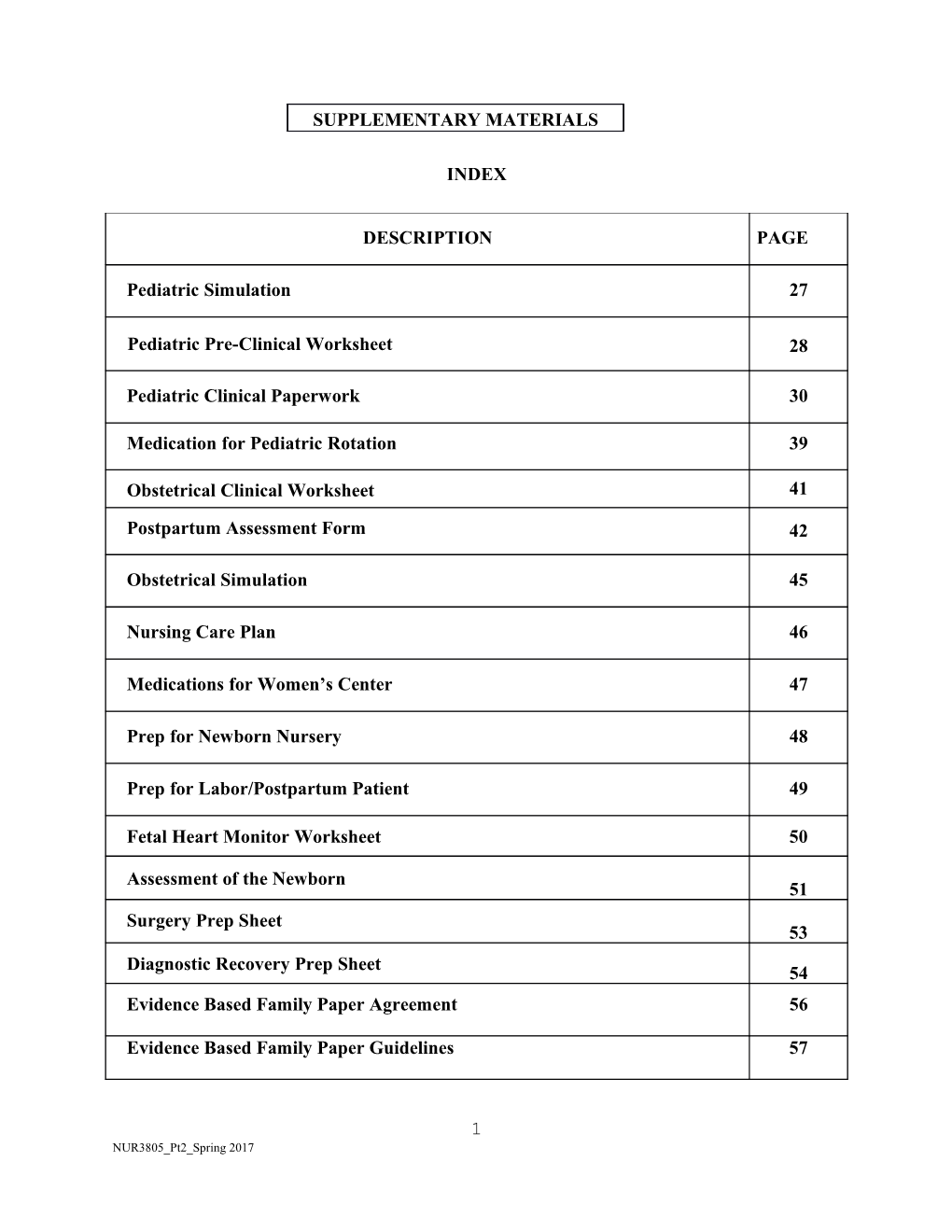
SUPPLEMENTARY MATERIALS
INDEX
DESCRIPTION PAGE
Pediatric Simulation 27
Pediatric Pre-Clinical Worksheet 28
Pediatric Clinical Paperwork 30
Medication for Pediatric Rotation 39
Obstetrical Clinical Worksheet 41
Postpartum Assessment Form 42
Obstetrical Simulation 45
Nursing Care Plan 46
Medications for Women’s Center 47
Prep for Newborn Nursery 48
Prep for Labor/Postpartum Patient 49
Fetal Heart Monitor Worksheet 50
Assessment of the Newborn 51 Surgery Prep Sheet 53
Diagnostic Recovery Prep Sheet 54 Evidence Based Family Paper Agreement 56
Evidence Based Family Paper Guidelines 57
1 NUR3805_Pt2_Spring 2017 Pediatric Simulation
Simulation 1
1. Complete Respiratory case study as assigned.
2. Complete Pain Scales worksheet and quiz as assigned.
3. Review Infant and Pediatric CPR.
4. Review and practice using SBAR with practitioner in simulation.
5. Discuss various respiratory medications and selected pediatric respiratory conditions.
6. Discuss various airways used in pediatrics (nasal and oral).
Simulation 2
1. Complete GI case study as assigned.
2. Review and define hypovolemic shock (risk factors, identification, and treatment).
3. Review Infant and Pediatric choking.
4. Discuss various types of shock most commonly seen in pediatrics.
5. Practice SBAR with practitioner in simulation.
6. Calculate the minimum 24 hour fluid requirement for pediatric patients under 70 kg.
Simulation 3
1. Complete a Cardiac case study as assigned.
2. View video(s) over various congenital cardiac conditions in pediatrics.
3. Practice CPR and introduce PALS in simulation setting with cardiac conditions.
4. Practice SBAR with practitioner in simulation.
5. Identify various cardiac rhythm strips.
6. Discuss various medications and administration methods used in the pediatric code setting.
2 NUR3805_Pt2_Spring 2017 ARKANSAS TECH UNIVERSITY Department of Nursing NUR 3805 – Practicum in Nursing II Pediatric Pre Clinical Worksheet
1. Read Chapters 34, 40 and 41. 2. Familiarize self with current immunization recommendations - Print and attach: http://www.cdc.gov/vaccines/recs/schedules/downloads/child/0-18yrs-pocket- pr.pdf 3. Create vital sign flashcards for normal temperature (rectal vs axillary), heart rate, respiratory rate and blood pressure in children for the following age groups: Newborn, < 2years, 2-6 years, 6-10 years, and 10+ years. 4. Review how to take a temperature with oral, rectal, and axillary thermometers. 5. List and describe Erikson’s psychosocial stages through adolescence. 6. Define the role of play therapy. Give appropriate examples of play for the hospitalized child for each of the age groups: (Infant, Toddler, Pre-school & School-age) 7. Develop communication skills with children of varying ages: You are administering a flu vaccination. How do you communicate this to an infant? A toddler? A pre-schooler? A school-age child? An adolescent? 8. Pain Scales: Print off a copy of following pain scales – FLACC, FACES, COMFORT and 0-10.
