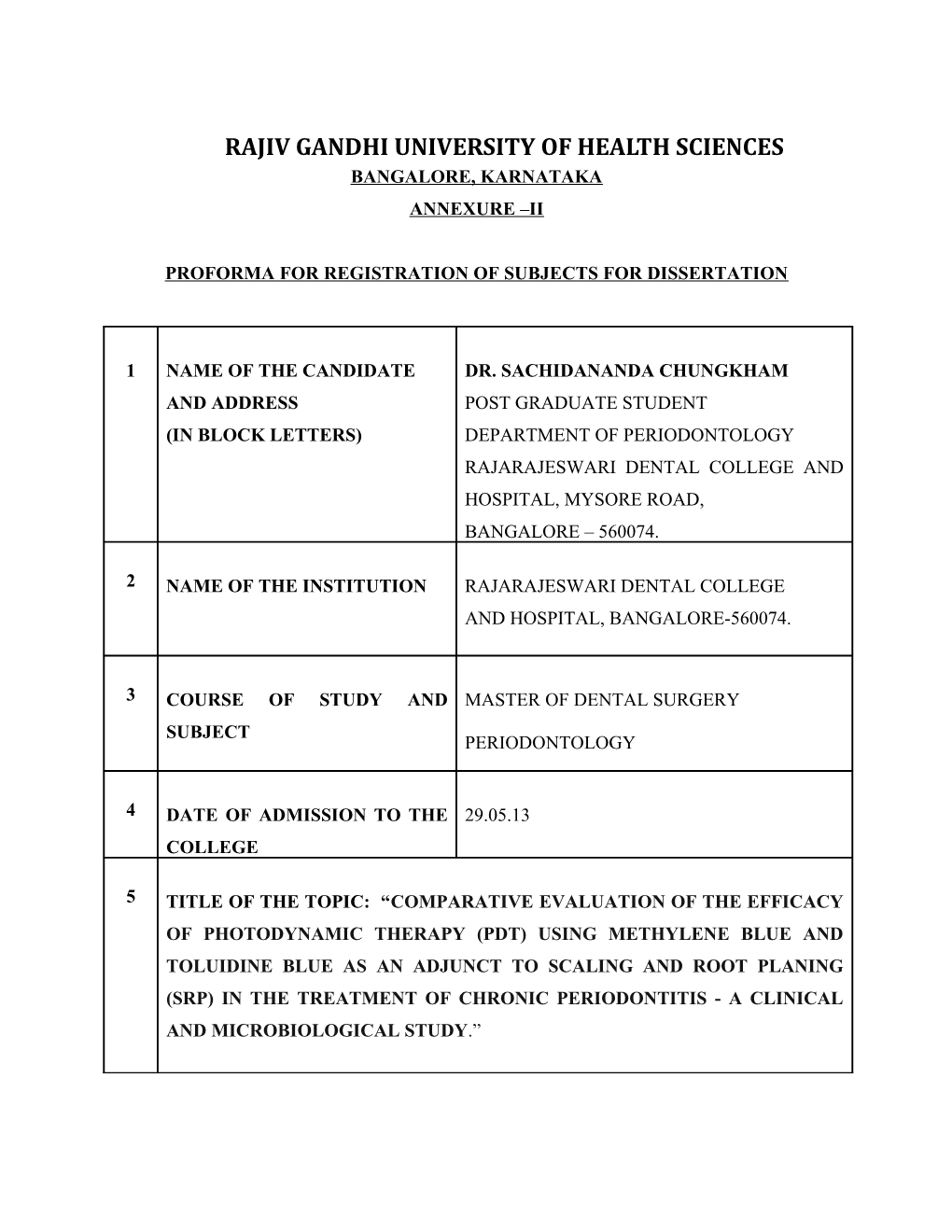
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES BANGALORE, KARNATAKA ANNEXURE –II
PROFORMA FOR REGISTRATION OF SUBJECTS FOR DISSERTATION
1 NAME OF THE CANDIDATE DR. SACHIDANANDA CHUNGKHAM AND ADDRESS POST GRADUATE STUDENT (IN BLOCK LETTERS) DEPARTMENT OF PERIODONTOLOGY RAJARAJESWARI DENTAL COLLEGE AND HOSPITAL, MYSORE ROAD, BANGALORE – 560074.
