Case Example for CORFs, HHAs, Hospices and SNFs Appeal Procedures
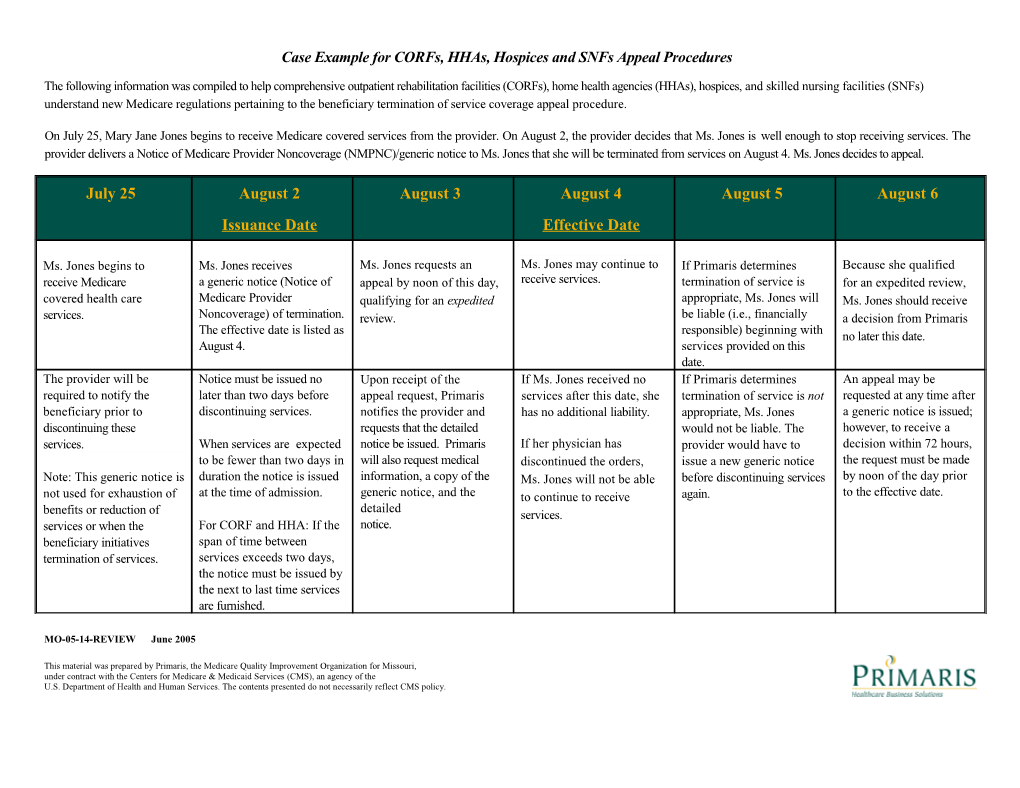
The following information was compiled to help comprehensive outpatient rehabilitation facilities (CORFs), home health agencies (HHAs), hospices, and skilled nursing facilities (SNFs) understand new Medicare regulations pertaining to the beneficiary termination of service coverage appeal procedure.
On July 25, Mary Jane Jones begins to receive Medicare covered services from the provider. On August 2, the provider decides that Ms. Jones is well enough to stop receiving services. The provider delivers a Notice of Medicare Provider Noncoverage (NMPNC)/generic notice to Ms. Jones that she will be terminated from services on August 4. Ms. Jones decides to appeal.
July 25 August 2 August 3 August 4 August 5 August 6 Issuance Date Effective Date
Ms. Jones begins to Ms. Jones receives Ms. Jones requests an Ms. Jones may continue to If Primaris determines Because she qualified receive Medicare a generic notice (Notice of appeal by noon of this day, receive services. termination of service is for an expedited review, covered health care Medicare Provider qualifying for an expedited appropriate, Ms. Jones will Ms. Jones should receive services. Noncoverage) of termination. review. be liable (i.e., financially a decision from Primaris The effective date is listed as responsible) beginning with no later this date. August 4. services provided on this date. The provider will be Notice must be issued no Upon receipt of the If Ms. Jones received no If Primaris determines An appeal may be required to notify the later than two days before appeal request, Primaris services after this date, she termination of service is not requested at any time after beneficiary prior to discontinuing services. notifies the provider and has no additional liability. appropriate, Ms. Jones a generic notice is issued; discontinuing these requests that the detailed would not be liable. The however, to receive a services. When services are expected notice be issued. Primaris If her physician has provider would have to decision within 72 hours, to be fewer than two days in will also request medical discontinued the orders, issue a new generic notice the request must be made Note: This generic notice is duration the notice is issued information, a copy of the Ms. Jones will not be able before discontinuing services by noon of the day prior not used for exhaustion of at the time of admission. generic notice, and the to continue to receive again. to the effective date. detailed benefits or reduction of services. services or when the For CORF and HHA: If the notice. beneficiary initiatives span of time between termination of services. services exceeds two days, the notice must be issued by the next to last time services are furnished.
MO-05-14-REVIEW June 2005
This material was prepared by Primaris, the Medicare Quality Improvement Organization for Missouri, under contract with the Centers for Medicare & Medicaid Services (CMS), an agency of the U.S. Department of Health and Human Services. The contents presented do not necessarily reflect CMS policy.