MEDICATIONS FOR PEDIATRIC ROTATION The following list includes some commonly prescribed pediatric medications. The student is required to prepare a completed medication sheet before their first day of pediatric practicum and maintain throughout the clinical rotation.
Acetaminophen Albuterol Ampicillin Ancef Ativan Claforan Ibuprofen Gentamycin Hyperal/TPN and Lipids Methadone Morphine Prelone Syrup/Prednisone Tabs Pulmicort Rifampin Rocephin
3 NUR3805_Pt2_Spring 2017 Singulair Solu-Medrol Q-Var Tobramycin Vancomycin Xopenex Zantac Zithromax Important Pediatric Measurement Conversions:
5cc = 1 teaspoon 3 tsp = 1 tablespoon 15 cc = 1 tablespoon
30 cc = 1 ounce 1 kg = 2.2 pounds 2.5 cm = 1 inch 1 mcg = 0.001mg 1mL = 1cc 1 gram = 1cc
Pediatric Dosage Calculation EXAMPLE: Amoxil 40mg/kg/day divided TID The patient weighs 15 kg. This drug comes in the concentration of 250mg/5cc. How many mg per dose? How many cc’s per dose? 40 mg x 15 kg = 600 mg per day 600 mg ÷ 3 = 200 mg per dose 200 mg ÷ 250 mg = 0.8 mg 0.8 mg x 5 cc = 4 cc per dose
4 NUR3805_Pt2_Spring 2017 Student Name:______
ARKANSAS TECH UNIVERSITY Department of Nursing NUR 3805 – Practicum in Nursing II Pediatric Clinical Paperwork
Patient Initials: ______Age: ______Male or Female
Allergy & Reactions: ______□NKA
Medical Diagnose(s) for this hospitalization: ______
Chronic Illness: ______□ N/A
Event(s) that brought patient to the hospital:
Birth History IF <2 years of age:
What is the expected outcome for this patient long term?
5 NUR3805_Pt2_Spring 2017 List all procedures this patient has had since admission (List most current for long term patients)
WEIGHT KG % Growth Chart HEAD CIRCUMFERENCE <2yo % Growth Chart HEIGHT/LENGTH % Growth Chart
6 NUR3805_Pt2_Spring 2017 NUTRITION
WHAT TYPE OF NUTRITION OR DIET IS THE PATIENT RECEIVING? BE SPECIFIC – FEEDING SCHEDULE, TYPE OF FORMULA, ROUTE, RATE… IF NOT RECEIVING FEEDS WHAT OTHER NUTRITION IS THE PATIENT RECEIVING?
7 NUR3805_Pt2_Spring 2017 INTAKE & OUTPUT
24 Hour Fluid Requirement: SHOW YOUR MATH : What is the hourly fluid requirement?
100cc FIRST 10kg 50cc NEXT 10kg 20cc REMAINDER OF WT kg
□ N/A if >70kg
What was your patient’s total shift intake? Was the intake adequate? □ YES □ NO ______cc Rationale: If inadequate
Type of IV Fluid: Why is the patient receiving IV fluids?