2 NAME OF THE INSTITUTION RAJARAJESWARI DENTAL COLLEGE AND HOSPITAL, BANGALORE-560074.
3 COURSE OF STUDY AND MASTER OF DENTAL SURGERY SUBJECT PERIODONTOLOGY
4 DATE OF ADMISSION TO THE 29.05.13 COLLEGE
5 TITLE OF THE TOPIC: “COMPARATIVE EVALUATION OF THE EFFICACY OF PHOTODYNAMIC THERAPY (PDT) USING METHYLENE BLUE AND TOLUIDINE BLUE AS AN ADJUNCT TO SCALING AND ROOT PLANING (SRP) IN THE TREATMENT OF CHRONIC PERIODONTITIS - A CLINICAL AND MICROBIOLOGICAL STUDY.” 6 BRIEF RESUME OF THE INTENDED WORK:
6.1 NEED FOR THE STUDY :
Periodontitis is a chronic inflammatory disease involving the supporting structures of
the teeth. It is triggered by periodontopathogens, while the clinical outcome is greatly
influenced by the local host immune response.1 The main approach to treat periodontitis
involves the removal of plaque biofilm by means of mechanical debridement (i.e. non-
surgical periodontal therapy). Although, in most cases, non-surgical periodontal therapy
results in significant clinical improvements, complete removal of bacterial deposits is still
very difficult to be accomplished. In order to additionally facilitate bacterial reduction,
especially in cases that do not adequately respond to conventional mechanical treatment,
complementary methods such as systemic and local antibiotics or various laser systems have
been proposed.2
In recent years, the combination of laser light and photosensitizer known as
photodynamic therapy (PDT) has been used in periodontal therapy.3
Photodynamic therapy (PDT) can be defined as eradication of target cells by reactive
oxygen species produced by means of a photosensitizing compound and light of an
appropriate wavelength. Photodynamic action describes a process in which light, after being
absorbed by dyes, sensitizes organisms for visible light induced cell damage.4
In photodynamic therapy, the particular photosensitizers employed are phenothiazine
dyes (Toluidine blue O, Methylene blue), erythrosine, chlorine e6 and hematoporphyrin,
which have been shown to be safe when employed in the medical field. The phenothiazine
dyes (Toluidine blue O and Methylene blue) are the major photosensitizers applied clinically in the medical field.5
The photosensitizer acts as an agent of optical absorption or chromophore, which produces fluorescence after irradiation, causing cytotoxicity in the medium.6
Various in vitro studies have shown the use of a laser associated to a photosensitizer is very efficient against bacteria, yeasts, viruses and parasites.7 It has been demonstrated that photosensitizers, such as toluidine blue O and methylene blue, which undergo a pronounced cationic charge, can bind to the outer membrane of gram-negative bacteria and penetrate bacterial cells, demonstrating a high degree of selectivity for killing microorganisms compared with host mammalian cells.8 Therefore, toluidine blue O and methylene blue have been the photosensitizers of choice in the treatment of periodontitis . However, toluidine blue
O seems to exhibit a greater ability for killing gram-positive and gram-negative bacteria than methylene blue.5
According to our knowledge, there are no studies comparing the effects of photodynamic therapy using methylene blue and Toluidine blue in the treatment of chronic periodontitis. Hence the present study is aimed to assess the efficacy of photodynamic therapy (PDT) using methylene blue and Toluidine blue as an adjunct to scaling and root planing (SRP) in the treatment of periodontitis and compare the efficacy of methylene blue and Toluidine blue as photosensitizers. 6.2 REVIEW OF LITERATURE:
A study was done to compare PDT with a diode laser and the Nd: YAG. Patients are
divided into three groups. Group I received SRP and irradiation from Nd: YAG.
