BIOII CH15 PowerPoint Lecture Outlines NAME______
Myocardial Thickness and Function The thickness of the myocardium of the four chambers varies according to the function of each chamber. The ATRIAL walls are thin because they deliver blood to the ventricles. The ventricle walls are thicker because they pump blood greater distances The right ventricle walls are thinner than the left because they pump blood into the ______which are nearby and offer very little resistance to blood flow. The left ventricle walls are thicker because they pump blood through the body where the resistance to blood flow is greater.
Location of Heart posterior to sternum base lies beneath 2nd rib at 5th intercostal space medial to lungs lies upon ______anterior to vertebral column
Coverings of Heart The connective tissue covering he heart is called the ______Which is a serous membrane Wall of the Heart Describe Function and Location****** Epicardium: Myocardium: Endocardium:
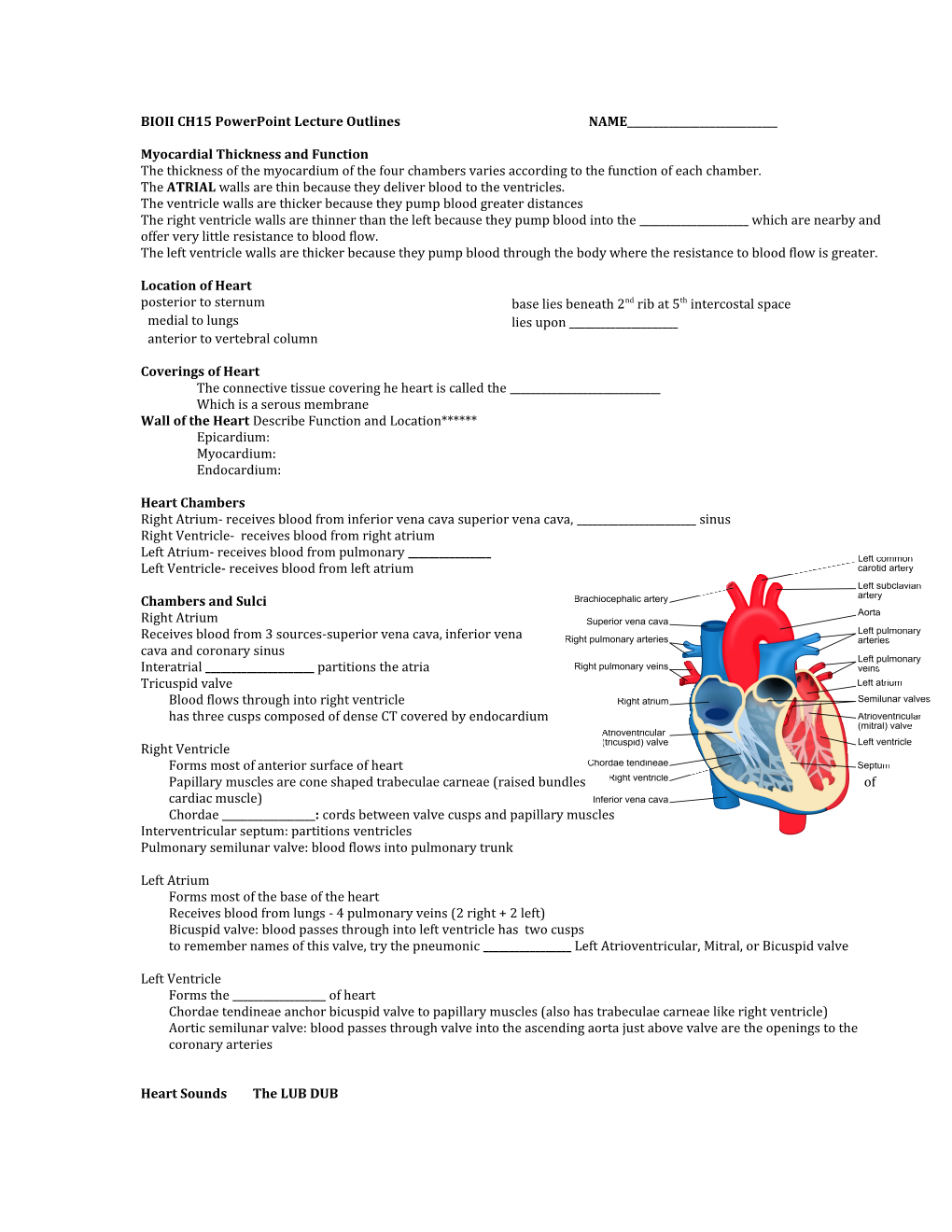
Heart Chambers Right Atrium- receives blood from inferior vena cava superior vena cava, ______sinus Right Ventricle- receives blood from right atrium Left Atrium- receives blood from pulmonary ______Left Ventricle- receives blood from left atrium
Chambers and Sulci Right Atrium Receives blood from 3 sources-superior vena cava, inferior vena cava and coronary sinus Interatrial ______partitions the atria Tricuspid valve Blood flows through into right ventricle has three cusps composed of dense CT covered by endocardium
Right Ventricle Forms most of anterior surface of heart Papillary muscles are cone shaped trabeculae carneae (raised bundles of cardiac muscle) Chordae ______: cords between valve cusps and papillary muscles Interventricular septum: partitions ventricles Pulmonary semilunar valve: blood flows into pulmonary trunk
Left Atrium Forms most of the base of the heart Receives blood from lungs - 4 pulmonary veins (2 right + 2 left) Bicuspid valve: blood passes through into left ventricle has two cusps to remember names of this valve, try the pneumonic ______Left Atrioventricular, Mitral, or Bicuspid valve
Left Ventricle Forms the ______of heart Chordae tendineae anchor bicuspid valve to papillary muscles (also has trabeculae carneae like right ventricle) Aortic semilunar valve: blood passes through valve into the ascending aorta just above valve are the openings to the coronary arteries
