Page 1
Conflict of interest statement
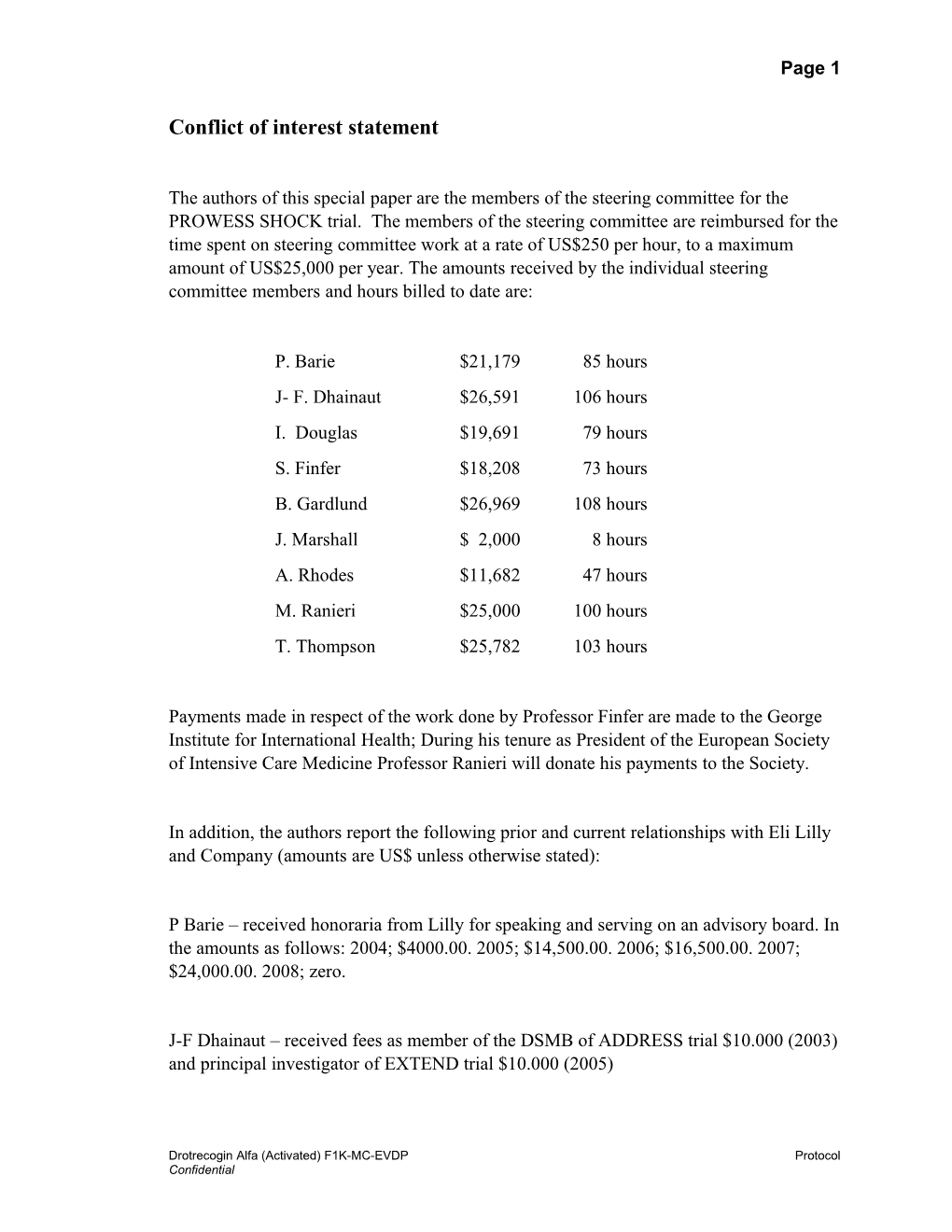
The authors of this special paper are the members of the steering committee for the PROWESS SHOCK trial. The members of the steering committee are reimbursed for the time spent on steering committee work at a rate of US$250 per hour, to a maximum amount of US$25,000 per year. The amounts received by the individual steering committee members and hours billed to date are:
P. Barie $21,179 85 hours J- F. Dhainaut $26,591 106 hours I. Douglas $19,691 79 hours S. Finfer $18,208 73 hours B. Gardlund $26,969 108 hours J. Marshall $ 2,000 8 hours A. Rhodes $11,682 47 hours M. Ranieri $25,000 100 hours T. Thompson $25,782 103 hours
Payments made in respect of the work done by Professor Finfer are made to the George Institute for International Health; During his tenure as President of the European Society of Intensive Care Medicine Professor Ranieri will donate his payments to the Society.
In addition, the authors report the following prior and current relationships with Eli Lilly and Company (amounts are US$ unless otherwise stated):
P Barie – received honoraria from Lilly for speaking and serving on an advisory board. In the amounts as follows: 2004; $4000.00. 2005; $14,500.00. 2006; $16,500.00. 2007; $24,000.00. 2008; zero.
J-F Dhainaut – received fees as member of the DSMB of ADDRESS trial $10.000 (2003) and principal investigator of EXTEND trial $10.000 (2005)
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 2
I. Douglas - received $4,000 between 2004 – 2007 for serving on an advisory board for Eli Lilly & Co.
S Finfer was a founding member of the ANZICS Clinical Trials Group and the Chair of its executive committee from 2000 – 2004, he was convener of the Annual Meeting on Clinical Trials in Intensive Care from 1999 – 2004. Lilly was a sponsor for all the meetings convened by Professor Finfer and all subsequent meetings. The ANZICS Clinical Trials Group received an unrestricted educational grant of A$22,000 from Eli Lilly for the independent statistical analysis of an inception cohort study of Severe Sepsis in Australia and New Zealand (Intensive Care Med. 2004;30:589–596) – Professor Finfer was the Principal Investigator for that study. Professor Finfer presented the results of the above study at a Lilly-sponsored satellite meeting of the Society of Critical Care Medicine meeting in San Antonio in January 2003, Lilly paid Professor Finfer’s traveling expenses and paid an honorarium of $1,000 to the ANZICS Clinical Trials Group.
B Gardlund - no prior relationships declared
J. Marshall - received $1500 for speaking at a Lilly-sponsored symposium during the Critical Care Canada Forum meeting in Toronto (October 2007), and travel costs and a $1500 honorarium for speaking at a meeting of the Polish Sepsis Society in 2003.
A. Rhodes has been the chair of the Congress Committee of the European Society of Intensive Care Medicine from 2005 through to 2008. During this time many of the meetings that were organized by the society were either sponsored or supported by Eli Lilly. A. Rhodes sits on an advisory board for Eli Lilly for which he has been paid £500.00.
V.M. Ranieri - received €2400 for consulting for Eli Lilly from February 2005 to June 2006 on the creation of the "About Sepsis.com” website.
T. Thompson- Between 2000 and 2002, Dr. Thompson was an ad hoc consultant to Lilly related to the design of the STRIVE and ADDRESS trials and was a co-investigator in the STRIVE trial. During this period, Dr. Thompson received financial compensation of $14,000. Between 2002 and 2005, Dr. Thompson was the Chair of the Data Monitoring Committee for the EXPRESS trial. During this time he received compensation of $12,475.
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 3
Confidential Information
The information contained in this protocol is confidential and is intended for the use of clinical investigators. It is the property of Eli Lilly and Company or its subsidiaries and should not be copied by or distributed to persons not involved in the clinical investigation of drotrecogin alfa (activated) (LY203638), unless such persons are bound by a confidentiality agreement with Eli Lilly and Company or its subsidiaries. Protocol F1K-MC-EVDP Efficacy and Safety of Drotrecogin Alfa (Activated) in Adult Patients with Septic Shock
Drotrecogin Alfa (Activated) (LY203638)
A randomized, double-blind, placebo-controlled, multicenter, Phase 3 study of drotrecogin alfa (activated) administered as a continuous 96-hour infusion to adult patients with septic shock.
Eli Lilly and Company Indianapolis, Indiana USA 46285 Protocol Approved by Lilly: 16 August 2007
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 4
Efficacy and Safety of Drotrecogin Alfa (Activated) in Adult Patients with Septic Shock
Table of Contents
Section Page 1. Introduction...... 3 2. Objectives...... 3 2.1. Primary Objective...... 3 2.2. Secondary Objectives...... 3 3. Investigational Plan...... 3 3.1. Summary of Study Design...... 3 3.2. Discussion of Design and Control...... 3 4. Study Population...... 3 4.1. Inclusion Criteria...... 3 4.1.1. Inclusion Criterion – Study Entry/Informed Consent 3 4.1.2. Inclusion Criterion – Enrollment/Randomization...... 3 4.2. Exclusion Criteria...... 3 4.2.1. Rationale for Exclusion of Certain Study Candidates ...... 3 4.3. Discontinuations and Interruptions...... 3 4.3.1. Discontinuation or Interruption of Study Drug...... 3 4.3.2. Discontinuation of Study Sites...... 3 4.3.3. Discontinuation of the Study...... 3 5. Treatment...... 3 5.1. Treatments Administered...... 3 5.2. Materials and Supplies...... 3 5.3. Method of Assignment to Treatment...... 3 5.4. Rationale for Selection of Doses in the Study...... 3 5.5. Selection and Timing of Doses...... 3 5.6. Blinding...... 3 5.7. Concomitant Therapy...... 3 5.7.1. Prohibited Concomitant Medications...... 3 5.7.2. Allowed Concomitant Medications...... 3 5.8. Treatment Compliance...... 3
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 5
6. Efficacy and Safety Evaluations, Sample Collection and Testing, and Appropriateness of Measurements...... 3 6.1. Efficacy Measures...... 3 6.1.1. Primary Efficacy Measure...... 3 6.1.2. Secondary Efficacy Measures...... 3 6.1.3. Other Efficacy Measures...... 3 6.2. Safety Evaluations...... 3 6.2.1. Adverse Events...... 3 6.2.1.1. Serious Adverse Events...... 3 6.2.2. Safety Monitoring...... 3 6.2.3. Complaint Handling...... 3 6.3. Sample Collection and Testing...... 3 6.3.1. Samples for Standard Laboratory Testing...... 3 6.3.2. Samples for Pharmacodynamic Measurements...... 3 6.3.3. Collection Procedures...... 3 6.4. Appropriateness of Measurements...... 3 7. Data Quality Assurance...... 3 7.1. Direct Data Entry and Computerized Systems...... 3 8. Sample Size and Statistical Methods...... 3 8.1. Determination of Sample Size...... 3 8.1.1. Resizing the Study...... 3 8.2. Statistical and Analytical Plans...... 3 8.2.1. General Considerations...... 3 8.2.2. Patient Disposition...... 3 8.2.3. Patient Characteristics...... 3 8.2.4. Primary Outcome and Methodology...... 3 8.2.5. Efficacy Analyses...... 3 8.2.6. Safety Analyses...... 3 8.2.7. Subgroup Analyses...... 3 8.2.8. Interim Analyses...... 3 9. Informed Consent, Ethical Review, and Regulatory Considerations...... 3 9.1. Informed Consent...... 3 9.2. Ethical Review...... 3 9.3. Regulatory Considerations...... 3 9.3.1. Investigator Information...... 3 9.3.2. Protocol Signatures...... 3 9.3.3. Final Report Signature...... 3
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 6
10. References...... 3
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 7
Table of Contents (concluded) List of Protocol Attachments Protocol Attachment EVDP.1. Study Schedule Protocol Attachment EVDP.2. Clinical Laboratory Tests Protocol Attachment EVDP.3. Noncardiovascular Organ Dysfunction Criteria Protocol Attachment EVDP.4. Guidelines for Evidence of Infection Protocol Attachment EVDP.5. Guidelines for Enrollment Protocol Attachment EVDP.6. Estimation of Baseline Creatinine Level
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 8
Abbreviations and Definitions
ANOVA Analysis of variance
APACHE II Acute Physiology and Chronic Health Evaluation II
ASA Acetylsalicylic acid
Audit A systematic and independent examination of the study-related activities and documents to determine whether the evaluated study-related activities were conducted, and the data were recorded, analyzed, and accurately reported according to the protocol, applicable standard operating procedures, good clinical practice, and the applicable regulatory requirements.
Blinding/Masking A procedure in which one or more parties to the study are kept unaware of the treatment assignments. Single-blinding usually refers to the patients being unaware, and double-blinding usually refers to the patients, investigators, monitors, and in some cases, select sponsor personnel being unaware of the treatment assignments.
Complaint A complaint is any written, electronic, or oral communication that alleges deficiencies related to the identity, quality, purity, durability, reliability, safety or effectiveness, or performance of a drug or drug delivery system.
Compliance Adherence to all the trial-related requirements, good clinical practice requirements, and the applicable regulatory requirements.
Confirmation A process used to confirm that laboratory test results meet the quality requirements defined by the laboratory generating the data and that Lilly is confident that results are accurate. Confirmation will either occur immediately after initial testing or will require that samples be held to be retested at some defined time point, depending on the steps required to obtain confirmed results.