Group II received SRP and irradiation from a diode laser. Group III received SRP and
PDT. Microbiological samples were examined and evaluated over a period of three
months. Significant bacterial reduction has been observed in all cases. The diode laser
with SRP presented long term positive results, while PDT showed significant bacterial
reduction during the entire observation period.3
A study was done to evaluate the susceptibility of Candida Albicans to photodynamic
therapy using methylene blue and toluidine blue as photosensitizing dyes. This study
concluded that Candida Albicans was susceptible to PDT, using either methylene blue
or toluidine blue as photosensitizers and the number of Candida Albicans was lower
when Toluidine blue was used.6
Another study was done to assess the effect of adjunctive antimicrobial photodynamic
therapy in chronic periodontitis. All teeth received periodontal treatment comprising
SRP.Using a split mouth design, two quadrants (test group) were additionally treated
with PDT. Bleeding on probing (BOP), relative attachment level (RAL), probing
depth (PD) were evaluated at baseline and 3 months after treatment. This study
indicates that the adjunctive use of a PDT has a positive effect on treatment outcomes.
Thus, by adding antimicrobial photodynamic treatment procedures to conventional
anti-infective approaches, it might be possible to improve non-surgical periodontal
therapy.9 A study was done to evaluate the bactericidal efficacy of Methylene Blue and
Toluidine Blue against different bacteria under light and dark conditions to determine
the most effective bactericidal dye. This study concluded that Toluidine Blue exhibits
a greater bactericidal activity than Methylene Blue against most bacteria in dark and
light conditions. Mostly, these results are consistent with their respective dye partition
coefficients.10
Another study was done to evaluate the effects of a combination of photodynamic
therapy with low-level laser therapy as an adjunct to nonsurgical treatment
of chronic periodontitis. Patients with untreated chronic periodontitis were randomly
assigned in a split-mouth design to receive scaling and root debridement with or
without one course of adjunctive photodynamic therapy and low-level laser therapy.
This study concluded that a combined course of photodynamic therapy with low-level
laser therapy could be a beneficial adjunct to nonsurgical treatment of chronic
periodontitis on a short-term basis. Further studies are required to assess the long-term
effectiveness of the combination of photodynamic therapy with low-level laser
therapy as an adjunct in nonsurgical treatment of periodontitis.11 A study was done to compare the efficacy of photoablative and photodynamic diode
laser in adjunct to scaling and root planing (SRP) and SRP alone for the treatment of
chronic periodontitis. This study concluded that diode laser treatment (photoablation
followed by multiple photodynamic cycles) adjunctive to conventional SRP improves
healing in chronic periodontitis patients.12 6.3 AIMS AND OBJECTIVES OF THE STUDY:
1) To evaluate the efficacy of photodynamic therapy (PDT) using methylene blue and
toluidine blue as an adjunct to scaling and root planing (SRP) in the treatment of chronic
periodontitis.
2) To compare the efficacy of methylene blue and Toluidine blue as photosensitizers.
7 MATERIALS AND METHODS :
7.1 SOURCE OF DATA
Patients reporting to the Department of Periodontology, Rajarajeswari Dental College and
Hospital, Bangalore.
7.2 METHOD OF COLLECTION OF DATA :
A total of 30 patients aged between 30-50 years diagnosed as chronic generalised
periodontitis will be selected for the study, out of which 90 sites will be treated and grouped
as follows:
Group I [control group] - 30 sites will be treated with scaling and root planing.
Group II [test group] - 30 sites will be treated with scaling and root planing followed by
methylene blue mediated photodynamic therapy.
Group III [test group] - 30 sites will be treated with scaling and root planing followed by
toluidine blue mediated photodynamic therapy. INCLUSION CRITERIA :
Systemically healthy patients.
Patient should have more than 20 teeth remaining.
More than 30% of sites involved.
Presence of periodontal pocket in at least two teeth with a probing depth of >5 mm in
each quadrant.
EXCLUSION CRITERIA :
Smokers.
Pregnant and lactating mothers.
Periodontal treatment within the past 6 months.
Antibiotics or anti-inflammatory drugs taken within the preceding 6 months.
SCREENING EXAMINATION INCLUDE
Gingival index by Loe H & Silness P, 1963.
Plaque index by Silness P & Loe H, 1964.
Probing Pocket Depth (PPD) to be measured using graduated Williams periodontal
probe.
Clinical attachment level measured from CEJ to the base of the pocket.