______@ ______hour □No IV □Saline Lock
24 Hour Output Requirement & Shift Total Was the output adequate? (1cc/kg/hour) □ YES □ NO
□ N/A if > 30cc/hour Rationale: If inadequate
8 NUR3805_Pt2_Spring 2017 VITAL SIGNS
VITAL SIGNS MORNING AFTE INTERPRET NURSING RNOO INTERVENTIONS N Temperature NORMAL HIGH LOW Pulse NORMAL HIGH LOW Respiration NORMAL HIGH LOW Blood Pressure NORMAL HIGH LOW Oxygen Saturation NORMAL HIGH LOW
PAIN
CIRCLE Pain Scale Utilized: 0-10 FLACC FACES COMFORT OTHER: ______
Pain Score: ______
Interventions (What would be used if no pain?)______
Effectiveness: ______□N/A
9 NUR3805_Pt2_Spring 2017 FAMILY
Who cares for the child? And who is at the bedside?
______
Siblings: ______
Do you observe any abnormal family interaction? □YES □NO
EXPLAIN: ______
INTERVENTIONS NECESSARY: ______
TEACHING
What did you teach the child or family today? What teaching could be done if not?
10 NUR3805_Pt2_Spring 2017 PLAY THERAPY
What type of play did you initiate or observe? What toys were used?
Complete a head to toe assessment and write this up as follows:
-Skin
-Eyes
-Mouth
-Heart
-Abdomen
-Genitals
-Extremities
-Head
-Face
-Ears
-Nose
-Lungs
-Spine
11 NUR3805_Pt2_Spring 2017 LAB & DIAGNOSTIC TESTING
IDENTIFY THE WHY WAS IT IDENTIFY NURSING LAB OR ORDERED? ABNORMAL INTERVENTIONS DIAGNOSTIC RESULTS & CAUSE TEST
12 NUR3805_Pt2_Spring 2017 EXPLAIN WHY THE FOLLOWING LABS ARE DONE FOR PATIENTS IN AN ICU SETTING. INCLUDE HOW THEY ARE DRAWN AND A SHORT DEFINITION. RSV, FLU, MRSA, PCR, ELECTROLYTES, ABG, VBG, CBG, BLOOD CULTURES, BRONCHIAL ALVEOLAR LAVAGE AND CBC.
13 NUR3805_Pt2_Spring 2017 MEDICATIONS
BRAND & DOSAGE WHY IS RECOMMENDED WEIGHT BASED SAFE MAJOR GENERIC + ROUTE DRUG DOSAGE (MG/KG) Y OR N SIDE NAME & PRESCRIBED DOSAGE EFFECTS DRUG CALCULATION DOSE (SHOW YOUR MATH) BRAND
GENERIC
CLASS
BRAND
GENERIC
CLASS
BRAND
GENERIC
CLASS
14 NUR3805_Pt2_Spring 2017 CRITICAL THINKING
1. During your first interaction with the child/family, what did you notice (odors/smell,
general appearance, location and position of child, family & visitor interaction,
equipment in room)? What were your initial thoughts about the child and family? What
emotions did you feel? What came to mind?
2. What things are connected to or inserted in your patient? Make a list of all dressings,
tubes, lines, monitors, and equipment that are being utilized for patient care. For each
item, list separately and explain: (If in ICU setting, address central lines, chest tubes
and feeding tubes only)
a. Purpose of item?
b. How you know the item is accomplishing its intended result?
c. What about the item or patient should be reported to the instructor and staff, why, & how soon?
3. What interventions did you implement for your patient/family? Include a rationale for
each intervention.
4. Were your interventions effective? Explain. What other interventions could have been
implemented?
5. In your opinion, what did you do well today? What do you need to improve upon?
How could your clinical day be improved?
15 NUR3805_Pt2_Spring 2017 ARKANSAS TECH UNIVERSITY Department of Nursing NUR 3805 – Practicum in Nursing II Obstetrical Clinical Worksheet
1. You will be assigned to all three areas usually on different clinical days (L &D, Nursery, & postpartum) during your rotation.
2. Please complete all prep work Newborn assessment and prepwork, Postpartum/ L &D/PP patient, EFM worksheet) for all three areas before your rotation starts. Bring ALL of your prep work with you to EVERY clinical day. (You may need to check the filing cabinet in the nursing office to locate your folder that has been graded the day before clinicals).
3. You will complete two full patient assessments (one in nursery and one in either PP or L &D) with one nursing care plan during your rotation (NO PAIN or INFECTION).
4. You will also need to complete the asterisked sections of your clinical paperwork before your clinical day (assessment of the newborn & EFM worksheet). Please also bring your gestational age assessment sheet provided in class to clinical.
5. Be prepared to answer questions related to your prep work as well as your suggested medication list.
6. You will have 2 quizzes and 2 articles due during this rotation.
7. Please turn in your completed post clinical paperwork in a folder with your name and KEEP each previous week’s work in the folder along with your new work.