Heart Sounds The LUB DUB Heart Valves Atrioventricular Valves Open A-V valves open and allow blood to flow from atria into ventricles when ventricular pressure is lower than atrial pressure Occurs when ventricles are relaxed, chordae tendineae are slack and papillary muscles are relaxed Atrioventricular Valves Close THE LUB A-V valves ______preventing backflow of blood into atria Occurs when ventricles contract, pushing valve cusps closed, chordae tendinae are pulled taut and papillary muscles contract to pull cords and prevent cusps from everting Semilunar Valves THE DUB SL valves open with ventricular contraction allow blood to flow into pulmonary trunk and aorta ______valves close with ventricular relaxation prevents blood from returning to ventricles, blood fills valve cusps, tightly closing the SL valves
Valve Function Review Fibrous Skeleton of Heart Dense CT rings surround the valves of the heart, fuse and merge with the interventricular septum Support structure for heart ______Insertion point for cardiac muscle bundles Electrical insulator between atria and ventricles prevents direct propagation of AP’s to ventricles
Path of Blood Through the Heart
Blood Supply to Heart
Cardiac Cycle Atrial Systole/Ventricular Diastole ______% blood flows passively into ventricles remaining 30% of blood pushed into ventricles A-V valves open/semilunar valves close ventricles relaxed ventricular pressure increases
Cardiac Muscle Fibers 1. A functional ______is a mass of merging cells that act as a unit. 2. Two syncytiums of the heart are in the atrial walls and the ventricular walls. 3. The atrial syncytium and ventricular syncytium are connected by fibers of the cardiac conduction system. Cardiac muscle cells -are joined end to end by ______discs which allow for depolarization to spread Cardiac muscle fibers swirl diagonally around the heart in interlacing bundles
Cardiac Conduction System The cardiac conduction system is responsible for coordinating events of the cardiac cycle. The S-A ______node is in the wall of the right atrium, AKA called the pacemaker because it generates the heart’s rhythmic contractions. As a cardiac impulse travels from the S-A node into the atrial syncytium, it goes from cell to cell via gap junctions. Conducting fibers deliver impulses from the S-A node to the A-V node. The A-V ______node is in the inferior interatrial septum and provides the normal conduction path between the atrial and ventricular syncytiums. From the A-V node, impulses pass to the A-V bundle in the interventricular septum and gives rise to bundle branches. ______fibers carry impulses to distant regions of the ventricular myocardium. The ventricular walls contract with a twisting motion because the muscle fibers in the walls form irregular whorls. Contraction of the ventricles begins at the apex of the heart and pushes blood superiorly toward the aortic and pulmonary semilunar valve.