DURATION OF THE STUDY: 18 Months PROCEDURE:
All the patients will be examined and screened for the suitability of the study and signed consent will be obtained from each patient after explaining the nature of the treatment. In each patient the sites per quadrant will be randomly allotted to the groups. Sites in group I will receive non-surgical periodontal therapy consisting of scaling and root planing. The sites in group II will receive non-surgical periodontal therapy consisting of scaling and root planing followed by methylene blue mediated photodynamic therapy. The sites in group III will receive non-surgical periodontal therapy consisting of scaling and root planing followed by toluidine blue mediated photodynamic therapy. Clinical parameters will be recorded and subgingival plaque samples from the sites will be collected at baseline (pre-treatment),
1month and 3 month interval. Subgingival plaque samples will be collected using sterilized curette and then suspended in 1ml sterile normal saline solution followed by microbiological analysis of the collected samples using Gram’s staining.
STATISTICAL ANALYSIS:
Following tests of statistics will be used in the present study:
1. ANOVA - To compare mean values between the groups.
2. Tukey Test- Pair wise comparison of the groups.
Any other statistical methods if required will be used.
7.3 Does the study require any investigations or interventions to be conducted on patients or other human or animals? If so, please describe briefly :
Yes. Patient will undergo scaling and root planing ,photodynamic therapy and
microbiological analysis pre and post treatment.
7.4 Has ethical clearance been obtained from your institution in case 7.3?
Yes.
Ethical clearance letter has been attached. LIST OF REFERENCES:
8 1. Page RC, Offenbacher S, Schroeder HE, Seymour GJ, Kornman KS. Advances in the
pathogenesis of periodontitis: summary of developments, clinical implications and
future directions. Periodontol 2000. 1997;14:216–248.
2. Chondros P , Nikolidakis D, Christodoulides Nicos, Rossler Ralf, Gutknecht Norbert .
Photodynamic therapy as adjunct to non-surgical periodontal treatment in patients on
periodontal maintenance: a randomized controlled clinical trial. Lasers Med Sci
2009;24(5):681-8
3. Romano E. Photodynamic therapy in periodontal therapy: Microbiological
observations from a private practice. Gen Dent 2010;58(2):e68-73
4. Raghavendra M, Koregol A,Bhola S. Photodynamic therapy: A targeted therapy in
periodontics . Aust Dent J 2009;54(1):S102–9.
5. Takasaki AA, Aoki A,Mizutani Koji,Schwarz Frank,Sculean Anton. Application of
antimicrobial photodynamic therapy in periodontal and peri-implant diseases.
Periodontol 2000.2009; 51:109–40.
6. Pupo YM., Gomes G M. Susceptibility of candida albicans to photodynamic therapy
using methylene blue and toluidine blue as photosensitizing dyes. Acta Odontol
Latinoam 2011; 24(2):188-92. 7. Wilson M, Burns T, Pratten J, Pearson GJ. Bacteria in supragingival plaque samples
can be killed by low-power laser light in the presence of a photosensitizer. J Appl
Bacteriol 1995;78(5):569-74
8. Soukos NS, Wilson M, Burns T, Speight PM. Photodynamic effects of toluidine blue
on human oral keratinocytes and fibroblasts and Streptococcus sanguis evaluated in
vitro. Lasers Surg Med 1996; 18(3): 253–9
9. Braun A, Dehn C,Krause F,Jepsen S. Short-term clinical effects of adjunctive
antimicrobial photodynamic therapy in periodontal treatment: a randomized clinical
trial. J Clin Periodontol 2008; 35(10): 877-84.
10. Usacheva MN, Teichert MC. Comparison of the Methylene Blue and Toluidine Blue
Photobactericidal Efficacy against Gram-Positive and Gram-Negative
Microorganisms. Lasers Surg and Med 2001; 29(2):165-73.
11. Lui J, Corbet EF,Jin L. Combined photodynamic and low-level laser therapies as an
adjunct to nonsurgical treatment of chronic periodontitis. J Periodont Res
2011;46(1):89–96.
12. Giannelli M, Formigli L,Lorenzini L,Bani D. Combined photoablative and
photodynamic diode laser therapy as an adjunct to non-surgical periodontal treatment.
A randomized split-mouth clinical trial. J Clin Periodontol 2012;39: 962–970.