-diffused pain along the metatarsals along 2-4 Interdigital nerve entrapment- due to entrapment in transverse metatarsal ligament Sensory only nerve so patients will complain of pain WB in toe extension causes pain Localized Morton’s neuroma Ganglion cyst Patient will complain of compression Most likely will need surgical intervention Treatment: evaluate shoe if they have a negative heel that can cause more extension in toes Tarsal tunnel Posterior tib nerve entrapment o Causes . Navicular drop . Calcaneus everted . Tight retinaculum . Tenosynovitis . Lancinate ligament . Edema . Vascular insufficiencies o Patient will have patient with eversion of the foot that subsides with inversion o Treatment: fascial techniques o Differential diagnosis: neurovascular