Electrocardiogram EKG-ECG Electrocardiogram Impulse conduction through the heart generates electrical currents that can be detected at the surface of the body. The ECG helps to determine if the conduction pathway is abnormal, if the heart is enlarged, and if certain regions are damaged.
EKG Action potentials of all active cells can be detected and recorded P wave- ______depolarization P to Q interval -conduction time from atrial to ventricular excitation QRS complex - ventricular ______T wave - ventricular repolarization
ECG In a typical ECG ______waves accompany each heartbeat: P wave (atrial depolarization - spread of impulse from SA node over atria) QRS complex (ventricular depolarization - spread of through ventricles) T wave (ventricular repolarization). Regulation of Cardiac Cycle CARDIAC OUTPUT Cardiac output (CO) is the volume of blood ejected from the left ventricle into the ______each minute. Cardiac output equals the stroke volume, the volume of blood ejected by the ventricle with each contraction, multiplied by the heart rate, the number of beats per minute. CO = SV X HR Cardiac Output CO = SV x HR at 70ml stroke volume & 75 beat/min----5 and 1/4 liters/min entire blood supply passes through circulatory system every minute Cardiac reserve is maximum output/output at rest - average is 4-5x while athlete’s is 7-8x
Influences on Stroke Volume Preload: Effect of Stretching - According to the Frank-Starling law of the heart, a greater preload (______) on cardiac muscle fibers just before they contract increases their force of contraction during systole. Contractility Myocardial contractility, the strength of contraction at any given preload, is affected by positive and negative inotropic agents. Afterload The pressure that must be overcome before a semilunar valve can open is the afterload.
Congestive Heart Failure - blood remains in the ventricles increasing the preload and causing an overstretching of the heart and less forceful contraction Left ventricular failure results in pulmonary ______Right ventricular failure results in peripheral edema.
Chemical regulation of heart rate Heart rate affected by hormones (epinephrine, norepinephrine, thyroid hormones). ______(Na+, K+, Ca+2) also affect heart rate. Other factors such as age, gender, physical fitness, and temperature also affect heart rate.
Arteries and Arterioles Artery ______strong wall, endothelial lining middle layer of ______muscle and elastic tissue outer layer of connective tissue carries blood under relatively high pressure
Arterioles thinner wall than artery endothelial lining some smooth muscle tissue small amount of connective tissue helps control blood flow into a ______smallest arterioles have few smooth muscle fibers capillaries lack muscle fibers
Capillaries smallest ______blood vessels extensions of inner lining of arterioles walls are endothelium only semipermeable sinusoids – leaky capillaries
Exchange in the Capillaries ______and other substances leave capillaries because of net outward pressure at the capillaries’ arteriolar ends water enters capillaries’ venular ends because of a net inward pressure substances move in and out along the length of the capillaries according to their respective concentration gradients
Venules and Veins ATERY vs. VEIN ______wall than arteriole less smooth muscle and elastic tissue than arteriole
Vein thinner wall than artery three layers to wall but middle layer is poorly developed some have ______valves carries blood under relatively low pressure serves as blood reservoir
Venous Valves –valves in veins prevent blood from falling back down the body during diastole, valves damaged can lead to varicose veins
Blood Pressure Blood pressure is the force the blood exerts against the inner walls of the blood vessels, most commonly refers to pressure in ______. Arterial Blood Pressure Systolic pressure is the maximum pressure and is created when the ventricles contract. Diastolic pressure is the minimum pressure and is created when the ventricles relax. A pulse is the alternate expanding and recoiling of an arterial wall.
