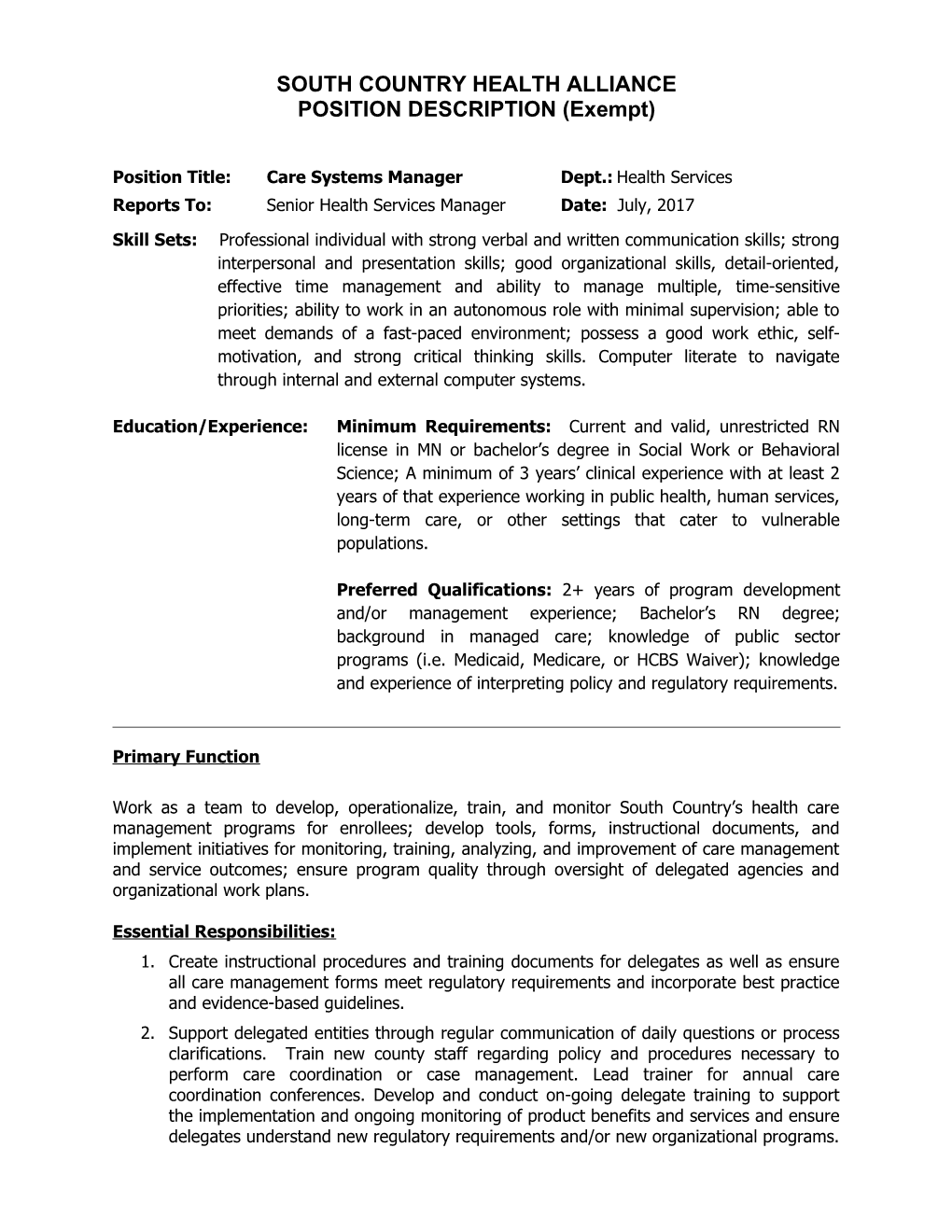
SOUTH COUNTRY HEALTH ALLIANCE POSITION DESCRIPTION (Exempt)
Position Title: Care Systems Manager Dept.: Health Services Reports To: Senior Health Services Manager Date: July, 2017
Skill Sets: Professional individual with strong verbal and written communication skills; strong interpersonal and presentation skills; good organizational skills, detail-oriented, effective time management and ability to manage multiple, time-sensitive priorities; ability to work in an autonomous role with minimal supervision; able to meet demands of a fast-paced environment; possess a good work ethic, self- motivation, and strong critical thinking skills. Computer literate to navigate through internal and external computer systems.
Education/Experience: Minimum Requirements: Current and valid, unrestricted RN license in MN or bachelor’s degree in Social Work or Behavioral Science; A minimum of 3 years’ clinical experience with at least 2 years of that experience working in public health, human services, long-term care, or other settings that cater to vulnerable populations.
Preferred Qualifications: 2+ years of program development and/or management experience; Bachelor’s RN degree; background in managed care; knowledge of public sector programs (i.e. Medicaid, Medicare, or HCBS Waiver); knowledge and experience of interpreting policy and regulatory requirements.
Primary Function
Work as a team to develop, operationalize, train, and monitor South Country’s health care management programs for enrollees; develop tools, forms, instructional documents, and implement initiatives for monitoring, training, analyzing, and improvement of care management and service outcomes; ensure program quality through oversight of delegated agencies and organizational work plans.