16 NUR3805_Pt2_Spring 2017 POSTPARTUM ASSESSMENT
Student Name:______
IDENTIFYING DATA Date:______Pt initials: ______Age: ______Race: ______Allergies:______Occupation: ______Medical Diagnosis:______Delivery Type:______Gravida: ______Para: ______Abortions: ______Term: ______Preterm: ______Living: ______Complications (maternal/fetal): ______Prepregnancy wt: ______Pregnancy wt: ______Height: ______
ASSESSMENT General Appearance: ______Skin/Hair: ______Respirations: Rate______Breath Sounds and effort: ______Smoker: Y/N Pk/day: ______No. of years ______Hx of Drug Use: Y/N Current Drug Use: Y/N Positive drug screen for:______Temperature ______B/P: ______Pulse: ______Regular/Irregular Heart Sounds: ______Peripheral Pulses (1-4+): Radial:______Dorsalis pedis: ______Edema(grade/location):______Skin turgor: ______Mucous membranes: ______Nausea/Vomiting: ______Prescribed diet: ______Food restrictions: ______Current IV solution and rate: ______24 hour I and O (if ordered/has IV/ or PIH): Input______Output______Meal %: ______Last bowel movement: ______
17 NUR3805_Pt2_Spring 2017 Bowel sounds: ______Hemorrhoids: Y/N Difficulty voiding: Y/N Bladder palpable: Y/N Foley catheter: Y/N Estimated Blood Loss: ______PAIN/COMFORT Location: ______Quality: ______Duration: ______Precipitating factors: ______Guarding: ______Facial Grimace: ______Pain Scale: No Pain 0 1 2 3 4 5 6 7 8 9 10 Worst Pain Imaginable
NEUROSENSORY Hearing Aid: ______Glasses: ______Contacts: ______Headaches: Location: ______Frequency: ______Seizures: ______Reflexes: ______Epigastric pain:______
Lab: Hgb&Hct: Pre Delivery______Post Delivery: ______WBC______Platelets______Blood Type: ______If mother Blood type O or Rh-: Baby’s Blood Type ______Coombs: ______HIV: ______Hep. B: ______Group B Strep: ______Rubella Titer: ______VDRL/Syphillis: ______Urinalysis if ordered:______
Feeding: Breast or Bottle Feeding If breastfeeding, complete the following – poor, fair, well Bra: ______Nipples (shape, condition): ______Latching on: ______Any referral to Lactation specialist______UTERUS Fundus: Consistency:______Height:______Position:______Lochia: Color:______Amount:______Clots:______Episiotomy/Lacerations: Type______Swelling______Redness/or drainage: ______
18 NUR3805_Pt2_Spring 2017 Surgical incision: Appearance:______Type: ______Dressing: ______MENSTRUAL HISTORY Frequency: ______Duration: ______Amount: ______LMP: ______Pap smear: ______Contraceptive Plan: ______
Pregnancy planned (Y/N) Marital Status: ______Living With: ______Financial Concerns: ______Extended family/other support: ______Religion: ______Cultural Factors: ______Report stress factors: ______Verbal/nonverbal communication with family/significant other: ______Hx of Postpartum Depression: Y/N Patient Demeanor:______Bonding behavior (including father): ______MEDICATIONS (List all routine and prn meds given) Drug name/mg How prescribed Purpose ______TEACHING/LEARNING Educational background (mother/father): ______Previous childbirth experience: ______In Hospital/Discharge Teaching: ______
19 NUR3805_Pt2_Spring 2017 Obstetrical Simulation
Simulation 1 1. Watch Postpartum Assessment YouTube videos and Gestation Assessment Videos on Blackboard under NUR 3805 2. Review Postpartum BUBBLE He sheet provided in class 3. Describe the proper nursing assessment techniques utilized during the first 24 hours using BUBBLE HE for vaginal and cesarean section.
4. Define Fundus and discuss techniques and deviations to assess. a. Discuss Involution and expected progression. b. Define Lochia and discuss stages?
Simulation 2 b.i.1. Complete asterisk* areas on Fetal Heart Monitor Strip Worksheet if you have not done so
already for clinical.
b.i.2. Discuss Spinal versus Epidural for a C-section. Discuss nursing interventions for a patient
undergoing a cesarean section.
b.i.3. Discuss pre and post-op teaching related to the patient undergoing a cesarean section.
b.i.4. Discuss the nursing care related to the patient undergoing elective induction.
Simulation 3
1. Discuss nursing interventions related to Pregnancy Induced Hypertension.
2. Discuss nursing assessments and interventions for Post-Partum hemorrhage
3. Complete a care plan with your clinical group for Pregnancy Induced Hypertension and Post-Partum
hemorrhage
20 NUR3805_Pt2_Spring 2017 21 NUR3805_Pt2_Spring 2017 b.i.5. b.i.6. b.i.7. b.i.8. NURSING CARE PLAN b.i.9. i.b. .b b.i.10. 1.1 .i 31 b.i . . b b. 12 i. . 1 . i 5. N . b. 1 i. 4 1 . 6. P I
b.i.21. i.b. 2.2
b i. 2. i.b. .3 4.2
22 NUR3805_Pt2_Spring 2017 b.i.27. The student is expected to maintain a drug card, or mark in drug book, on each of the medications ordered for their assigned client. It is the responsibility of the student to know and understand the drugs. The following lists are some of the common drugs used. b.i.28. DRUGS b.i.29 b.i. b.i.31 . N 30. . P b.i.32u b.i.Po b.i.34o . A 33. . * b.i.35 b.i. b.i.40 . * 39. . M b.i.41A b.i.* b.i.43o . C 42. . N b.i.44 b.i. b.i.46 . * 45. . * b.i.47 b.i. b.i.49 . G 48. . P b.i.50 b.i. b.i.52 . * 51. . * b.i.55 b.i.53 b.i. . * . N 54. P b.i.5 b.i. b.i.58 6. * b.i.5 57.b.i. . 9. 60. b.i.62 * b.i.6 b.i. b.i.65. 3. 64. . S b.i.6 b.i. b.i.68 6. 67. . * b.i.6 b.i. b.i.71 9. 70. . V b.i.7 b.i. b.i.74 2. 73. . V b.i.7 b.i. b.i.77 5. 76. . X b.i.7 b.i. b.i.80 8. 79. b.i.8 b.i. . Z b.i.83 1. 82. b.i. . * b.i.8 85. b.i.86 4. Pro . C b.i.8 b.i. b.i.89 7. 88. D b.i.9 b.i. .b.i.92 0. b.i.9 91. . * 3. b.i. b.i.95 94. b.i.9 . N 6. b.i. b.i.9 b.i.99. 97. 8. b.i.101.b.i.100. b.i.102. The above medications with an asterisk (*) should be reviewed in detail. Expect to administer and verbalize drug information to instructor. You will be giving these medications more frequently. b.i.103. b.i.104. b.i.105. 23 NUR3805_Pt2_Spring 2017 b.i.106. b.i.107.