Coordinating An third party contracted by Lilly to provide support to the investigative sites Center for certain aspects of the conduct of the study, such as patient enrollment, study drug administration, and serious adverse event reporting.
CRO Clinical research organization
Designee Lilly may delegate the responsibility for certain aspects of the conduct of the study to a third party, such as a clinical research organization or an academic research organization.
DMC Data monitoring committee
DVT Deep venous thrombosis
eCRF Electronic case report form
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 9
End of Study End of study is defined as the date of the last visit or last scheduled procedure at the last site shown in the Study Schedule for the last active subject in the study.
Enroll See Study Entry Terms
Enter See Study Entry Terms
IB Investigator’s Brochure
ICU Intensive care unit
Interim Analysis Any analysis intended to compare treatment groups at any time prior to the formal completion of a trial.
Intention to Treat The principle that asserts that the effect of a treatment policy can be best (ITT) assessed by evaluating on the basis of the intention to treat a patient (that is, the planned treatment regimen) rather than the actual treatment given. It has the consequence that patients allocated to a treatment group should be followed up, assessed, and analyzed as members of that group irrespective of their compliance to the planned course of treatment.
Investigator A person responsible for the conduct of the clinical trial at a study site. If a study is conducted by a team of individuals at a study site, the investigator is the responsible leader of the team and may be called the principal investigator.
IRB/ERB Institutional review board/ethical review board: a board or committee (institutional, regional, or national) composed of medical and nonmedical members whose responsibility is to verify that the safety, welfare, and human rights of the patients participating in a clinical study are protected.
IVRS Interactive voice response system
Legal An individual, judicial, or other body authorized under applicable law to Representative consent on behalf of a prospective patient to the patient's participation in the clinical study.
Opt Out Discontinue study drug and initiate treatment with commercial drotrecogin alfa (activated).
PAI-1 Plasminogen activator inhibitor 1
Patient A subject with a defined disease.
SAP Statistical analysis plan
SIRS Systemic inflammatory response syndrome
SOFA Sequential Organ Failure Assessment
Sponsor Eli Lilly and Company
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 10
Study Entry Terms Screen The act of determining if an individual meets minimum requirements to become part of a pool of potential candidates for participation in a clinical study. Enter/Consent The act of obtaining informed consent for participation in a clinical study from patients deemed eligible or potentially eligible to participate in the clinical study. Patients entered into a study are those who sign the informed consent document directly or through their legally acceptable representatives. Enroll/Randomize The act of assigning a patient to a treatment. Patients who are enrolled in the study are those who have been assigned to a treatment.
Subject An individual who is or becomes a participant in clinical research, either as a recipient of the test article or as a control. A subject may be either a healthy human or a patient.
Treatment- Any untoward medical occurrence that either occurs or worsens at any time Emergent Adverse after treatment baseline and which does not necessarily have to have a causal Event relationship with this treatment.
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 11
Efficacy and Safety of Drotrecogin Alfa (Activated) in Adult Patients with Septic Shock
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 12
1. Introduction
Drotrecogin alfa (activated) has been shown to be beneficial in the treatment of severe sepsis in adult patients (Bernard et al. 2001) and is currently approved for the treatment of adult patients with severe sepsis and a high risk of death. This approval was based on the results of a global Phase 3 study, PROWESS. The indicated population varies in the approved prescribing information: in the European Union, it is defined as severe sepsis with multiple organ dysfunction and, in the United States, as severe sepsis with a high risk of death, for example, an APACHE II score 25. Two recent studies in nonindicated populations, adult patients with severe sepsis at low risk of death (Abraham et al. 2005) and pediatric patients with severe sepsis (Nadel et al. 2007) have failed to demonstrate efficacy in these populations. The European Union’s regulatory authority has requested an additional study to further evaluate the efficacy and safety of drotrecogin alfa (activated) in patients with severe sepsis and to better identify patients who would benefit from drotrecogin alfa (activated) treatment. The regulatory agency of the United States (FDA) is aware of the conduct of this study and has concluded that it is reasonable to conduct an additional placebo-controlled study to provide evidence of efficacy of drotrecogin alfa (activated) for treatment of patients with septic shock. Of course, these regulatory agency opinions do not preclude institutional review board consideration of the study. Septic shock occurs in more than half of patients presenting with severe sepsis (Abraham et al. 2001; Bernard et al. 2001; Warren et al. 2001; Annane et al. 2002; Cole et al. 2002) and has an associated in-hospital mortality rate ranging from 34% to 61%. Septic shock is defined as acute circulatory failure characterized by persistent arterial hypotension and hypoperfusion due to infection. Hypotension is typically defined by a systolic arterial pressure below 90 mm Hg, a mean arterial pressure below 60 mm Hg, or a reduction in systolic blood pressure of 40 mm Hg from baseline, despite adequate volume resuscitation, in the absence of other causes of hypotension (Levy et al. 2003). At present, there is no pharmacologic treatment specifically for septic shock that has been definitively proven to reduce mortality. Thus, treatment continues to be based on eliminating the underlying infection and supporting the patient’s blood pressure with intravenous fluid resuscitation and vasopressor agents (Rivers et al. 2001). Drotrecogin alfa (activated) or recombinant human activated protein C is a 54 kilodalton recombinant glycoprotein with antithrombotic, profibrinolytic, and anti-inflammatory properties. Protein C is an inactive zymogen synthesized in the liver. When coupled to thrombomodulin on the endothelial surface, protein C is converted to activated protein C by thrombin. Significant decreases in protein C levels have been well documented in sepsis and specifically in septic shock (Mesters et al. 2000). Depressed protein C levels have also been associated with sepsis-induced acute lung injury (Sheth and Carvalho 1991) and meningococcal septicemia (Brandtzaeg et al. 1989; Fijnvandraat et al. 1995). Protein C deficiency results partly from a sustained procoagulant state (Brandtzaeg et al. 1989; Fourier et al. 1992; Sheth and Carvalho 1991). Numerous reports have been
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 13 published examining the prognostic value of protein C level in severe sepsis. These reports confirm the association between depressed protein C levels and the increased likelihood of negative outcomes in sepsis, including development of shock and increased mortality (Brandtzaeg et al. 1989; Philippe et al. 1989; Hesselvik et al. 1991; Fourrier et al. 1992, Leclerc et al. 1992; Roman et al. 1992; Peters et al. 1993; Piette et al. 1993; Powars et al. 1993; Hazelzet et al. 1994; Shorr et al. 2006; Brunkhorst et al. 2007). In the PROWESS study, drotrecogin alfa (activated) significantly reduced mortality in patients with severe protein C deficiency. Patients receiving drotrecogin alfa (activated) also had greater increases in protein C level compared with placebo patients (Shorr et al. 2006). Drotrecogin alfa (activated) has also been shown in vitro to decrease sepsis-induced interactions between isolated neutrophils and endothelial cells in patients with septic shock, which may improve microvascular patency (Kirschenbaum et al. 2006). In vitro cell culture and animal data also support that drotrecogin alfa (activated) blocks the induction of adrenomedullin, likely mediated by interferon- and inducible nitric oxide synthase, and suggests a mechanism that may account for ameliorating lipopolysaccharide-induced hypotension (Gupta et al. 2007). Drotrecogin alfa (activated) has also been shown to reduce the hypotensive response in a study of human endotoxin challenge (Kalil et al. 2004). In PROWESS, drotrecogin alfa (activated) treatment resulted in faster resolution of cardiovascular dysfunction at the end of the 96-hour infusion period compared to placebo (Vincent et al. 2003). In addition, Monnet et al. (2005) have shown retrospectively that patients with septic shock treated with drotrecogin alfa (activated) had their vasopressor dose (norepinephrine) decreased compared to age-matched controls not treated with drotrecogin alfa (activated). To date, drotrecogin alfa (activated) has not been studied prospectively in an exclusively septic shock patient population. The safety profile of drotrecogin alfa (activated) has been studied extensively in clinical studies. Table EVDP.1 contains a summary of the safety information from placebo- controlled studies and studies in which open-label drotrecogin alfa (activated) was administered (Williams et al. 2007). The rate of serious adverse events, serious bleeding events, and central nervous system bleeding events has remained relatively consistent between studies. More detailed information about the known benefits and risks of drotrecogin alfa (activated) may be found in the Investigator's Brochure (IB).
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 14
Table EVDP.1. Safety Information from Drotrecogin Alfa (Activated) Studies Placebo-Controlled Studies Open-Labela PROWESS ADDRESS ENHANCE XPRESS DRO PLA DRO PLA DRO DRO N=850 N=840 N=1317 N=1293 N=2378 N=1935 Days 0 through 6 Serious events 58 (6.8) 55 (6.5) 75 (5.7) 78 (6.0) 166 (7.0) 128 (6.6) Serious bleeds 20 (2.4) 8 (1.0) 31 (2.4) 15 (1.2) 85 (3.6) 46 (2.4) CNS bleeds 2 (0.2) 0 4 (0.3) 3 (0.2) 15 (0.6) 6 (0.3) Days 0 through 28 Serious events 106 (12.5) 102 (12.1) 182 (13.8) 183 (14.2) 319 (13.4) 256 (13.2) Serious bleeds 30 (3.5) 17 (2.0) 51 (3.9) 28 (2.2) 155 (6.5) 88 (4.5) CNS bleeds 2 (0.2) 1 (0.1) 6 (0.5) 5 (0.4) 35 (1.5) 17 (0.9) Abbreviations: CNS = central nervous system; DRO = drotrecogin alfa (activated); PLA = placebo. a ENHANCE was an open-label study. XPRESS was a placebo-controlled study of the coadministration of heparin with drotrecogin alfa (activated). Study drug was heparin; open-label drotrecogin alfa (activated) was administered to all patients.
The purpose of this placebo-controlled study is to determine if drotrecogin alfa (activated) treatment provides significant mortality reduction and organ function improvement in patients with septic shock compared with placebo treatment in patients receiving the current standard of care for septic shock. This study will also assess the effectiveness of drotrecogin alfa (activated) in reducing 28-day mortality in patients with septic shock and concomitant severe protein C deficiency at baseline..
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 15
2. Objectives
2.1. Primary Objective The primary objective of this study is to demonstrate that treatment with drotrecogin alfa (activated) 24 mcg/kg/h administered as an intravenous infusion for 96 hours reduces 28-day all-cause mortality in adult patients with septic shock compared with placebo.
2.2. Secondary Objectives The secondary objectives of this study are as follows: To demonstrate that treatment with drotrecogin alfa (activated) reduces 28-day all-cause mortality in adult patients with septic shock and severe protein C deficiency (baseline protein C level less than or equal to half the lower limit of normal) compared with placebo. To demonstrate that treatment with drotrecogin alfa (activated) improves cardiovascular, respiratory, and renal organ function compared with placebo. To demonstrate that treatment with drotrecogin alfa (activated) reduces 90-day and 180-day all-cause mortality in adult patients with septic shock compared with placebo. To demonstrate that patients treated with drotrecogin alfa (activated) have a similar quality of life compared with patients treated with placebo. To demonstrate that drotrecogin alfa (activated) has an acceptable safety profile in this patient population.
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 16
3. Investigational Plan
3.1. Summary of Study Design Study F1K-MC-EVDP is a multicenter, randomized, double-blind, parallel, placebo-controlled, Phase 3 study of drotrecogin alfa (activated) in patients with septic shock. Planned enrollment in the study is approximately 1500 patients. Patients will be randomly assigned to either the drotrecogin alfa (activated) or placebo treatment group in a 1:1 ratio. Randomization will be stratified by investigative site. The study consists of 4 treatment periods: pretreatment, treatment, posttreatment, and follow-up. Figure EVDP.1 illustrates the study design.
Figure EVDP.1. Illustration of study design for Protocol F1K-MC-EVDP.
Refer to Protocol Attachment EVDP.3 for definitions of noncardiovascular organ dysfunction.
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 17
Pretreatment period (Visit 1). This period begins with the start of vasopressor therapy and extends for a maximum of 24 hours to the start of the study drug infusion. The following activities are performed during this period: (1) the patient’s eligibility for the study is assessed, (2) the coordinating center is contacted to confirm eligibility, (3) informed consent is obtained, (4) baseline evaluations are made, and (5) the patient is randomly assigned to a treatment group. The study drug infusion should start within 2 hours of randomization. Treatment period (Visit 2). This period begins with the start of the study drug infusion and continues through Study Day 6. Study drug is administered by intravenous infusion for 96 hours 1 hour. The infusion may extend into Study Day 5 or 6 because of interruptions in the infusion (refer to Section 4.3.1). Posttreatment period (Visit 3). This period begins on Study Day 7 and continues through Study Day 28. Survival status and quality of life are assessed for all patients on Study Day 28. If a patient has been discharged from the study hospital before Study Day 28, site personnel will contact the patient, the patient’s legal or authorized representative, or the patient’s primary physician to determine survival status and assess quality of life. If site personnel are unable to determine the patient’s survival status, the sponsor or designee should be notified. Follow-up period (Visit 4 and Visit 5). Visit 4 begins on Study Day 29 and continues through Study Day 90; Visit 5 begins on Study Day 91 and continues through Study Day 180. Survival status and quality of life are assessed for all patients on Study Day 90 and Study Day 180. Site personnel will contact the patient, the patient’s legal or authorized representative, or the patient’s primary physician to determine survival status and assess quality of life. If site personnel are unable to determine the patient’s survival status, the sponsor or designee should be notified.