Factors that Influence Arterial Blood Pressure Heart Action Stroke volume Cardiac output Blood Volume Peripheral Resistance Viscosity
Control of Blood Pressure -Factors affecting stoke volume and heart rate are mechanical, neural, and chemical. If blood pressure rises, baroreceptors initiate the cardioinhibitory reflex which decreases blood pressure. If blood pressure falls, the cardioaccelerator reflex occurs which increases ______stimulation to the heart, which ______heart rate and cardiac output, which increases blood pressure. Other factors that increase HR and BP are emotional responses, exercise, and a rise in body temperature. When arterial blood pressure suddenly increases, baroreceptors signal the vasomotor center, and ______sympathetic outflow to arterial walls, which results in a decrease in blood pressure. Chemicals that influence peripheral resistance are carbon dioxide, oxygen, and hydrogen ions.
Central Venous Pressure Central venous pressure is the pressure within the heart. Central venous pressure is of special interest because it affects the pressure within the peripheral veins. An increase in central venous pressure can lead to peripheral ______.
Blood Flow Through Alveoli cells of alveolar wall are tightly joined together the high osmotic pressure of the interstitial fluid draws water out of them Life-Span Changes cholesterol deposition in blood vessels increase in adipose tissue of the heart heart enlargement ______in blood pressure death of cardiac muscle cells decrease in resting heart rate increase in fibrous connective tissue of the heart
Clinical Problems MI = myocardial infarction use clot dissolving drugs streptokinase or t-PA & HEPARIN
death of area of heart muscle from lack of O2 balloon angioplasty replaced with scar tissue Angina pectoris-heart pain from ischemia of results depend on size & location of damage cardiac muscle Blood clot
CAD Coronary artery disease CAD is a condition in which the heart muscle receives an inadequate amount of blood due to obstruction of its blood supply. It is the leading cause of death in the United States each year. The principal causes of obstruction include ______, coronary artery spasm, or a clot in a coronary artery. Risk factors for development of CAD include high blood cholesterol levels, high blood pressure, cigarette smoking, obesity, diabetes, “type A” personality, and sedentary lifestyle.
Atherosclerosis is a process in which smooth muscle cells proliferate and fatty substances, especially cholesterol and triglycerides accumulate in the walls of the medium and large arteries in response to stimuli, such as endothelial damage Diagnosis of CAD includes such procedures as cardiac catheterization and cardiac angiography. Treatment options for CAD include drugs and coronary artery ______grafting, and stents
Risk factors in heart disease: high blood cholesterol level Other factors include: high blood pressure diabetes mellitus cigarette smoking genetic predisposition obesity & lack of regular exercise. male gender high blood levels of fibrinogen left ventricular hypertrophy Plasma Lipids and Heart Disease Risk factor for developing heart disease is high blood cholesterol level. promotes growth of fatty plaques very low-density lipoproteins (VLDLs) Most lipids are transported as lipoproteins ______remove excess cholesterol from circulation low-density lipoproteins (LDLs) LDLs are associated with the formation of fatty plaques high-density lipoproteins (HDLs) VLDLs contribute to increased fatty plaque formation
There are two sources of cholesterol in the body: in foods we ingest & formed by liver Desirable Levels of Blood Cholesterol for Adults TC (total cholesterol) under 200 mg/dl LDL under 130 mg/dl HDL over 40 mg/dl Normally, triglycerides are in the range of 10-190 mg/dl. Among the therapies used to reduce blood cholesterol level are exercise, diet, and ______DRUGS.