Client Name / Date of Birth / Medicaid #/ Member # Date of Service:
Initial Diagnostic Interview/Evaluation (90801) for DCFS Cases
Biopsychosocial Data
Client Information provided by:
1. Presenting Problems (or statement of behaviors resulting in referral)
2. Social History: (incl. demographics, residency, pertinent personal information including significant relationships and history of forming relationships)
3. Family Background: (incl. family history, living arrangements, caregivers)
4. Family Dynamics: (current and family of origin; including domestic violence)
5. Child Rearing Practices: (including impulse control; assertive and displays empathic responsiveness; understands and recognizes threats to child and assumes protective role)
6. Mental Health History: (discuss past & present assessment, and/or treatment services) *Specific assessment of trauma history including symptoms that may be related to the trauma, and an assessment of the environment to support recovery from the trauma – for children, assess the child’s care giving system and its capacity to support the child’s recovery from trauma)
7. Academic and Intellectual history and current functioning:
8. Medical History (describe past & present medical diagnoses, & treatment)
9. Use of Prescription medications for physical conditions: (past/present, dosage, frequency, mode, prescriber)
10. Legal and/or Court Involvement (past/present charges, arrests, convictions, probation, parole, Child in Need of Services Petitions, etc.)
11. Abuse and/or Neglect History: A. Offender Issues B. Survivor/Victim Issues
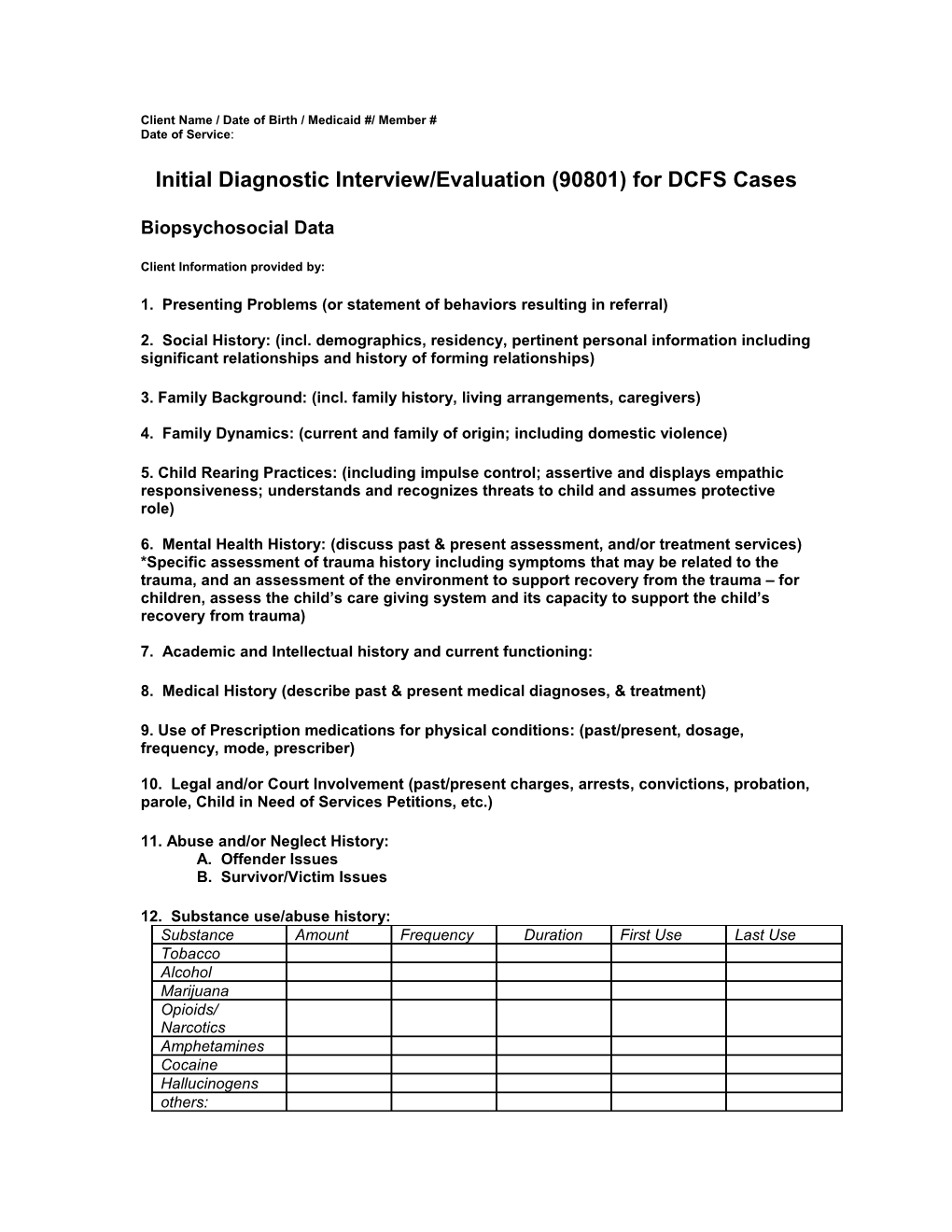
12. Substance use/abuse history: Substance Amount Frequency Duration First Use Last Use Tobacco Alcohol Marijuana Opioids/ Narcotics Amphetamines Cocaine Hallucinogens others: Client Name / Date of Birth / Medicaid #/ Member # Date of Service:
13. Strengths, Supports, and Needs Identification:
14. Mental Status Exam:
Appearance: Affect: Orientation: Mood: Thought Content: Thought Process: Speech: Motor: Intellect: Insight Judgment: Impulse Control: Memory: Concentration: Attention: Behavior: Thought Disorder:
15. Risk of Harm Assessment: (describe past & present occurrences) None Thoughts Plan Intent Means Attempt Able to Contract for Safety Noted Only (describe) (describe) (describe) (describe) Suicidal Ideation Homicidal Ideation
Risk Factors: ____ Non-compliance with treatment ______History of Domestic Violence ____ AMA/elopement potential ______Child Abuse &/or Neglect ____ Prior behavioral health inpatient admissions ______History of Sexual Abuse ____ Multiple behavioral health diagnoses ______Eating Disorder or self- mutilating ____ Suicidal/homicidal ideation/attempts ______Other behavioral factors (describe)
16. Impressions/Summary:
In Summary:
17. Diagnosis:
Axis I: Axis II: Axis III: Axis IV: Nature of Stressors: ___ Family ____ School ______Work ______Health ______other: ______Axis V: ______Mild ____ Moderate ______Severe Current GAF: Highest GAF: Client Name / Date of Birth / Medicaid #/ Member # Date of Service:
18. Treatment Recommendations:
Signature of Mental Health Professional: ______
Date: ______
Printed Name: ______
Signature of Supervisor (if applicable): ______Date: ______
Printed Name: ______