3.2. Discussion of Design and Control Design. The design and endpoints of this study have incorporated the key recommendations of the Committee for Medicinal Products for Human Use (CHMP) guidelines for investigations in severe sepsis (CHMP 2006). Septic shock as an independent criterion for the use of drotrecogin alfa (activated) has not been studied in previous trials. A placebo-controlled study of the efficacy of drotrecogin alfa (activated) for the treatment of septic shock will be conducted for several reasons: (1) Drotrecogin alfa (activated) received approval on the basis of a single, pivotal study in patients with severe sepsis (PROWESS). In the European Union, drotrecogin alfa (activated) was licensed under exceptional circumstances and requires an annual review. (2) Since registration, two placebo-controlled studies of drotrecogin alfa (activated) have not shown evidence of efficacy; however, these studies were conducted in nonindicated populations: one in adult patients with severe sepsis who were at low risk of death (F1K- MC-EVCL/EVCM or ADDRESS) and one in pediatric patients with severe sepsis (F1K- MC-EVBP or RESOLVE). (3) Regulatory authorities in the European Union have
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 18 requested an additional study to further evaluate the efficacy and safety of drotrecogin alfa (activated) in patients with severe sepsis, and to better identify patients who would benefit from drotrecogin alfa (activated) treatment. Regulatory authorities in the United States have acknowledged and concurred with a placebo-controlled study of drotrecogin alfa (activated) in patients with septic shock. In the pivotal study of drotrecogin alfa (activated) in patients with severe sepsis (PROWESS), 70% of patients had septic shock and were receiving vasopressor therapy at baseline (Bernard et al. 2001). The current study will only enroll patients with septic shock who are receiving vasopressor therapy. There has been change in the delivery of care for these patients. Specifically, Rivers et al. (2001) showed a 16% absolute mortality reduction in patients with septic shock by initiating early goal-directed therapy in the emergency department. The current study will assume that current institutional standards of care in regard to increased fluid resuscitation, deep venous thrombosis (DVT) prophylaxis, and timely antibiotic therapy will be performed. Control. No suitable active control exists as there is no other pharmacological agent approved for the treatment of septic shock with sufficient similarity to drotrecogin alfa (activated). Therefore, placebo is an appropriate control for this study.
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 19
4. Study Population
4.1. Inclusion Criteria Patients are eligible to be included in the study only if they meet the following criteria. Criteria [1] through [4] must be met at the time of study entry/informed consent signed; Criterion [5] must be met at the time of enrollment/randomization.
4.1.1. Inclusion Criterion – Study Entry/Informed Consent [1] Must be an adult (18 years old) [2] Must have evidence of an infection for which the patient is receiving intravenous antimicrobial therapy (refer to Protocol Attachment EVDP.4 for guidelines). [3] Must have systemic inflammatory response syndrome (SIRS). Patients must meet at least 2 of the criteria defined below during the 36 hours prior to study entry. (a) Core temperature 38 C (100.4 F) or 36 C (96.8 F). Core temperature is defined as rectal, central catheter, or tympanic. If oral or axillary temperature is used, add 0.5 C or 1 F to the measured value. Hypothermia (36 C or 96.8 F) must be determined by a rectal or central catheter temperature. (b) Heart rate 90 beats/minute. (c) Respiratory rate 20 breaths per minute or a PaCO2 32 mm Hg or mechanical ventilation for an acute process. (d) White blood cell count of 12,000/mm3 or 4000/mm3 or >10% immature neutrophils. [4] Must have septic shock, which is defined as the following: (a) The patient must have received 30 mL/kg of intravenous fluid during the resuscitation period. The resuscitation period begins 4 hours prior to the initiation of vasopressor therapy and ends 4 hours after start of vasopressor therapy). (b) The patient must have a continuous requirement for vasopressor support for at least 4 hours at a minimum dose of at least 1 of the vasopressors shown below: norepinephrine 5 mcg/min dopamine 10 mcg/kg/min phenylephrine 25 mcg/min epinephrine 5 mcg/min
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 20
vasopressin 0.03 units/min (c) Must have clinical signs consistent with hypoperfusion. The patient must meet at least 1 of the following criteria during the 36 hours prior to study entry: Metabolic acidosis: base deficit 5.0 mEq/L or venous bicarbonate <18 mEq/L or lactate 2.5 mMol/L. Acute oliguria/renal injury: urine output <0.5 mL/kg/h for 1 hour or a 50% increase in creatinine from a known or calculated baseline level (estimated using the MDRD equation or a similar estimation of baseline creatinine, refer to Protocol Attachment EVDP.6). Patients with a history of chronic renal disease must meet the metabolic acidosis or acute hepatic dysfunction criterion. Acute hepatic dysfunction: AST or ALT >500 IU/dL or bilirubin >2 g/dL. Patients with a history of acute hepatitis or chronic liver disease must meet the metabolic acidosis or oliguria/renal injury criterion for evidence of hypoperfusion.
4.1.2. Inclusion Criterion – Enrollment/Randomization [5] Patients must remain vasopressor dependent throughout the pretreatment period and through the time of randomization at any vasopressor dose with the goal of maintaining a systolic blood pressure of approximately 90 mm Hg or higher or a mean arterial pressure of approximately 65 mm Hg or higher with reasonable attempts made to wean the patient from vasopressor support, if applicable. (Note: dopamine at doses <5 mcg/kg/min does not fulfill the criteria for vasopressor dependency.)
4.2. Exclusion Criteria Patients will be excluded from the study if they meet any of the following criteria: [6] Have receivedvasopressor therapy (at any dose) for greater than 24 hours prior to the start of study drug. [7] Have sepsis-induced organ dysfunction (respiratory, renal, hematologic, or unexplained metabolic acidosis; refer to Protocol Attachment EVDP.3 for definitions) for greater than 36 hours prior to the start of the study drug infusion. [8] Have single organ dysfunction and recent surgery (within 30 days of study entry).
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 21
Surgery is defined as a surgical procedure that requires general or spinal anesthesia or a biopsy or surgical procedure of a closed space in which there is a high risk of significant bleeding and it would not be possible to control bleeding by external pressure. [9] Have had surgery performed within the 12-hour period immediately preceding the study drug infusion, or are postoperative with evidence of active bleeding, or have planned or anticipated surgery during the infusion period (for example, patients with staged surgeries or burn patients with planned excisions and grafting; peritoneal lavage alone is not considered planned surgery). (Refer to exclusion criterion [8] for definition of surgery.) [10] Have a platelet count <30,000/mm3. [11] Have a prothrombin time-international normalized ratio (INR) >5.0. [12] Have active internal bleeding or are at increased risk for bleeding, for example: (a) History (within the previous 3 months) of stroke or severe head trauma that required hospitalization or intracranial surgery. (b) History of intracranial arteriovenous malformation, cerebral aneurysm, or central nervous system mass lesion. (c) Patients with an epidural catheter in place or who are anticipated to receive an epidural catheter during the study drug infusion. (d) History of congenital bleeding diatheses (for example, hemophilia). (e) Gastrointestinal bleeding within the 6 weeks prior to study entry that required medical intervention unless definitive/curative endoscopic procedure or surgery has been performed. (f) Patients with known esophageal varices, chronic jaundice, cirrhosis, or chronic ascites. (g) Trauma patients at increased risk of life-threatening bleeding (for example, flail chest; significant contusion to lung, liver, or spleen; retroperitoneal bleed; pelvic fracture; compartment syndrome). [13] Are receiving any of the following medications at study entry or will have a concurrent need for any of the following medications during the study drug infusion: (a) Therapeutic heparin, defined as unfractionated heparin >15,000 U/day within 8 hours of study entry or low molecular weight heparin used at any dose higher or more frequent than the recommended dose in the product label for DVT prophylaxis within 12 hours of study entry.
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 22
(b) Direct thrombin inhibitors, such as argatroban, ximelagatran, melagatran, bivalirudin, lepirudin, or recombinant hirudins within 3 days of study entry. (c) Thrombolytic therapy, such as streptokinase, tPA, rPA, or urokinase (unless used to treat intra-catheter thrombosis) within 3 days of study entry. (d) Warfarin, if used within 7 days of study entry or warfarin-type medications within 5 half-lives of study entry and where the prothrombin time is prolonged beyond the upper limit of normal for the institution. (e) Antiplatelet medications, such as ticlopidine, clopidogrel, or ascetylsalicylic acid (ASA) >650 mg/day or compounds that contain ASA >650 mg/day, within 3 days of study entry. (f) Glycoprotein IIb/IIIa receptor antagonists, such as abciximab or eptifibatide, within 7 days of study entry. (g) Recombinant factor VIIa within 30 days of study entry. (h) Antithrombin infusion of >10,000 units within 12 hours of study entry. (i) Protein C concentrate infusion within 24 hours of study entry. [14] Are not expected to survive 28 days given their preexisting uncorrectable medical condition, for example, patients with, or suspected to have the following conditions: (a) Poorly controlled neoplasms (b) End-stage cardiac disease (c) Cardiac arrest requiring cardiopulmonary resuscitation or with pulseless electrical activity or asystole within the past 30 days (d) End-stage lung disease (e) End-stage liver disease (f) HIV/AIDS with known end-stage processes. Refer to Protocol Attachment EVDP.5 for further guidelines. [15] Are moribund and death is perceived to be imminent (within 24 hours). [16] Are not committed to aggressive management of the patient. For example, the patient’s family or primary physician is unwilling to place the patient on mechanical ventilation or an advanced directive to withhold life support, with the exception of cardiopulmonary resuscitation, is present.
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 23
[17] Have received treatment within the last 30 days with drotrecogin alfa (activated). [18] Have previously completed or withdrawn from this study (F1K-MC- EVDP). [19] Are pregnant or lactating and the milk is to be ingested by the newborn. [20] Fail to give written informed consent or the patient’s legal representative fails to give written informed consent. [21] Have received treatment within the last 30 days with a drug that has not received regulatory approval for any indication at the time of study entry. [22] Are participating concurrently to this study in any clinical study for an investigational drug or device for the treatment of sepsis or septic shock. [23] Are investigative site personnel directly affiliated with this study and/or their immediate family. Immediate family is defined as a spouse, parent, child, or sibling, whether biological or legally adopted. [24] Are Lilly employees.
4.2.1. Rationale for Exclusion of Certain Study Candidates Exclusion Criteria [6] and [7] exclude patients with septic shock requiring vasopressor support for longer than 24 hours or whose first sepsis-induced organ dysfunction occurred greater than 36 hours prior to the start of the study drug infusion. Approximately 90% of patients in PROWESS received study drug within 24 hours of the onset of sepsis-induced organ dysfunction. In an open-label study, ENHANCE, only about 50% of patients received study drug within 24 hours of the onset of the first sepsis- induced organ dysfunction. In analyses of mortality by time from first organ dysfunction to start of study drug, patients who received drotrecogin alfa (activated) within 24 hours of the onset of organ dysfunction had better outcomes compared with patients who received drotrecogin alfa (activated) greater than 24 hours from the onset of organ dysfunction. The recommendation to consider treatment with drotrecogin alfa (activated) within 24 hours of the onset of organ dysfunction has been incorporated into the product label in the European Union and other countries. Exclusion Criterion [8] excludes patients with single organ dysfunction and recent surgery. In 2 previous studies of drotrecogin alfa (activated) in patients with severe sepsis (PROWESS and ADDRESS), subgroup analyses of surgical patients with single organ dysfunction showed that patients receiving drotrecogin alfa (activated) had higher mortality than patients receiving placebo. Exclusion Criteria [9], [10], [11], [12], and [13] exclude patients who are at increased risk of bleeding; bleeding events are the only adverse events that were noted in previous
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 24 studies to occur more frequently in drotrecogin alfa (activated) patients than placebo patients. Exclusion Criteria [14], [15], and [16] exclude patients who are likely to die of their preexisting uncorrectable medical condition before Study Day 28. Exclusion Criteria [17] and [18] are included to avoid confounding with recent prior treatment with the study drug. Exclusion criterion [19] is included because there are not sufficient data to support the use of drotrecogin alfa (activated) in pregnant or lactating women. Exclusion Criterion [20] is included for ethical and regulatory reasons. Exclusion Criterion [21] eliminates drugs that cannot be mapped to a standard drug dictionary or for which little data are known to analyze the potential relationship of adverse events or drug interactions. Exclusion Criteria [22], [23], and [24] reduce the potential bias that may be introduced at the study site.