b.i.108. 1. Discuss the risk for heat loss in the newborn and what nursing interventions are used to prevent them.
b.i.109. 2. Discuss the pathophysiology in regards to newborn jaundice. Also discuss the b.i.110. different types/causes of jaundice and treatment.
b.i.111. 3. Discuss elimination patterns of the newborn (voiding and stooling). Also discuss the difference in stooling between breast vs. bottle feeding.
b.i.112. 4. Complete the clinical significance for the assessment of the newborn including b.i.113. normals and abnormals. (PRIOR TO CLINICAL)
b.i.114. 5. Describe the process of assigning APGARS at birth including the five criteria of b.i.115. assessment.
24 NUR3805_Pt2_Spring 2017 b.i.116. 6. Summarize the indication and use of Vitamin K, Hepatitis B, and Erythromycin. b.i.117. (Including site of administration and proper equipment)
b.i.118. 7. Identify teaching and learning needs of the new mother and family of a newborn.
8. Discuss hypoglycemia criteria and treatment in the newborn.
Discuss feeding methods and timing in the newborn. (breast, bottle, gavage)
Discuss common skin conditions found in the newborn. b.i.119. PREP FORM FOR NEWBORN NURSERY b.i.120. b.i.121. Be prepared to answer questions, verbally or by quiz, during the clinical day. b.i.122. b.i.123. b.i.124. b.i.125. b.i.126. b.i.127. b.i.128. b.i.129.
25 NUR3805_Pt2_Spring 2017 b.i.130. b.i.131. PREPARATION FOR LABOR/POSTPARTUM PATIENT b.i.132. b.i.133. b.i.134. The information should be written on additional pages. b.i.135. b.i.136. 1. Discuss a postpartum assessment for a vaginal and a cesarean section patient (including fundus, lochia, bladder…) b.i.137. b.i.138. 2. Complete asterisk* areas on Fetal Heart Monitor Strip Worksheet. Be ready to discuss early, variable, and later decelerations in clinical. b.i.139. b.i.140. 3. List normals in the following statistics: b.i.141. Blood pressure: Temp: b.i.142. Pulse: b.i.143. Fetal heart rate: b.i.144. Respirations: b.i.145. b.i.146. 4. Be able to define terms: Presentation, position, dilation, station, effacement, contraction, duration, frequency , intensity and variability. b.i.147. b.i.148. 5. Discuss the different types of anesthesia (spinal, epidural, general) and analgesia (IV narcotics) during labor and possible effects to mother and/or baby. b.i.149. b.i.150. 6. Discuss breast care for the lactating and non-lactating mother. b.i.151. b.i.152. 7. Discuss pitocin for induction vs. use during the recovery period. Discuss Magnesium Sulfate for the pre-eclamptic pt vs. the preterm patient. Discuss assessment and risk factors for both pitocin (oxytocin) and magnesium sulfate. Identify the antidote for magnesium sulfate toxicity b.i.154.b.i.153. b.i.155. 8. Discuss the risks for pre-term labor, the current means for identifying patients at risk, and the identification and protocols for group B strep. b.i.156.
9. Discuss the use of MMR and TDAP vaccines in the Prenatal or Postpartum period. b.i.157. Also discuss the indications, dosing, and administration of Rhogam. b.i.158. (Discuss appropriate sites and needle size and length.)