Essential Responsibilities: 1. Create instructional procedures and training documents for delegates as well as ensure all care management forms meet regulatory requirements and incorporate best practice and evidence-based guidelines. 2. Support delegated entities through regular communication of daily questions or process clarifications. Train new county staff regarding policy and procedures necessary to perform care coordination or case management. Lead trainer for annual care coordination conferences. Develop and conduct on-going delegate training to support the implementation and ongoing monitoring of product benefits and services and ensure delegates understand new regulatory requirements and/or new organizational programs. Be a resource to care management staff regarding care coordination policies, procedures and duties in accordance with Centers for Medicare and Medicaid Services (CMS) and MN Department of Human Services (DHS) contract guidelines.
3. Collaborate and share information with delegate interdisciplinary care teams in order to identify and assist enrollees with benefit or utilization issues through data analysis, care planning, focus reviews, case consultation, and care coordination. Facilitate teamwork to meet medical and care coordination needs of enrollees. Conduct monthly meetings directly with delegates and quarterly meetings with delegate liaison staff. 4. Execute or contribute to reports and monitor quality with State and Federal quality improvement or assurance requirements such as Part C Data Validation, Model of Care, care transitions, and care planning. Evaluate, audit, and/or make recommendations to improve quality oversight of delegated services. 5. Provide leadership for the interpretation of results and development of improvement action plans arising from quality and regulatory initiatives. Participate and represent agency at meetings with regulators. 6. Provide quality oversight of agency processes such as Personal Care Assistant or Elderly Waiver Authorizations, Denial, Termination, or Reduction requests, and Residential Services Workbook review. Take action on reports involving Elderly Waiver, Enrollment, or Pre-Admission Screening notifications. 7. Assist with the development of policies, procedures, and programs to meet the goals of our enrollees in a cost effective and quality delivery system. Partner with functional areas such as Operations, Member Services, Information Technology, Communications, and Quality to review performance and effectiveness and determine actionable items to address enrollee issues. Participate in oversight and quality performance of in-reach programs. Contribute data for pay-for-performance measures. 8. Oversee and coordinate cross-functional projects which impact product performance through identification, resolution and ongoing product performance monitoring. Track and communicate key product performance indicators including analyzing the results and advocating changes to meet departmental and company goals. 9. Effectively communicate information to superiors, team members, delegates, and other staff in a timely, accurate, respectful, and courteous manner. Develop and/or maintain professional relationships with stakeholders to facilitate information and program improvement. Collaborate with other health plans regarding process improvement. 10. Other duties as assigned within the scope, responsibility, and requirements of the job.
Additional Qualifications: To perform this job successfully, an individual must be able to perform each essential duty satisfactorily. The requirements listed below are representative of the knowledge, skill, and/or ability required.
Language Skills:
Must be able to read and write in English.
2 Mathematical Skills:
Analytic skills required.
Accuracy:
Considerable accuracy required. Errors would be difficult to detect and would have a critical impact on enrollees or South Country’s relationship with business partners.
Reasoning Ability:
Position requires use of considerable judgment and broad decision making, complex problem solving (technically and administratively). Must understand cause and effect relationships and be able to draw conclusions from data, regulatory requirements, and past practice.
Physical demands:
The physical demands described represent those that must be met by an employee to successfully perform the essential functions of this job. When possible, reasonable accommodations may be made to enable individuals with disabilities to perform the essential functions.
While performing the duties of this job, the employee is regularly required to talk or hear. The employee frequently is required to sit, stand and drive and; use hands to navigate office equipment (i.e. computer, telephone) and use office supplies; and reach with hands and arms.
The employee may occasionally lift and/or move up to 25 pounds. Specific vision abilities required by this job include close vision, distance vision, peripheral vision, depth perception, and the ability to adjust focus.
The duties of this job require the employee to be seated at a computer approximately 70% of the time. Communication by telephone is an integral part of this position.
Work Environment:
The work environment characteristics described here are representative of those an employee encounters while performing the essential functions of this job. Reasonable accommodations may be made to enable individuals with disabilities to perform the essential functions.
While performing the duties of this job, the employee should encounter no unusual or hazardous conditions. The noise level in the work environment is usually low.
The employee must be able to travel to counties and agencies within the service area and/or external meetings on average approximately one to two days per week.
Travel Requirements:
The employee must be willing and able to travel 1-2 times per week throughout Minnesota and the South Country service area.
Contacts:
3 Maintains satisfactory relationships; may include collaboration in executing established policies, discussion of ways to reach agreed-upon objectives, securing compliance with approved procedures; not proposing new or highly controversial programs.
In addition to Health Services, this position works most often with the following internal departments: Operations, Quality, and Member Services. This position also works with external business partners, including: Third Party Administrators (TPA’s), County Staff, MN Department of Human Services (DHS), Delegated Entities, and Providers.
Financial Impact:
Significant monetary responsibility; involves some risk.
This position is responsible for ensuring that South Country Health Alliance is following contract language as promulgated by governmental agencies. Failure to comply with this contractual language could result in breach of contract resulting in financial penalty, potential contract cancellation, sanctions and/or corrective action.
4