4.3. Discontinuations and Interruptions
4.3.1. Discontinuation or Interruption of Study Drug The criteria for entry and enrollment must be followed explicitly. If a patient who does not meet the entry and enrollment criteria is inadvertently enrolled and the study drug infusion has been started, the investigator should consult with the coordinating center regarding the termination or continuation of the study drug infusion. If study drug is discontinued, the patient will continue in the study and undergo all study assessments per the protocol in order to provide the follow-up data needed for the analysis of the entire intention-to-treat (ITT) population. Bleeding. Should clinically important bleeding occur, the study drug infusion should be stopped immediately. The infusion can be restarted once adequate hemostasis has been achieved and there are no signs or symptoms of bleeding and no exclusion criteria have developed. The study drug infusion should not be restarted if the infusion has been interrupted for more than 36 continuous hours. Abnormal coagulation. If the patient develops any of the following coagulation abnormalities, the study drug should be stopped: Platelet count <30,000/mm3 Prothrombin time-INR >5 Following corrective treatment, the study drug infusion can be resumed if all of the following conditions are met: Platelet count 30,000/mm3. If study drug is resumed, platelet count must be checked at least every 6 hours for 24 hours following any platelet transfusion. Prothrombin time-INR 5. If study drug is resumed, prothrombin time must be checked at least every 12 hours for 24 hours following any transfusion of plasma products, such as fresh frozen plasma. Study drug has been discontinued for less than 36 hours.
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 25
Procedures. Table EVDP.2 contains guidelines for interrupting and resuming the study drug infusion for procedures.
Table EVDP.2. Guidelines for Interrupting and Resuming Study Drug Infusion
Procedure Interrupting Study Drug Resuming Study Druga Central venous catheter 2 hours prior to procedure Immediately after procedure Arterial catheter 2 hours prior to procedure Immediately after procedure Chest tube insertion 2 hours prior to procedure Immediately after procedure Re-intubation requiring tube changer 2 hours prior to procedure Immediately after procedure Lumbar puncture 2 hours prior to procedure Immediately after procedure Sinus puncture 2 hours prior to procedure Immediately after procedure Thoracic drainage 2 hours prior to procedure Immediately after procedure Tracheostomy 2 hours prior to procedure Immediately after procedure Surgeryb 2 hours prior to procedure 12 hours after procedure a Resume study drug if there are no signs of bleeding and the investigator feels there is minimal risk of bleeding complications and is comfortable with resuming the study drug infusion. b Surgery is defined as a surgical procedure that requires general or spinal anesthesia or a biopsy or surgical procedure of a closed space in which there is a high risk of significant bleeding and it would not be possible to control bleeding by external pressure.
Interruption of study drug infusion. Every attempt should be made to complete the study drug infusion without interruption. However, if an interruption occurs, the infusion should be restarted if there are no signs or symptoms of bleeding and no exclusion criteria related to increased risk of bleeding have developed. For continuous interruptions of 1 hour or longer, the planned duration of the infusion should be extended to compensate for the time that the infusion was interrupted. The study drug infusion should not be restarted if the infusion has been interrupted for more than 36 continuous hours. Discontinuation of study drug infusion. Discontinuation of study drug infusion is defined as termination of the study drug infusion without the intent to restart the infusion at a later time. Patients whose infusion is discontinued prior to completion of 96 hours of infusion, regardless of the reason for stopping, are not discontinued from the study. All patients should be followed to determine their 28-day, 90-Day, and 180-day survival status and to assess quality of life. Patients will discontinue the study drug infusion in the following circumstances: Patient has completed 96 hours of infusion.
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 26
The investigator decides that study drug should be discontinued. If this decision is made because of a serious adverse event or a clinically significant laboratory value, the study drug is to be discontinued and appropriate measures taken. The coordinating center is to be alerted immediately. Refer to Section 6.2, Safety Evaluations. The patient, the patient’s legal authorized representative, or attending physician requests that study drug be discontinued. If this decision is made because the patient’s condition has worsened and the investigator determines that it is essential for the management of the patient to unblind the treatment assignment and potentially change the course of therapy, the coordinating center must be alerted immediately. The medical care provided to the patient is always at the discretion of the attending physician. The patient, for any reason, requires treatment with a prohibited concomitant medication (refer to Section 5.7.1). Withdrawal from the study. In the event that the patient, the patient’s legal representative, the investigator, or Lilly decides that the patient should be withdrawn from the study, the study drug infusion and all scheduled survival status assessments, physiologic assessments, and laboratory testing will be discontinued. The coordinating center must be alerted immediately if a patient is withdrawn from the study. A patient will be withdrawn from the study in the following situations: The patient or the patient’s legal representative withdraws consent. The investigator or Lilly, for any reason, stops the patient's participation in the study.
4.3.2. Discontinuation of Study Sites Study site participation may be discontinued if Lilly, the investigator, or the ethical review board of the study site judges it necessary for any reason.
4.3.3. Discontinuation of the Study The study will be discontinued if Lilly judges it necessary for any reason.
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 27
5. Treatment
5.1. Treatments Administered This study involves a comparison of drotrecogin alfa (activated) 24 mcg/kg/h administered intravenously for 96 hours 1 hour with placebo. Patients randomly assigned to the placebo treatment group will receive sterile 0.9% sodium chloride. The patient’s most recent actual weight recorded in the medical record or other source document should be used to prepare the study drug. If the patient’s body weight cannot be measured, an estimate of the patient’s current weight should be made from the last known weight. The weight used to prepare the study drug must be recorded in the patient’s medical record. Study drug will be administered as a continuous 96-hour infusion via a dedicated intravenous line or a dedicated lumen of a multilumen venous catheter. The only other solutions that can be administered through the same line are 0.9% sodium chloride, lactated Ringer’s, dextrose, and dextrose/sodium chloride. The investigator or his/her designee is responsible for explaining the correct use of the investigational agent to site personnel, verifying that instructions are followed properly, maintaining accurate records of study drug dispensing and collection, and returning all unused medication to Lilly or its designee at the end of the study.
5.2. Materials and Supplies Lilly will provide drotrecogin alfa (activated) as a sterile, freeze-dried product in glass vials. Each vial will contain an equivalent of 5 mg or 20 mg of drotrecogin alfa (activated). Clinical trial materials will be labeled according to the country’s regulatory requirements. Placebo of sterile 0.9% sodium chloride will be obtained locally by the investigative sites. Shrouds for the intravenous infusion bags will be provided by Lilly. The intravenous infusion bags will be shrouded after preparation of the study drug and will remain shrouded throughout the duration of the infusion.
5.3. Method of Assignment to Treatment Patients who meet all criteria for enrollment will be randomly assigned to double-blind treatment at Visit 1. Assignment to treatment groups will be determined by a computer-generated random sequence using an interactive voice response system (IVRS). To help achieve between-group comparability for site factor, the randomization will be stratified by site.
5.4. Rationale for Selection of Doses in the Study Drotrecogin alfa (activated) 24 mcg/kg/h administered as a intravenous infusion for 96 hours is the dose and infusion duration approved for the treatment of patients with severe sepsis.
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 28
5.5. Selection and Timing of Doses Patients will receive study drug at the dose described in Section 5.1. Dose adjustments are not permitted in this study.
5.6. Blinding This is a double-blind study. The patient’s treatment assignment will be provided to the unblinded pharmacist or designee by an IVRS. The randomization code for treatment assignment will be retained by the IVRS. It is anticipated that there will be little need to unblind the patient’s treatment assignment. Given that drotrecogin alfa (activated) has a very short half-life and there is no known treatment to increase the clearance or counter the effects of drotrecogin alfa (activated), incidences where unblinding could be beneficial should be rare. Emergency unblinding for adverse events may be performed through the IVRS. This option may be used ONLY if the patient's well-being requires knowledge of the patient’s treatment assignment. All calls resulting in an unblinding event are recorded and reported by the IVRS. The investigator should make every effort to contact the coordinating center prior to unblinding a patient's treatment assignment. If a patient's treatment assignment is unblinded, the coordinating center must be notified immediately by telephone.
5.7. Concomitant Therapy
5.7.1. Prohibited Concomitant Medications The following medications may not be given to the patient during the administration of study drug: Therapeutic heparin, defined as unfractionated heparin >15,000 U/day or low molecular weight heparin used at any dose higher or more frequent than the recommended dose in the product label for DVT prophylaxis or hemodialysis. Direct thrombin inhibitors, such as argatroban, ximelagatran, melagatran, bivalirudin, lepirudin, or recombinant hirudins. Thrombolytic therapy, such as streptokinase, tPA, rPA, and urokinase. Note: Thrombolytic therapy can be used for the dissolution of intracatheter thromboses only; however, care should be taken to avoid systemic administration. Warfarin or warfarin-type medications Glycoprotein IIb/IIIa receptor antagonists Antiplatelet medications, such as the following:
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 29
Ascetylsalicylic acid (ASA) >650 mg/day or compounds that contain ASA >650 mg/day Any dose of thienopyridines, such as ticlopidine or clopidogrel Recombinant factor VIIa Antithrombin Protein C concentrate Commercially available drotrecogin alfa (activated). If any of these agents are required during the study drug infusion, the infusion must be discontinued and the concomitant therapy may be administered starting 2 hours after stopping the study drug infusion.
5.7.2. Allowed Concomitant Medications The following anticoagulant medications are permitted during study drug administration: Drotrecogin alfa (activated) is not indicated for DVT prophylaxis. Therefore, unfractionated and low molecular weight heparin at the dose recommended in the product labeling as a prophylactic treatment for DVT are allowed concomitant medications. Prophylactic treatment for DVT is considered standard of care for patients with septic shock (Geerts et al. 2004). When possible, sites should make a decision regarding the appropriate DVT prophylaxis for patients prior to starting the study drug infusion. If a patient is receiving prophylactic dose heparin before study entry, starting treatment with drotrecogin alfa (activated) of itself does not require the cessation of prophylactic heparin treatment. Baseline prophylactic heparin treatment should only be discontinued if deemed medically necessary. Unfractionated heparin <15 U/kg/h or low molecular weight heparin at the dose recommended in the product labeling in conjunction with acute hemodialysis or continuous renal replacement therapy. Thrombolytic therapy, such as streptokinase, tPA, rPA, and urokinase, for the dissolution of intracatheter thromboses only; care should be taken to avoid systemic administration. Discontinuation of prophylactic heparin therapy. Clinicians should continue prophylactic heparin when initiating study drug unless discontinuation is considered medically necessary. If prophylactic heparin therapy is discontinued during the pretreatment period, blood samples should be drawn just prior to the start of the study drug infusion and every 12 hours for 72 hours after the start of the infusion to measure prothrombin fragment 1.2 (F1.2) and thrombin-antithrombin complex (TATc). This investigation will examine whether these patients have evidence of increased coagulation following abrupt cessation of prophylactic heparin.
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 30
5.8. Treatment Compliance Study drug will be administered by site personnel at the study hospital.
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 31
6. Efficacy and Safety Evaluations, Sample Collection and Testing, and Appropriateness of Measurements
Study procedures and their timing (including tolerance limits for timing) are summarized in the Study Schedule (Protocol Attachment EVDP.1).
6.1. Efficacy Measures
6.1.1. Primary Efficacy Measure The primary efficacy measure is 28-day all-cause mortality. The 28-day time point is defined at 672 hours from randomization. All patients will be classified as either “alive at Study Day 28” or, if dead, “dead at Study Day 28.”
6.1.2. Secondary Efficacy Measures The following measures will be used to assess the secondary efficacy endpoints. Twenty-eight-day mortality by protein C class. Mortality will be examined in patients with severe protein C deficiency, which is defined as a baseline protein C level less than or equal to half the lower limit of normal. Organ function. Changes in organ function will be assessed quantitatively with the following measurements: Cardiovascular function: lactate level, bicarbonate level, pressure-adjusted heart rate, central venous oxygenation, vasopressor usage, and cardiovascular Sequential Organ Failure Assessment (SOFA) score
Respiratory function: oxygenation index, PaO2/FiO2 (P/F ratio), SpO2/FiO2 (S/F ratio), mechanical ventilation usage, and respiratory SOFA score Renal function: creatinine level, microalbumin/creatinine ratio, urine output, renal replacement therapy usage, and renal SOFA score Long-term mortality. Date of death will be recorded for all patients who have died on or before Study Day 180. Ninety-day mortality, 180-day mortality, and median survival time will be calculated for each treatment group. Quality of life. The Euro-QoL-5 and SF-12 scales will be used to evaluate quality of life at baseline and Study Days 28, 90, and 180 (EuroQol Group 1990; Brooks 1996; Ware et al. 1996).
6.1.3. Other Efficacy Measures The following efficacy measures will also be evaluated: Other organ function assessments. Hematologic and hepatic organ function will be assessed using the following measures:
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 32
Hematologic function: protein C level and hematologic SOFA score Hepatic function: hepatic SOFA score Sequential Organ Function Assessment (SOFA; Vincent et al. 1996): Cardiovascular, respiratory, renal, hepatic, and hematology organ function will be assessed using the SOFA methodology. Scores are based on laboratory data, vasopressor dosages, and the need for mechanical ventilation. Scores range from 0 to 4 with an increasing score indicating increasing organ dysfunction. Hospital resource utilization. Resource utilization will be assessed using measures of vasopressors, mechanical ventilation, or renal replacement therapy (hemodialysis, peritoneal dialysis, or continuous veno-venous hemofiltration) usage and the number of days in the intensive care unit (ICU) and study hospital.