26 NUR3805_Pt2_Spring 2017 10. Discuss the care of the episiotomy site, including comfort measures.
b.i.159.Be prepared to answer questions, verbally or by quiz, during the clinical day. b.i.160. b.i.162. b.i.163. Date b.i.161. Patient
a.i.1. WORKS HEET a.i.2. FETAL HEART MONITOR STRIP
Initials: b.i.164. b.i.165. 1. Fetal Heart Rate - Beats per minute? b.i.166. Check one of the following: Indicate criteria for all. b.i.167. _____Tachycardia *Criteria: b.i.168. b.i.169. _____Average *Criteria: b.i.170. b.i.171. _____Bradycardia *Criteria: b.i.172. b.i.173. b.i.174. 2. What is the baseline variability? What is the significance of reading? * b.i.175. b.i.176. _____Absent variability: 0 to 2 bpm. b.i.177. b.i.178. _____Minimal variability: 3 to 5 bpm. b.i.179. b.i.180. _____Average/Moderate: 6 to 25 bpm. b.i.181. b.i.182. _____Marked: greater than 25 bpm. b.i.183. b.i.184. 3. Are there any periodic changes in the FHR? b.i.185. _____Accelerations b.i.186. b.i.187. _____Early deceleration Usual cause : * b.i.188. b.i.189. _____Late deceleration Usual cause: * b.i.190. b.i.191. _____Variable Deceleration Usual cause: * b.i.192. b.i.193. 4.Looking at uterine contractions, determine the
27 NUR3805_Pt2_Spring 2017 following: b.i.194. USE ADDITIONAL PAGES b.i.195. ______Frequency: Define term: * b.i.196. ______Duration: Define: * b.i.197. b.i.198. 5.* Nursing interventions utilized for all 3 types of decelerations. b.i.199. USE ADDITIONALb.i.205. PAGES b.i.206. 6.Summarize the significance of your patient’s strip. b.i.207. USE ADDITIONAL PAGES b.i.208. b.i.229. * Please complete the above noted areas prior to clinicals b.i.230. Patient's INITIALS: b.i.231. b.i.232. DA TE: a.i.3. ASSES SMENT OF THE NEWBORN b.i.233. b.i.234.IDENTIFICATION PLACEMENT: b.i.235. b.i.237. b.i.239. b.i.240. APGAR: b.i.236. b.i.238. ED (1 m) (5 DELIVE C: m)
b.i.241. b.i.243. b.i.242. METHOD OF b.i.244. Est. DELIVERY: Gest. Age: b.i.245. b.i.246. FINDING CLINICAL SIGNIFICANCE * b.i.247. b.i.250. b.i.252. b.i.253. b.i.248. b.i.251. Weight b.i.249.
b.i.254. b.i.257. b.i.259. b.i.260. b.i.255. b.i.258. Length b.i.256.
b.i.261. b.i.264. b.i.266. b.i.267. b.i.262. b.i.265. Posture
28 NUR3805_Pt2_Spring 2017 b.i.263.
b.i.268. b.i.271. b.i.273. b.i.274. b.i.269. b.i.272. Head
b.i.270.
b.i.275. b.i.278. b.i.280. b.i.281. b.i.276. b.i.279. Chest
b.i.277.
b.i.282. b.i.285. b.i.287. b.i.288. b.i.283. b.i.286. Tempera
b.i.284.
b.i.289. b.i.292. b.i.294. b.i.295. b.i.290. b.i.293. Resp:Rat
b.i.291.
b.i.296. b.i.298. b.i.299.
b.i.297. Heart
b.i.300. b.i.302. b.i.304. b.i.305. b.i.301. b.i.303. Sucking,
b.i.306. * Discuss normals and abnormals. Have this column prepared
29 NUR3805_Pt2_Spring 2017 prior to nursery day. b.i.307. b.i.308. b.i.309. b.i.310. b.i.311. b.i.312. b.i.314. b.i.316. b.i.317. C b.i.313. IT b.i.315. LINICAL EM FINDING SIGNIFIC ANCE * b.i.318. b.i.320. b.i.321. Eyes/Ea
b.i.319. b.i.322. b.i.324. b.i.326. b.i.323. b.i.327. Moro b.i.325.
b.i.328. b.i.332. b.i.334. b.i.335. b.i.329. b.i.333. Skin: b.i.330. C olor b.i.331. b.i.336. b.i.340. b.i.342. b.i.343. b.i.337. Bi b.i.341. rthmarks b.i.338. b.i.339. b.i.344. b.i.348. b.i.350. b.i.351. b.i.345. L b.i.349. anugo b.i.346. b.i.347. b.i.352. b.i.357. b.i.359. b.i.360. b.i.353. b.i.358. Head b.i.354. F ortanelles b.i.355. Si ze/Shape b.i.356. b.i.361. b.i.363. b.i.365. b.i.366. b.i.362. b.i.364. 30 NUR3805_Pt2_Spring 2017 Pulses
b.i.367. b.i.369. b.i.371. b.i.372. b.i.368. b.i.370. Umbilic
b.i.373. b.i.375. b.i.377. b.i.378. b.i.374. b.i.376. b.i.379. Genitals b.i.380. b.i.387. b.i.389. Plantar b.i.390. b.i.388. b.i.391.
b.i.381. Reflexes
b.i.382. G rasp b.i.383. Pl antar b.i.384. B abinski b.i.385. b.i.386.