6.2. Safety Evaluations Investigators are responsible for monitoring the safety of patients who have entered this study and for alerting Lilly or its designee to any event that seems unusual, even if this event may be considered an unanticipated benefit to the patient. The investigator is responsible for the appropriate medical care of patients during the study. The investigator remains responsible for following, through an appropriate health care option, adverse events that are serious or that caused the patient to discontinue before completing the study. The patient should be followed until the event is resolved or explained. Frequency of follow-up evaluation is left to the discretion of the investigator.
6.2.1. Adverse Events The following adverse events will be collected during Study Days 0 through 28: Serious adverse events Nonserious adverse events that are considered by the investigator to be related to study drug Adverse events that lead to permanent discontinuation of the study drug infusion All thrombotic events (serious and nonserious) All bleeding events (serious and nonserious). Lilly has standards for reporting adverse events that are to be followed regardless of applicable regulatory requirements that may be less stringent. A clinical trial adverse event is any untoward medical event associated with the use of a drug or drug delivery system in humans, whether or not it is considered related to a drug or drug delivery system. Lack of drug effect is not an adverse event in clinical trials because the purpose of the clinical trial is to establish drug effect.
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 33
After the informed consent document is signed, adverse events related to protocol procedures are reported to Lilly or its designee via electronic data entry. Adverse events (as described above) that occur after the patient receives the first dose of study drug must be reported to Lilly or its designee via electronic data entry. Study site personnel will record any daily dosage of study drug that exceeds the maximum dosage in the protocol or in the relevant reference safety document (eg, clinical dosage section for humans in the Investigator Brochure), whichever is greater, via electronic data entry. Investigators will be instructed to report to Lilly or its designee their assessment of the potential relatedness of each adverse event to protocol procedure and study drug via electronic data entry. Investigators will determine relatedness of an event to study drug based on a temporal relationship as well as if the event is unanticipated or unexplained given the patient’s clinical course, previous medical conditions, and concomitant medications. An event should be recorded as “drug related” if the investigator believes it to be reasonably related to study drug. Study site personnel must alert Lilly or its designee within 24 hours of the investigator unblinding a patient’s treatment group assignment for any reason. If a patient's treatment is discontinued as a result of an adverse event, study site personnel must clearly report to Lilly or its designee via electronic data entry the circumstances and data leading to discontinuation of treatment. Given that drotrecogin alfa (activated) has a very short half-life and there is no known treatment to increase the clearance or counter the effects of drotrecogin alfa (activated), situations where unblinding could be beneficial should be rare. Study-specific clinical outcomes of severe sepsis are exempt from all adverse event reporting unless the investigator deems the event to be related to the administration of study drug. The following events will be considered clinical outcomes: Death related to severe sepsis, that is, related to severe sepsis or a sequela of sepsis based on the interpretation of the investigator. Cardiovascular events: the need for vasoactive drugs or hypotension.
Respiratory events: decreased PaO2/FiO2, mechanical ventilation, hypoxia, acute respiratory distress syndrome, acute lung injury, or respiratory failure. Hepatic events: hepatic injury or liver dysfunction that leads to an increase from baseline in the serum level of bilirubin. Renal events: renal failure, renal insufficiency, or renal injury that leads to an increase from baseline in serum creatinine. Hematologic/coagulation events: coagulopathy, disseminated intravascular coagulation, thrombocytopenia, or thrombocytosis.
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 34
Systemic inflammatory response syndrome related criteria: tachypnea, hypopnea, leukocytosis, leukopenia, hypothermia, hyperthermia, tachycardia, or bradycardia. Note: Arrhythmias, such as atrial fibrillation, heart block, ventricular tachycardia, or ventricular fibrillation, are not considered clinical outcomes and should be recorded as adverse events if they are serious events, are considered by the investigator to be related to study drug, or lead to discontinuation of the study drug infusion.
6.2.1.1. Serious Adverse Events Serious adverse event collection begins after the patient has signed informed consent and has received study drug. If a patient experiences a serious adverse event after signing informed consent, but prior to receiving study drug, the event will NOT be collected unless the investigator feels the event may have been caused by a protocol procedure. Study site personnel must alert the coordinating center of any serious adverse event within 24 hours of investigator awareness of the event via a Sponsor-approved method. Alerts issued via telephone are to be immediately followed with official notification on study-specific serious adverse event forms. A serious adverse event is any adverse event that results in one of the following outcomes and is not classified as a clinical outcome of severe sepsis using the definitions shown above: any central nervous system bleeding a bleeding event that leads to the administration of 3 or more units of packed red blood cells per day for 2 consecutive days death that is not related to severe sepsis or a sequelae of sepsis or death that is considered by the investigator to be related to study drug prolonged inpatient hospitalization or rehospitalization a life-threatening experience (that is, immediate risk of dying) persistent or significant disability/incapacity congenital anomaly/birth defect considered significant by the investigator for any other reason. Important medical events, other than those classified as a clinical outcome of severe sepsis, that may not result in death, be life-threatening, or require hospitalization may be considered serious adverse events when, based upon appropriate medical judgment, they may jeopardize the patient and may require medical or surgical intervention to prevent one of the outcomes listed in this definition. Serious adverse events will be collected during the 28-day study period, regardless of the investigator's opinion of causation. Thereafter, serious adverse events are not required to be reported unless the investigator feels the events were related to either study drug or a protocol procedure.
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 35
6.2.2. Safety Monitoring The Lilly clinical research physician will monitor blinded safety data throughout the course of the study. Lilly will review serious adverse events within time frames mandated by company procedures and local regulatory requirements and will review trends, laboratory analytes, and adverse events at periodic intervals. In the event that safety monitoring uncovers an issue that needs to be addressed by unblinding at the group level, only members of the data monitoring committee (DMC; an advisory group for this study formed to protect the integrity of data; refer to Section 8.2.8) can conduct additional analyses of the safety data. For the purpose of this study, in which mortality is a primary endpoint, all deaths and serious adverse event reports will be reviewed in a blinded manner by the Lilly clinical team during the clinical trial. These reports will be reviewed to assure completeness and accuracy, but will not be unblinded to the Lilly clinical team during the study. If a death or clinical adverse event is deemed serious, unexpected, and possibly related to study drug, only Lilly Global Patient Safety will be unblinded for regulatory reporting and safety monitoring purposes. These measures will preserve the integrity of the data collected during this trial and minimize any potential for bias while providing for appropriate safety monitoring.
6.2.3. Complaint Handling Lilly collects product complaints on study drugs and drug delivery systems used in clinical trials in order to ensure the safety of study participants, monitor quality, and to facilitate process and product improvements. Complaints related to unblinded comparator drugs or concomitant drugs/drug delivery systems are reported directly to the manufacturers of those drugs/devices in accordance with the package insert. For blinded studies, all product complaints associated with material packaged, labeled, and released by Lilly will be reported via product complaint forms. The investigator or his/her designee is responsible for handling the following aspects of the product complaint process in accordance with the instructions provided for this study: recording a complete description of the product complaint reported and any associated adverse events using the study-specific complaint forms provided for this purpose faxing the completed product complaint form within 24 hours to Lilly or its designee determining when a drug/drug delivery system is to be returned for investigation.
6.3. Sample Collection and Testing Protocol Attachment EVDP.2 lists the specific tests performed for this study.
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 36
6.3.1. Samples for Standard Laboratory Testing Blood and urine samples will be collected at the times specified in the Study Schedule (Protocol Attachment EVDP.1). Standard laboratory tests, including hematology panel, blood lactate level, creatinine, and pregnancy test (if applicable), will be performed by a local laboratory. Other clinical laboratory tests will be analyzed by a central laboratory. Central laboratory data will not be reported to investigative sites. Protocol Attachment EVDP.2 lists the specific tests that will be performed for this study. Investigators must document their review of local laboratory reports and any central laboratory panic alerts. Samples collected for specified central laboratory tests will be destroyed within 60 days of receipt of confirmed test results. Certain samples may be retained for a longer period, if necessary, to comply with applicable laws, regulations, or laboratory certification standards.
6.3.2. Samples for Pharmacodynamic Measurements Blood samples will be collected at the times specified in the Study Schedule (Protocol Attachment EVDP.1) to measure markers of coagulation (activated partial thromboplastin time and prothrombin time) and other biomarkers (protein C and plasminogen activator inhibitor 1). Samples collected to measure markers of coagulation and other biomarkers will be destroyed within 60 days of receipt of confirmed test results.
6.3.3. Collection Procedures Approximately 38 mL of blood will be collected by venipuncture or through a central line at Visit 1, approximately 138 mL of blood will be collected during Visit 2, and approximately 48 mL of blood will be collected during Visit 3. Approximately 1 mL of urine will be collected at Visit 1 and 2 mL during Visit 2. Supplies required for the collection and shipment of the patients’ stored samples will be supplied by the sponsor. Sample handling and shipment to the central laboratory will occur per instructions given to the study site.
6.4. Appropriateness of Measurements All assessments are widely used and generally regarded as reliable, accurate, and relevant.
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 37
7. Data Quality Assurance
To ensure accurate, complete, and reliable data, Lilly or its representatives will do the following: provide instructional material to the study sites, as appropriate. sponsor a start-up training session to instruct the investigators and study coordinators. This session will give instruction on the protocol, the completion of the electronic case report form (eCRF), and study procedures. make periodic visits to the study site. be available for consultation and stay in contact with the study site personnel by mail, telephone, and/or fax. review and evaluate case report form data and use standard computer edits to detect errors in data collection. conduct a quality review of the database. In addition, Lilly or its representatives may periodically check a sample of patient data recorded against source documents at the study site. The study may be audited by Lilly Medical Quality Assurance (MQA) or its representatives, and/or regulatory agencies at any time. Investigators will be given notice before an audit occurs. To ensure the safety of participants in the study, and to ensure accurate, complete, and reliable data, the investigator will keep records of laboratory tests, clinical notes, and patient medical records in the patient files as original source documents for the study. If requested, the investigator will provide the sponsor, applicable regulatory agencies, and applicable ethical review boards with direct access to original source documents.
7.1. Direct Data Entry and Computerized Systems An electronic data capture system will be used in this trial. Some or all of a patient’s data (for example, a rating scale) may be directly entered into the system on an eCRF at the time that the information is obtained. In these instances where there is no prior written or electronic record of the data, the eCRF will serve as the source document. Any data for which the eCRF will serve as the source document will be identified and documented by each site in that site’s study file. Data collected on the eCRF by the clinical research organization (CRO) will be encoded by the CRO and stored electronically in the CRO’s database system. Validated data will subsequently be transferred to the sponsor’s data warehouse, using standard Lilly file transfer processes. Data managed by a central vendor, such as laboratory test data, will be stored electronically in the central vendor’s database system. Data will subsequently be transferred from the central vendor to Lilly.
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 38
Data from complaint forms submitted to Lilly will be encoded and stored in the global product complaint management system.
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 39
8.Sample Size and Statistical Methods
8.1. Determination of Sample Size A sample size of approximately 1500 patients is required to achieve 80% power at an alpha level of 0.05 using a chi-squared test of the null hypothesis that the mortality rates are equal in the 2 treatment groups. The assumptions that underlie the sample size calculations are based upon analyses of results from the PROWESS database. In PROWESS, the placebo mortality rate for patients with septic shock at baseline was approximately 35% and treatment with drotrecogin alfa (activated) was associated with a 20% relative risk reduction. Based on these data, it was assumed that the placebo mortality rate is 35% in patients with septic shock and that drotrecogin alfa (activated) is associated with a 20% relative risk reduction, resulting in a drotrecogin alfa (activated) mortality rate of 28%.
8.1.1. Resizing the Study Due to uncertainty in the mortality rate of patients with septic shock because of changes in the standard of care as well as the possibility that some patients may opt out of their randomly assigned therapy, the sponsor, in conjunction with the steering committee, may choose to increase the sample size during the course of the study if the blinded mortality rate is lower than expected or if there is a greater-than-anticipated number of patients for whom study drug is permanently discontinued due to disease progression/lack of improvement and therapy with commercial drotrecogin alfa (activated) is initiated (opt- out patients). The maximum adjustment to the sample size will be 500 patients for a total maximum sample size of 2000 patients. Mortality rate. After approximately one-half of the patients in the study have been enrolled, the blinded mortality rate will be computed. This calculation will be based upon summary data that have been aggregated across the 2 treatment groups. If the estimate of the overall mortality rate is less than 30%, the total sample size may be increased by reconsidering the initial assumptions surrounding the mortality rate in the placebo group and the size of the anticipated treatment benefit. Under the initial assumptions, the overall mortality rate was expected to be 31.5%. Opt-out rate. After approximately one-half of the patients in the study have been enrolled, the blinded opt-out rate will be computed. This calculation will be based upon summary data that have been aggregated across the 2 treatment groups. If the estimate of the opt-out rate is greater than or equal to 3%, the total sample size may be increased. Recalculation of the sample size will be based upon the observed opt-out rate and upon assumptions surrounding the mortality rate and treatment benefit in placebo patients who opt out of their randomly assigned therapy and receive drotrecogin alfa (activated). The purpose behind the augmentation of the sample size is to maintain the nominal statistical power of the study in the event that some placebo patients actually receive commercial drotrecogin alfa (activated).
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 40
8.2. Statistical and Analytical Plans
8.2.1. General Considerations Statistical analysis of the data from this study will be the responsibility of Lilly or designee. The efficacy analyses will be conducted on an ITT basis unless otherwise specified. The ITT population for this study will consist of all randomly-assigned patients, regardless of whether the patient received study drug. An ITT analysis is an analysis of data by the treatment groups to which patients are assigned by random allocation even if the patient does not receive the correct treatment or otherwise does not follow the protocol. Efficacy analyses will also be performed for all treated patients, the subset of patients in the ITT population who receive study drug for any length of time. Safety analyses will be performed for all treated patients. All tests of treatment effects will be conducted at a two-sided alpha level of 0.05 unless otherwise stated. The Statistical Analysis Plan (SAP) and List of Analyses will include a comprehensive description of the statistical methods and reports to be included in the final study report. Since no member of the Lilly clinical team will be unblinded to the clinical data before completion or termination of the study, all analyses specified in the SAP are considered prospectively defined. Any change to the data analysis methods described in the protocol will require an amendment ONLY if it changes a principal feature of the protocol. Any other change to the data analysis methods described in the protocol, and the justification for making the change, will be described in the clinical study report. Additional exploratory analyses of the data will be conducted as deemed appropriate. Data for qualitative variables will be presented as incidence rates (total number of patients, number of events, and percent). For qualitative variables, treatment groups will be compared using chi-square and Cochran-Mantel-Haenszel tests. Relative risks and confidence intervals will be calculated using the logit adjusted relative risk method. Data for continuous variables will be summarized using measures of central tendency and dispersion. Statistical tests for continuous variables will be performed using analysis of variance (ANOVA) based on ranked and unranked data (Snedecor and Cochran 1989). With the exception of the primary efficacy analyses, two-sided 5% significance levels and 95% confidence intervals will be used for all efficacy and safety analyses. The two- sided alpha level for the primary analysis will be adjusted to account for the planned interim analyses (Section 8.2.8). Patients with unknown survival status will be excluded from all landmark analyses of mortality. Patients with unknown survival status will be censored at the last date for which the patient was known to be alive or in the study hospital for all survival analyses. In longitudinal analyses of organ function and central laboratory data, the last observation carried forward (LOCF) method of imputation will be used. No adjustments for multiple comparisons will be made.
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 41
8.2.2. Patient Disposition Differences between the treatment groups in the frequencies with which each reason for discontinuation is observed will be summarized and presented. The data will be described using incidence rates (number of patients, number of events, and percent). Treatment comparisons will be performed using chi-square tests.
8.2.3. Patient Characteristics Listings and summary reports of baseline characteristics will be produced. The variables evaluated will include gender, age, age classification, origin, country, region, patient location prior to hospitalization, patient history (hypertension, coronary artery disease, congestive cardiomyopathy, immunodeficiency, stroke, deep vein thrombosis or pulmonary embolism, thrombophilia, diabetes mellitus, pancreatitis, chronic liver disease, chronic obstructive pulmonary disease, chronic renal disease, malignancy, recent trauma, and recent surgery), baseline APACHE II score, APACHE II class (<25, 25), APACHE II Acute Physiology Score, APACHE II Chronic Health Points, Glasgow Coma score, organ dysfunction criteria status for respiratory, renal, hematology, and metabolic acidosis; number of organ dysfunction criteria met; time from onset of septic shock to start of study drug; volume of intravenous fluids received at baseline, presumed or known site of infection; source of infection; type of infecting agent; baseline central laboratory values, baseline mechanical ventilation status; vasopressor type and dose; baseline renal replacement therapy status; baseline steroid exposure; and baseline heparin exposure. Two-sided p-values from chi-square and ANOVA tests will be used to summarize the comparability of the treatment groups with respect to these factors.
8.2.4. Primary Outcome and Methodology The primary efficacy analysis will be the comparison of 28-day all-cause mortality in the drotrecogin alfa (activated) and placebo treatment groups for the ITT population. Patients will be classified as “alive at Study Day 28” or, if dead, “dead at Study Day 28,” regardless of cause of death. The 28-day time point will occur 672 hours from randomization. Treatment comparisons will be performed using a chi-square test. Relative risk and odds ratio estimates with associated 95% confidence intervals will be presented. Survival analyses will also be performed. Differences between the drotrecogin alfa (activated) and placebo treatment groups in the time to death from randomization through 28 days will be assessed using a log-rank test. Survival curves will be produced using the method of Kaplan and Meier (Kaplan and Meier 1958). An analysis of 28-day mortality adjusted for independent predictors of mortality, such as age, APACHE II score, and protein C activity level, will also be conducted.
8.2.5. Efficacy Analyses The following secondary efficacy analyses will be conducted.
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 42
Twenty-eight-day mortality by protein C class. Analyses of mortality will be conducted in patients with severe protein C deficiency. Patients will be classified as severely deficient in protein C if their baseline protein C level is less than or equal to half the lower limit of normal. Organ function. Measures of organ function will be assessed at baseline and during the study drug infusion. The data will be summarized using measures of central tendency and dispersion. Statistical tests for continuous variables will be performed using ANOVA based on ranked and unranked data. Analyses of change from baseline, percent changes from baseline, and symmetric percent changes from baseline will be performed for each scheduled reference time. Symmetric percent changes will be computed using the method of Berry and Ayers (2006). Long-term mortality. Survival status will be assessed at Study Day 90 and Study Day 180. Patients will be classified as “alive at Study Day 90 (or 180)” or, if dead, “dead at Study Day 90 (or 180).” Because some patients will be lost to follow-up and therefore censored, mortality rates will be estimated using the method of Kaplan and Meier. Differences between drotrecogin alfa (activated) and placebo in mortality rates at these landmarks will be evaluated using the assumption of asymptotic normality. Standard errors of the mortality estimates within each treatment group will be estimated using Greenwood’s formula. Estimates of relative risks and odds ratios and the corresponding 95% confidence intervals will be presented. The difference between the drotrecogin alfa (activated) and placebo groups in the time to death from the start of the study drug infusion to Study Day 90 (or Study Day 180) will be assessed using a log-rank test. Survival curves will be constructed using the method of Kaplan and Meier. Quality of life. Measures of quality of life (Euro-QoL-5D and SF-12) will be assessed at baseline and Study Days 28, 90, and 180 and will be compared between the 2 treatment groups. The following additional efficacy analyses will also be performed: Sequential Organ Failure Assessment. Each organ system (cardiovascular, hematology, hepatic, renal, respiratory) will be scored using the SOFA methodology. For analysis, a patient will receive a score of 0, 1, 2, 3, or 4 on each day (Study Days 1 through 7, Study Day 14, and Study Day 28). Mean changes in organ function scores over time and percentages of patients whose organ function has resolved will be compared between treatment groups. Hospital resource utilization. Days on vasopressors, mechanical ventilation, and renal replacement therapy and days in the ICU and in the study hospital will be collected while the patient is alive and in the study hospital.
8.2.6. Safety Analyses All comparisons of safety-related data across treatment groups will be performed on the ITT population. For qualitative variables, such as adverse events, data will be
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 43 summarized as incidence rates (number of patients, number of events, and percent). Incidence rates in the 2 treatment groups will be compared using chi-square tests. Analyses of adverse events will be presented for Study Days 0 through 6 and Study Days 0 through 28. Laboratory data. Continuous laboratory and biomarker data will be summarized using measures of central tendency and dispersion. Statistical tests for continuous variables will be performed using ANOVA based on ranked and unranked data. Analyses of change from baseline, percent change from baseline, and symmetric percent change from baseline will be performed for each postbaseline data point.
8.2.7. Subgroup Analyses Subgroup analyses of 28-day all-cause mortality will be performed for the ITT population. Subgroup analyses of serious adverse events and serious bleeding events will be performed the population of all treated patients. The primary purpose of the subgroup analyses is to examine the consistency of treatment effects across subgroups. A second purpose is to identify subgroups that merit further exploratory analysis. Within each level of each subgroup factor, treatments will be compared using chi-square (nonstratified) tests. Relative risks and 95% confidence intervals will be calculated using the logit adjusted relative risk method. Since mortality rates may vary across the levels of the subgroup factors, adjusted treatment comparisons will be assessed using Cochran- Mantel-Haenszel tests. Adjusted relative risks and 95% confidence intervals will be calculated using the logit adjusted relative risk method. Breslow-Day tests for homogeneity of odds ratios across strata will also be performed. For subgroup analyses, Breslow-Day p-value <0.10 will be considered significant. A result for a given subgroup will be defined as consistent with the overall study results if the 95% confidence interval around the relative risk in that subgroup contains the point estimate of the relative risk for the overall study. Subgroups to be investigated for 28-day all-cause mortality, serious adverse events, and serious bleeding events include the following: gender, age classification, origin, region, APACHE II class (<25, 25), number of organ dysfunctions at baseline, organ dysfunction class (single, multiple), baseline vasopressor type and dose, lactate level, recent surgery, baseline steroid exposure, baseline heparin exposure, time from onset of septic shock to start of study drug class, time from onset of first sepsis-induced organ dysfunction to the start of study drug class, presumed or known site of infection, source of infection (community, nosocomial), type of infecting agent, mechanical ventilation status, and baseline protein C class.
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 44
8.2.8. Interim Analyses Two interim analyses are planned for this study. These interim analyses will be conducted under the auspices of an external and independent DMC to minimize the operational and statistical bias that result from performing interim analyses. The purpose of the DMC is to advise Lilly regarding the continuing safety of study participants and the continuing validity and scientific merit of the study. Only the DMC is authorized to evaluate unblinded interim efficacy and safety analyses. Study sites will receive information about interim results ONLY if they need to know for the safety of their patients. The DMC will be composed of 1 statistician and 5 physicians with relevant critical care, medical, or medical/clinical study ethics experience. All members will be voting members and DMC membership will cover the duration of the study. All members of the DMC are external to Lilly. The first interim analysis will occur after approximately one-third of patients have completed 28 days of follow-up; the second will occur after approximately two-thirds of patients have completed 28 days of follow-up. If a decision is made to increase the sample size of the study, interim analyses will be inserted in such a way that approximately 500 patients are enrolled between each contiguous pair of interim analyses. Since the first interim analysis is scheduled to take place after 28-day outcomes have been obtained for 500 patients, the additional interim analyses will be conducted at regular intervals between 500 and the new sample size, and the interim analysis that was originally scheduled to take place after 28-day outcomes had been obtained for 1000 patients will be eliminated. For example, if the blinded mortality rate is observed to be 28% after 750 patients have completed 28 days of follow-up, and the sample size is increased to 1940 patients, the estimated number of patients who would be enrolled after the first interim analysis would be 1940 – 500 = 1440. In this case, the number of interim analyses that would occur after the first look would be calculated by taking the integer portion of the fraction 1440/500 or int(2.88) = 2. Each of these 2 interim analyses would be triggered once 28-day outcomes have been obtained for an additional 480 patients (1440/number of inserted interim analyses + 1). Thus, the 2 inserted interim analyses would take place after 28-day outcomes have been recorded for 980 and 1460 patients, respectively. Alpha-spending procedures, such as those described by Lan and DeMets (1983), will be used to maintain an overall two-sided Type I error of 0.05. The objective of the DMC for the first interim analysis is to recommend whether to terminate enrollment in the study for safety concerns based on prospectively defined guidelines. Because an examination of mortality rate will be a part of the safety review, there will be an alpha spend at the first interim analysis. However, the sponsor has no plans to stop the study for positive efficacy at the first interim analysis. The objective of the second interim analysis is to recommend whether to terminate enrollment in the study for safety concerns, efficacy, or futility based on prospectively defined guidelines.
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 45
The prescription for alpha spending will follow accepted statistical practices, such as the methodology of O’Brien and Fleming as implemented by Lan and DeMets (Lan and DeMets 1983; DeMets et al. 1995). The alpha spend at the first interim analysis and the guideline for stopping due to efficacy at the second interim analysis will ensure an overall false positive (one-sided) error rate less than 2.5%. The final stopping guidelines will be decided in consultation with the DMC committee members and documented in the DMC Charter. The DMC Charter will be submitted to regulatory agencies before the first patient visit. The prospectively defined interim analysis plan will be executed by a group of independent statisticians at a CRO who will be separated by a firewall from the statisticians at the same CRO who will be responsible for the analysis of data at the conclusion of the study. This group of independent statisticians will present interim results to the DMC. Individuals responsible for data management activities and the generation of datasets for interim reporting will not have access to patient treatment assignments. Patient treatment assignments will be provided to the independent statistical group prior to each interim analysis. The independent statistical group will merge the interim datasets and the data set that contains patient treatment assignments to execute the interim analysis plan.