31 NUR3805_Pt2_Spring 2017 b.i.393. b.i.394. b.i.395. b.i.396. 1. Review Chapter 18, 19, 20 in Brunner & Suddarth b.i.397. b.i.398. b.i.399. b.i.400. b.i.401. b.i.402.2. Prepare drug cards or list for:
a.i.4. SAME DAY SURGERY PREP SHEET
b.i.403. a.Alka Setzer Gold d. Valium g. Atropine b.i.404. b.Zantac e. Zofran h. Chloral Hydrate b.i.405. c.Versed Syrup f. Reglan i. Phenergan b.i.406. j. Lovenox b.i.407. b.i.408. Include action, major side effects, and reason given to surgical patients. b.i.409. List references used b.i.410. b.i.411.3. Prepare a pre and postoperative teaching plan for a child undergoing a tonsillectomy. All interventions must have a referenced rationale. Information can be found in Brunner & Suddarth, London & Ladewig and on- line. b.i.412. You must use APA format for listing sources and references. b.i.413. b.i.414. b.i.415.4. Calculate the preoperative medication for a child weighing 22 lbs. b.i.416. b.i.417. PAM 0.5 ml per kilogram b.i.418. available premixed in 10 ml syringe b.i.419. b.i.420. Atropine 0.01 mg per kilogram b.i.421. available in 0.4 mg/ml vial b.i.422. b.i.423. b.i.424. b.i.425. b.i.426. 5. Include discharge teaching for four patients, the discharge teaching must have have rationales that are referenced. Briefly discuss procedure and patient history b.i.427. rationales that are referenced. Briefly discuss procedure and patient history and b.i.428. instructions for self care at home. b.i.429. b.i.430. 6. Include a log for each day of clinical. b.i.431. Diagnostic Recovery Paperwork
1. Prior to your first day in Diagnostic Recovery (DR), prepare a written drug list for: a. Versed (midazolam) g. Decadron / Hexadrol (dexamethasone) b. Fentanyl (sublimaze) h. Benadryl (diphenhydramine) c. Demerol (meperidine) i. Narcan (naloxone) d. Robinul (glycopyrrolate) j. Romazicon (flumazenil) e. Valium (diazepam) k. Aspirin (acetylsalicylic acid) f. Plavix (clopidogrel) b.i.432.
2. Review how to place a peripheral IV and a foley catheter. You will start several IVs and may be required to place a foley in DR. Be prepared to answer questions prior to being allowed to perform these procedures. b.i.433.
3. Look up the Aldrete (or modified Aldrete) score. Be familiar with its purpose. b.i.434.
4. Start working on the following teaching plans prior to first clinical day in DR. You will fine tune these during DR clinical time. Turn completed plans in on Monday (by 0830) after last clinical day in DR: a. Prepare a pre- and post-procedure teaching plan for a patient undergoing a colonoscopy. b. Prepare a pre- and post-procedure plan for a patient undergoing a cardiac catheterization for shortness of breath, chest pain, and abnormal ECG. b.i.435.
5. Review and be able to discuss administration of packed red blood cells (PRBC) during clinicals. Include the following in your written paperwork to be turned in after clinical rotation: a. Explain what labs should be drawn prior to administration of PRBCs. b. Most patients who are going to receive blood products are also given diphenhydramine and/or dexamethasone IV prior to administration. Please give a brief explanation as to why these drugs are given. c. Describe signs and symptoms of a transfusion reaction and what you as a nurse would need to do if this were to happen to your patient. What is the absolute most important thing to do if a reaction is suspected? b.i.436.
6. Cardiac cath patients have the following labs drawn prior to their procedure: CBC, BMP (basic metabolic panel), lipids, PT/PTT with INR. Give a brief explanation of what you think they are looking for in these labs and why they are important. Also, why is it important to do an ECG prior to a cardiac cath? Include this information with the teaching plans and transfusion information listed above. b.i.437.
7. During clinicals, explore how to write an RN note for recovery following a GI procedure (these are done on paper, not on the computer, at St. Mary’s).
b.i.438. b.i.439. *Prep work must be completed and turned in the morning of your first day in DR! Failure to bring completed prep work may result in you being sent home from clinicals. b.i.440. 8. b.i.441. ARKANSAS T ECH UNIVERSITY b.i.442. Department of Nursing b.i.443. Evidence Based Family Paper Agreement b.i.444. b.i.445. b.i.446. NOTE: Agreement due to Assigned Faculty member on or before assigned date. b.i.447. b.i.448. You May Not Use a Family Member or Another Nursing Student’s Family. b.i.449. b.i.450. Name of Student______Assigned Faculty Member______b.i.451. b.i.452. Name of Male Head of Household______b.i.453. b.i.454. Name of Female Head of Household______b.i.455. b.i.456. Street Address______Apt. No.______b.i.457. b.i.458. City, State, Zip Code______b.i.459. b.i.460. Telephone Numbers______Best Time to Call______b.i.461. b.i.462. In the table below, list the names of all persons living in this household, their ages, and relationship to the b.i.463. Head(s) of the household. If additional space is needed, use the back of this form. b.i.464. b.i.468. b.i.465. Name b.i.467. b.i.469. Relat of Each ionship to Individual Living Head(s) of in Household Household b.i.470. b.i.474. b.i.471. b.i.473. b.i.475. b.i.476. b.i.480. b.i.477. b.i.479. b.i.481. b.i.482. b.i.486. b.i.483. b.i.485. b.i.487. b.i.488. b.i.490. b.i.492. b.i.489. b.i.491. b.i.493. b.i.494. b.i.496. b.i.498. b.i.495. b.i.497. b.i.499. b.i.500. b.i.502. b.i.504. b.i.501. b.i.503. b.i.505. b.i.506. b.i.508. b.i.510. b.i.507. b.i.509. b.i.511. b.i.512. Head(s) of Household, please read the following statement and sign