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 46
9. Informed Consent, Ethical Review, and Regulatory Considerations
9.1. Informed Consent The investigator is responsible for ensuring that the patient understands the risks and benefits of participating in the study, including answering any questions the patient may have throughout the study and sharing in a timely manner any new information that may be relevant to the patient's willingness to continue his or her participation in the trial. The informed consent document will be used to explain the risks and benefits of study participation to the patient in simple terms before the patient is entered into the study, and to document that the patient is satisfied with his or her understanding of the risks and benefits of participating in the study and desires to participate in the study. The investigator is responsible for ensuring that informed consent is given by each patient or legal representative. This includes obtaining the appropriate signatures and dates on the informed consent document prior to the performance of any protocol procedures and prior to the administration of study drug. As used in this protocol, the term "informed consent" includes all consent and assent given by patients or their legal representatives.
9.2. Ethical Review Lilly must agree with all informed consent documents before they are submitted to the ethical review board and are used at investigative sites. All informed consent documents must be compliant with the International Conference on Harmonisation guideline on good clinical practice. Informed consent obtained under special circumstances may occur only if allowed by local laws and regulations and performed in accordance with a written process approved by Lilly. Documentation of ethical review board approval of the protocol and the informed consent document must be provided to Lilly before the study may begin at the investigative sites. The ethical review board will review the protocol as required. Any member of the ethical review board who is directly affiliated with this study as an investigator or as site personnel must abstain from the vote on the approval of the protocol. The study site’s ethical review board should be provided with the following: the current Investigator’s Brochure or package labeling and updates during the course of the study informed consent document relevant curricula vitae
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 47
9.3. Regulatory Considerations This study will be conducted in accordance with the ethical principles that have their origin in the Declaration of Helsinki and that are consistent with good clinical practices and the applicable laws and regulations. The investigator, head of the medical institution, or designee will promptly submit the protocol to applicable ethical review boards. Drotrecogin alfa (activated) is being studied in the United States (US) under a US Investigational New Drug (IND) application. The US IND number is BB-IND 5919. All or some of the obligations of the sponsor will be assigned to a CRO. An identification code assigned by the investigator to each patient will be used in lieu of the patient's name to protect the patient's identity when reporting adverse events and/or other trial-related data.
9.3.1. Investigator Information Physicians who are qualified by training and experienced in the practice of critical care medicine will participate as investigators in this clinical study.
9.3.2. Protocol Signatures After reading the protocol, each principal investigator will sign the protocol signature page and send a copy of the signed page to a Lilly representative.
9.3.3. Final Report Signature The clinical study report coordinating investigator will sign the final clinical study report for this study, indicating agreement that, to the best of his or her knowledge, the report accurately describes the conduct and results of the study.
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 48
10. References
Abraham E, Reinhart K, Svoboda P, Seibert A, Olthoff D, Dal Nogare A, Postier R, Hempelmann G, Butler T, Martin E, Zwingelstein C, Percell S, Shu V, Leighton A, Creasy AA. 2001. Assessment of the safety of recombinant tissue factor pathway inhibitor in patients with severe sepsis: a multicenter, randomized, placebo-controlled, single-blind, dose-escalation study. Crit Care Med 29(11):2081–2089. Abraham E, Laterre PF, Garg R, Levy H, Talwar D, Trzaskoma BL, Francois B, Guy JS, Brueckmann M, Rea-Neto A, Rossaint R, Perrotin D, Sablotzki A, Arkins N, Utterback BG, Macias WL, Administration of Drotrecogin Alfa (Activated) in Early Stage Severe Sepsis (ADDRESS) Study Group. 2005. Drotrecogin alfa (activated) for adults with severe sepsis and a low risk of death. N Engl J Med 353:1332–1341. Annane D, Sebille V, Charpentier C, Bollaert PE, Francois B, Korach JM, Capellier G, Cohen Y, Azoulay E, Troche G, Chaumet-Riffaut P, Bellissant E. 2002. Effect of treatment with low doses of hydrocortisone and fludrocortisone on mortality in patients with septic shock. JAMA 288(7):862–871. Bernard GR, Vincent JL, Laterre PF, LaRosa SP, Dhainaut JF, Lopez-Rodriguez A, Steingrub JS, Garber GE, Helterbrand JD, Ely EW, Fisher CJ Jr. 2001. Efficacy and safety of recombinant human activated protein C for severe sepsis. N Engl J Med 344:699–709. Berry AD, Ayers GD. 2006. Symmetrized percent change for treatment comparisons. Am Stat 60:27–31. Brandtzaeg P, Sandset PM, Joo GB, Ovstebo R, Abildgaard U, Kieruef P. 1989. The quantitative association of plasma endotoxin, antithrombin, protein C, extrinsic pathway inhibitor, and fibrinopeptide A in systemic meningococcal disease. Thromb Res 55:459–470. Brooks R. 1996. EuroQol: the current state of play. Health Policy 37:53–72. Brunkhorst F, Sakr Y, Hagel S, Reinhart K. 2007. Protein C concentrations correlate with organ dysfunction and predict outcome independent of the presence of sepsis. Anesthesiology 107:15–23. [CHMP] Committee for Medicinal Products for Human Use. Guideline on Clinical Investigation of Medicinal Products for the Treatment of Sepsis. Available at http://www.emea.europa.eu/pdfs/human/ewp/471303en.pdf. Accessed 6 August 2007. Cole L, Bellomo R, Hart G, Journois D, Davenport P, Tipping P, Ronco C. 2002. A phase II randomized, controlled trial of continuous hemofiltration in sepsis. Crit Care Med 30(1):100–106. DeMets DL, Fleming TR, Whitley RJ, Childress JF, Ellenberg SS, Foulkes M, Mayer KH, O’Fallon J, Pollard RB, Rahal JJ, Sande M, Straus S, Walters L, Whitley- Williams P. 1995. The data and safety monitoring board and acquired immune deficiency syndrome (AIDS) clinical trials. Control Clin Trials 16:408–421.
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 49
EuroQol Group. 1990. EuroQol – a new facility for the measurement of health-related quality of life. Health Policy 16:199–208. Fijnvandraat K, Derkx B, Peters M, Bijlmer R, Sturk A, Prins MH, van Deventer SJ, ten Cate JW. 1995. Coagulation activation and tissue necrosis in meningococcal septic shock: severely reduced protein C levels predict a high mortality. Thromb Haemost 73(1):15–20. Fourrier F, Chopin C, Goudemand J, Hendrycx S, Caron C, Rime A, Marey A, Lestavel P. 1992. Septic shock, multiple organ failure, and disseminated intravascular coagulation: compared patterns of antithrombin III, protein C and protein S deficiencies. Chest 101:816–823. Geerts WH, Pineo GF, Heit JA, Bergquist D, Lassen MR, Colwell CW, Ray JG. 2004. Prevention of venous thromboembolism. The Seventh ACCP Conference on Anthithrombotic and Thrombolytic Therapy. Chest 126:338S–400S Gupta A, Berg DT, Gerlitz B, Richardson MA, Galbreath E, Syed S, Sharma AC, Lowry SF, Grinnell BW. 2007. Activated protein C suppresses adrenomedullin and ameliorates lipopolysaccharide-induced hypotension. Shock Epub 2007 Jun 7. Hazelzet JA, Van der Voort E, Lindemans J, Ter Heerdt PGJ, Neijens HJ. 1994. Relation between cytokines and routine laboratory data in children with septic shock and purpura. Intensive Care Med 20:371–374. Hesselvik JF, Malm J, Dahlback B, Blomback M. 1991. Protein C, protein S and C4b- binding protein in severe infection and septic shock. Thromb Haemost 65:126–129. Kalil AC, Coyle SM, Um JY, LaRosa SP, Turlo MA, Calvano SE, Sundin DP, Nelson DR, Lowry SF. 2004. Effects of drotrecogin alfa (activated) in human endotoxemia. Shock 21(3):222–229. Kaplan EL, Meier P. 1958. Nonparametric estimation from incomplete observations. JASA 53:456–481. Kirschenbaum LA, Lopez WC, Ohrum P, Tsen A, Khazin J, Astiz ME. 2006. Effect of recombinant activated protein C and low-dose heparin on neutrophil-endothelial cell interactions in septic shock. Crit Care Med 34(8):2207–2212. Lan KKG, DeMets DL. 1983. Discrete sequential boundaries for clinical trials. Biometrika 70:659-663. Leclerc F, Hazelzet J, Jude B, Hofhuis W, Hue V, Martinot A, Van der Voort E. 1992. Protein C and S deficiency in severe infectious purpura of children: a collaborative study of 40 cases. Intensive Care Med 18:202–205. Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G; SCCM/ESICM/ACCP/ATS/SIS. 2003. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Congress. Crit Care Med 31(4): 1250–1256. Mesters RM, Helterbrand J, Utterback BG, Yan B, Chao YB, Fernandez JA, Griffin JH, Hartman DL. 2000. Prognostic value of protein C concentrations in neutropenic patients at high risk of severe septic complications. Crit Care Med 28(7):2209–2216.
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 50
Monnet X, Lamia B, Anquel N, Richard C, Bonmarchand G, Teboul JL. 2005. Rapid and beneficial hemodynamic effects of activated protein C in septic shock patients. Intensive Care Med 31(11):1573–1576. Nadel S, Goldstein B, Williams MD, Dalton H, Peters M, Macias WL, Abd-Allah SA, Levy H, Angle R, Wang D, Sundin DP, Giroir B, for the Researching severe sepsis and organ dysfunction in children: a global perspective (RESOLVE) study group. 2007. Drotrecogin alfa (activated) in children with severe sepsis: a multicentre phase III randomized controlled trial. Lancet 369:836–843. Peters M, Fijnvandraat K, Derkx B, Stassen M, van Deventer SJH. 1993. Severely reduced protein C levels predict a high mortality in meningococcal shock. Thromb Haemost 65:A2337. Philippe J, Offner F, Leroux-Roels G, Vogelaers D, Baele G. 1989. Plasminogen activator inhibitor-1, protein C, antithrombin III and tissue plasminogen activator activities in the early phase of septic shock. Thromb Haemost 65:A1836. Piette WW, Shasby DM, Kealey GP, Olson JD. 1993. Retiform purpura is a sign of severe acquired protein C deficiency and risk of progression to purpura fulminans in sepsis and disseminated intravascular coagulation. Clin Res 41:253A. Powars D, Larsen R, Johnson J, Hulbert T, Sun T, Patch M, Francis R, Chan L. 1993. Epidemic meningococcemia and purpura fulminans with induced protein C deficiency. Clin Infect Dis 17:254–261. Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M, Early Goal-Directed Therapy Collaborative Group. 2001. Early goal- directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 345(19):1368–1377. Roman J, Velasco F, Fernandez F, Fernandez M, Villalba R, Rubin V, Torres A. 1992. Protein C, protein S, and C4B-binding protein in neonatal severe infection and septic shock. J Perinat Med 20:111–116. Sheth SB, Carvalho AC. 1991. Protein S and C alterations in acutely ill patients. Am J Hematol 36(1):14–19. Shorr AF, Bernard GR, Dhainaut JF, Russell JR, Macias WL, Nelson DR, Sundin DP. 2006. Protein C concentrations in severe sepsis: an early directional change in plasma levels predicts outcome. Crit Care 10(3):R92. Epub 2006 Jun 15. Snedecor GW, Cochran WG. 1989. Statistical Methods. 8th Edition. Iowa State University Press. Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, Reinhart CK, Suter PM, Thijs LG. 1996. The SOFA (Sepsis-Related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the working group on sepsis- related problems of the European Society of Intensive Care Medicine. Intensive Care Med 22:707–710. Vincent JL, Angus DC, Artigas A, Kalil A, Basson BR, Jamal HH, Johnson G 3rd, Bernard GR, Recombinant Human Activated Protein C Worldwide Evaluation in
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 51
Severe Sepsis (PROWESS) Study Group. 2003. Effects of drotrecogin alfa (activated) on organ dysfunction in the PROWESS trial. Crit Care med 31(3):834–840. Ware J, Kosinski M, Keller SD. 1996. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care 34:220–233. Warren BL, Eid A, Singer P, Pilay SS, Carl P, Novak I, Chalupa P, Atherstone A, Penzes I, Kubler A, Knaub S, Keinecke HO, Heinrichs H, Schindel F, Juers M, Bone RC, Opal SM; KyberSept Trial Study Group. 2001. Caring for the critically ill patient. High-dose antithrombin III in severe sepsis: a randomized controlled trial. JAMA 286(15):1869– 1878. Williams MD, Macias W, Rustige J. 2007. Safety of drotrecogin alfa (activated): a fair comparison required consistent definitions. Intensive Care Med 33:1487–1488.
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 52
Protocol Attachment EVDP.1. Study Schedule
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential
Study Schedule, Protocol F1K-MC-EVDP
Page 53 Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Pretreatment Treatment Posttreatment Follow-Up Visit 1 Visit 2 Visit 3 Visit 4 Visit 5 Study Day –1a 0a 1 2 3 4 5 6 7 8-14 15-28 90 180 Discharge Eligibility assessment X Informed consent X Baseline Assessments X APACHE II X Administer study drugb <======> Adverse events X X X X X X X X X X X Quality of life X Xc X X Resource utilization X X X X X X X X X X X X Survival status Xc X X Hospital discharge/death date X Patient location X Xc X X X Vital signsd X X X X X X X X Urine output X X X Glasgow Coma Scale X X Xe Xe Local laboratory tests: Pregnancy (if applicable) X Lactatef X X X Hematologyg X X Xe Xe Creatinineh X X X X Central laboratory tests: Chemistryg X X Xe Xe Coagulationg X X Xe Xe Protein C X X X X X X X X Xe Xe PAI-1 X X
Page 54 Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential (continued)
Study Schedule, Protocol F1K-MC-EVDP (concluded)
Page 55 Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Pretreatment Treatment Posttreatment Follow-Up Visit 1 Visit 2 Visit 3 Visit 4 Visit 5 Study Day –1a 0a 1 2 3 4 5 6 7 8-14 15-28 90 180 Discharge Central laboratory tests: Microalbumin (urine) X X X Creatinine (urine) X X X Heparin discontinuation central laboratory tests:i F1.2 X X X X X TATc X X X X X Record if available: Bicarbonate (venous) X X X X X X X X Arterial blood gask X X X X X X X X P/F and S/F ratiosl X X X Central venous oxygen X X X saturationk Ventilator settingsk X X X X X X X SOFA score X X X X X X X X Xe Xe Abbreviations: APACHE II = Acute Physiology and Chronic Health Evaluation II; char. = characteristics; F1.2 = prothrombin fragment 1.2; QoL = quality of life; PAI-1 = plasminogen activator inhibitor 1; SOFA = Sequential Organ Failure Assessment; TATc = thrombin-antithrombin complex. a The pretreatment period (Study Day –1) is defined as the time from the onset of vasopressor therapy to the start of the study drug infusion (maximum of 24 hours). Study Day 0 is defined as the time from the start of the infusion to midnight of that day. Study Day 1 is the calendar day after the start of the infusion. b Study drug is administered for 96 hours 1 hour. The infusion may extend into Study Day 5 or 6 because of interruptions in the infusion. c Survival status, patient location, and quality of life should be assessed on Study Day 28. d Record vital signs at baseline, every 6 hours for the first 48 hours after the start of the infusion, and daily on Study Days 3 through 6, if available. Vital signs include heart rate, blood pressure, and central venous pressure e Draw samples or perform assessment on Study Days 14 and 28. Footnotes continued on next page.
Page 56 Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Footnotes continued from previous page. f Measure every 6 hours during the first 24 hours after the start of the study drug infusion. g Refer to Attachment EVDP.2 for a list of analytes to be measured. h Draw samples at baseline and every 6 hours for the first 48 hours after the start of the infusion. i Draw blood samples only for patients who discontinue prophylactic heparin during the pretreatment period. Samples should be drawn just prior to the start of the infusion and every 12 hours for 72 hours after the start of the infusion. k Record the assessment closest to 8:00 am each day for patients receiving mechanical ventilation. Ventilator settings include FiO2, mean airway pressure, and plateau pressure. l Record measurement every 6 hours during the first 24 hours after the start of the study drug infusion, if available, for patients receiving mechanical ventilation.
Page 57 Page 58
Protocol Attachment EVDP.2. Clinical Laboratory Tests
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 59
Clinical Laboratory Tests
Central Laboratorya,b: Chemistry: Alanine aminotransaminase (ALT) Aspartate aminotransferase (AST) Sodium Potassium Chloride Albumin Bilirubin Blood urea nitrogen Creatinine Glucose (nonfasting) Coagulation: Activated partial thromboplastin time (APTT) Prothrombin time Microalbumin (urine) Creatinine (urine) Protein C Plasminogen activator inhibitor 1 (PAI-1) Prothrombin fragment 1.2 (patients who discontinue prophylactic heparin only) Thrombin-antithrombin complex (TATc) (patients who discontinue prophylactic heparin only) Local Laboratoryc: Creatinine Lactate Hematology: Hemoglobin Hematocrit Platelet count Leukocytes (WBC) Pregnancy test (females of childbearing age only; urine or serum) Abbreviations: ALT = alanine aminotransaminase; APTT = activated partial thromboplastin time; AST = aspartate aminotransferase; PAI-1 = plasminogen activator inhibitor 1; WBC = white blood cells. a Assayed by Lilly-designated laboratory. b Results will be confirmed by the central laboratory at the time of initial testing. c Local or investigator-designated laboratory.
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 60
Protocol Attachment EVDP.3. Noncardiovascular Organ Dysfunction Criteria
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 61
Use the following criteria to determine if the following sepsis-induced organ dysfunctions are present at baseline. Renal. Average urine output <0.5 mL/kg/h for 1 hour despite adequate fluid resuscitation. Adequate fluid resuscitation or adequate intravascular volume is defined as one or more of the following: (a) the administration of an intravenous fluid bolus (500 mL of crystalloid solution, 20 g of albumin, or 200 mL of other colloids administered over 30 minutes or less); (b) pulmonary arterial wedge pressure 12 mm Hg; or (c) central venous pressure 8 mm Hg.
Respiratory. Evidence of acute pulmonary dysfunction PaO2/FiO2 ≤250 and, if measured, a pulmonary capillary wedge pressure not suggestive of central volume overload. If the lung is also the suspected site of infection, the patient must have a PaO2/FiO2 ≤200. PaO2 altitude adjustment: 760 divided by barometric pressure multiplied by PaO2. Hematology. Platelet count <80,000/mm3 or a 50% decrease in platelet count from the highest value recorded over the 3 days prior to study entry. Unexplained metabolic acidosis. Defined by (1) pH ≤7.30 or base deficit ≥5.0 mEq/L and (2) a plasma lactate level >1.5 times the upper limit of normal for the reporting laboratory. Measurement of pH or base deficit and lactate level should occur within a clinically relevant time interval such that a causal relationship exists between the measured values.
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 62
Protocol Attachment EVDP.4. Guidelines for Evidence of Infection
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 63
Guidelines for evidence of infection: Lower respiratory tract and other infections of the thorax: (1) Chest x-ray or CT scan showing the presence of a new or progressive infiltrate, consolidation, cavitation, or pleural effusion, and a clinical presentation consistent with pneumonia or empyema. Patients with nosocomial pneumonia (defined as pneumonia diagnosed 72 hours or more after admission to a healthcare facility) must, in addition, have a microbiological diagnosis, such as positive culture, gram stain, antigen testing, made using protected specimen brush/bronchoalveolar lavage or endotracheal aspirate. (2) Mediastinitis after cardiothoracic surgery verified on surgical re-exploration or clinical signs of mediastinitis after esophageal perforation. Abdominal infection: (1) Perforated viscus with either localized peritonitis, for example, abdominal abscess, or diffuse peritonitis, confirmed surgically or with percutaneous drainage. (2) Intestinal gangrene requiring resection. (3) Clinical signs of cholangitis (such as fever, right upper quadrant pain, increased bilirubin). (4) Clostridium difficile toxin positive with evidence of colon dilation. Skin or soft tissue infection: Acute onset infection of the skin, such as erysipelas, or infection involving deeper soft tissue. Purpura fulminans: extensive petechiae or ecchymosis without a known underlying hematological disease or other likely explanation for clinical findings. Bacterial meningitis: cerebrospinal fluid analyses and a clinical presentation consistent with bacterial meningitis. Pyelonephritis: clinical signs of pyelonephritis (for example, flank pain) with a positive test for granulocyte esterase or nitrate in urine, or a positive culture (defined as >105 CFU/mL) from a clean-catch midstream or catheterization urine specimen. Positive specimens from a chronic indwelling urinary catheter are excluded. Bloodstream infections: isolation of a pathogen in one or more blood cultures drawn peripherally, or from a central venous catheter/port in place <48 hours.
The following are not considered evidence of infection: Fever of unknown origin. Blood cultures with a microorganism usually regarded as a common skin contaminant, such as diphtheroids, bacillus species, propionibacterium species, coagulase-negative staphylococci, or micrococci. Suspicion of peritonitis by clinical examination only.
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 64
Postoperative hypotension and/or fever without a verified infectious focus. High serum levels of C-reactive protein, procalcitonin, or other inflammatory markers. Protozoal or helminthic infections.
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 65
Protocol Attachment EVDP.5. Guidelines for Enrollment
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 66
Use the following guidelines for patients who are not expected to survive 28 days or who are likely to have limitations put on their life support given their preexisting, uncorrectable medical condition. Exclude the following patients: New York Heart Association class IV patients. Patients with cardiac arrest requiring CPR within the past 30 days. Patients with biopsy proven cirrhosis and documented portal hypertension; episodes of past upper gastrointestinal bleeding attributed to portal hypertension; or prior episodes of hepatic failure/encephalopathy/coma. Patients with vascular disease resulting in severe exercise restriction (that is, unable to climb stairs or perform household duties), or chronic restrictive or obstructive pulmonary disease that also results in severe exercise restriction, or documented chronic hypoxia, hypercapnia, secondary polycythemia, severe pulmonary hypertension (mean pulmonary artery pressure >40 mm Hg), or respirator dependency. Patients with end-stage neurological disorders (for example, amyotrophic lateral sclerosis). For patients with poorly controlled neoplasms or patients currently receiving chemotherapy, use the following guidelines: Bladder Cancer: Exclude Stage III and IV Breast Cancer: Exclude Stage III and IV Central Nervous System Cancer: Exclude all Colorectal Cancer: Exclude Stage III and IV Cervical Cancer: Exclude Stage III and IV Hepatic Cancer: Exclude all Leukemia, Acute Myelocytic: Exclude unless in remission; exclude if hematopoietic stem cell transplant is planned or has been performed within the month prior to study entry Leukemia, Acute Lymphocytic: Exclude unless in remission; exclude if hematopoietic stem cell transplant is planned or has been performed within the month prior to study entry Leukemia, Chronic Myelocytic: Exclude blast or accelerated phase Leukemia, Chronic Lymphocytic: Allowed unless anemia, thrombocytopenia, or organomegaly present Lung Cancer: Exclude Stage III and IV; Stage I and II allowed if curative resection done
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 67
Lymphoma, Non-Hodgkins: Exclude if Intermediate or High Grade or hematopoietic stem cell transplant is planned or has been performed within the month prior to study entry Lymphoma, Hodgkins: Exclude Stage IIIb and IV Multiple Myeloma: Exclude unless low tumor burden Pancreatic Cancer: Exclude all Prostate Cancer: Exclude if Stage T3 or T4 Renal Cancer: Enroll only if cancer is confined to capsule Skin Cancer: Exclude melanoma if evidence of metastasis Stomach Cancer: Exclude Stage III and IV; Stage I and II allowed if curative resection done
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 68
Protocol Attachment EVDP.6. Estimation of Baseline Creatinine Level
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential Page 69
The MDRD (Modification of Diet in Renal Disease Study) Equation or Cockcroft-Gault Equation can be used to estimate baseline creatinine. Both of these equations rely on an estimation of normal renal function prior to the onset of septic shock, and, thus, patients must be screened thoroughly for the possibility of underlying renal disease. Underlying renal disease would cause the estimation of renal function (creatinine) to be incorrect, and, thus, if there is any possibility of underlying renal disease, other evidence of hypoperfusion (oliguria, metabolic acidosis, or acute hepatic dysfunction) should be used for inclusion in the study.
MDRD Equation As recommended by the ADQI workgroup (assuming an average glomerular filtration rate of 75 mL/min in this age group:
Estimated baseline creatinine Black Males Other Males Black Females Other Females Age (years) mg/dL (mol/L) mg/dL (mol/L) mg/dL (mol/L) mg/dL (mol/L) 20–24 1.5 (133) 1.3 (115) 1.2 (106) 1.0 (88) 25–29 1.5 (133) 1.2 (106) 1.1 (97) 1.0 (88) 30–39 1.4 (124) 1.2 (106) 1.1 (97) 0.9 (80) 40–54 1.3 (115) 1.1 (97) 1.0 (88) 0.9 (80) 55–65 1.3 (115) 1.1 (97) 1.0 (88) 0.8 (71) >65 1.2 (106) 1.0 (88) 0.9 (80) 0.8 (71)
Estimated glomerular filtration rate = 75 (mL/min per 1.73 m2) = 186 (serum creatinine [Scr]) – 1.154 (age) –0.203 (0.742 if female) (1.210 if black) = exp(5.228 – 1.154 ln[Scr] – 0.203 ln(age) – (0.299 if female) + (0.192 if black)
References: National Kidney Foundation. 2002. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 39(2 Suppl 1):S1–S266. Uchino S, Bellomo R, Goldsmith D, Bates S, Ronco C. 2006. An assessment of the RIFLE criteria for acute renal failure in hospitalized patients. Crit Care Med 34(7):1913–1917.
Cockcroft-Gault Equation
Creatinine clearance (mL/min) = (140 – age in years) actual weight (kg) serum creatinine (mol/L) Multiply the result by 1.2 for men Normal range is >90 mL/min, >1.5 mL/s
Drotrecogin Alfa (Activated) F1K-MC-EVDP Protocol Confidential