below: b.i.513. I/We agree to allow the Arkansas Tech University Nursing Student named above to visit us in our home for the purpose of meeting his/her b.i.514. educational objectives in the Nursing Program at Arkansas Tech University. We understand that the student will be interviewing us and may b.i.515. carry out teaching programs and/or other nursing actions provided that we give consent. We understand that the information we provide the b.i.516. student will be kept confidential and will be handled in a professional manner. We understand that we may refuse any teaching or other b.i.517. nursing care at any time. We understand that the student will be visiting us in our home from four to six times over the period of the next b.i.518. several weeks. We understand that this agreement will be terminated the last scheduled visit, or when requested, whichever comes first. b.i.519. b.i.520. I/We agree to the above statement______Date______b.i.521. ______Date______b.i.522. I agree to the above statement______(Student)Date______b.i.523. b.i.524. ARKANSAS TECH UNIVERSITY b.i.525. NUR 3805 Practicum in Nursing II b.i.526. Evidence Based Family Paper b.i.527. b.i.528. Objective: 1. Utilize the nursing process to plan and deliver care to individuals and families. 2. Practice the role of caregiver, communicator, collaborator and teacher in the delivery of holistic care to a family unit. 3. Utilize current evidence based literature to assist families in making positive lifestyle changes. b.i.529. b.i.530. Selecting a Family: b.i.531. Seek help from family, friends, church and/or community members to locate a suitable b.i.532. family. The selected family needs to include either children and/or a pregnant family b.i.533. member. Family members, friends, or classmates families may not be used. b.i.534. Number of Visits: b.i.535. The student will visit the family from 4 to 6 times in person. b.i.536. Written Requirements: b.i.537. The student will submit a written comprehensive professional paper of between 5 and 8 b.i.538. pages (not including title and reference pages). Current APA guidelines must be b.i.539. followed. b.i.540. Process: b.i.541. After selecting a family to use for the paper, the student should: Contact the family to schedule the initial visit and obtain a signed “Family Paper Agreement Contract.” The “Family Visit Log” should be initiated on the first visit and updated after each visit throughout the project. Initiate the “Family Assessment” to determine the needs of the family. Complete the assessment and submit the assessment guide by the due date. Your assessment will determine your planning and intervention for each subsequent visit. Identify THREE priority needs for the family from your completed family assessment. These are not nursing diagnoses. Utilize journal articles and reputable internet sources (government guidelines, etc.) to gather evidence-based educational materials to address the family’s priority needs. You will utilize these materials during each planned family visit. Teaching must be based on evidence (evidence based practice). You may use your textbook only for introductory support. Evaluate the effectiveness of the intervention for each priority need (three required). Terminate the relationship on the last visit and ensure that the family has appropriate referrals in place. Complete your family paper by submitting an electronic copy online within the Blackboard practicum course, a paper copy to your instructor along with a grade sheet and copy of teaching materials provided to family. b.i.542. b.i.543. b.i.544. Arkansas Tech University b.i.545. Department of Nursing b.i.546. Evidence Based Family Paper - Level II b.i.547. b.i.548. Student: ______Grade: ______b.i.549. Instructor: ______
b.i.550. b.i.552. b.i.551. Evaluation: (Total Possible Points - 100%) b.i.553. POINT
b.i.554. b.i.559. b.i.555. Introduction and Conclusion (5%) b.i.556. Describe family type, purpose and organization of b.i.560. paper. b.i.557. No abstract is necessary. b.i.558. b.i.561. b.i.566. b.i.562. Family Visit Log (10%) b.i.563. Detailed description of each visit & plan for future b.i.567. ___ visits (see form) points b.i.564. b.i.565. b.i.568. b.i.573. b.i.569. Family Assessment Guide (20%) b.i.570. Completed assessment form. Student will make b.i.574. revisions based on instructor comments. b.i.571. b.i.572. b.i.575. Family summary and identification of three b.i.578. priority needs (15%) b.i.576. Summarize family assessment and identify three b.i.579. priority needs with supportive evidence. b.i.577.
b.i.580. Intervention using evidence-based practice and b.i.584. education (30%) b.i.581. Identify interventions for each need utilizing b.i.585. evidence based-practice and education reference materials appropriately in the document and provide a copy of all teaching materials - Must use reputable sources. b.i.582. b.i.583. b.i.588. b.i.586. Evaluation and Adaptations (20%) b.i.589. b.i.587. What worked, what didn’t, any adaptations made, and why.
b.i.592. b.i.590. APA Format, Grammar and Spelling b.i.593. b.i.591. As many as 5 points can be deducted
b.i.594. b.i.596. b.i.595. Total b.i.597. b.i.598. FAMILY VISIT LOG (Make copies- will be longer than one page) b.i.599. b.i.601. b.i.604. b.i.602. Detailed summary of visit: b.i.605. Detailed plan and date b.i.603. What was the purpose of this visit? Did you use any teaching for materials? What did/didn’t you accomplish (evaluation)? Any adaptation b.i.606. future visit(s) necessary? b.i.607. b.i.608. b.i.609.
b.i.610.