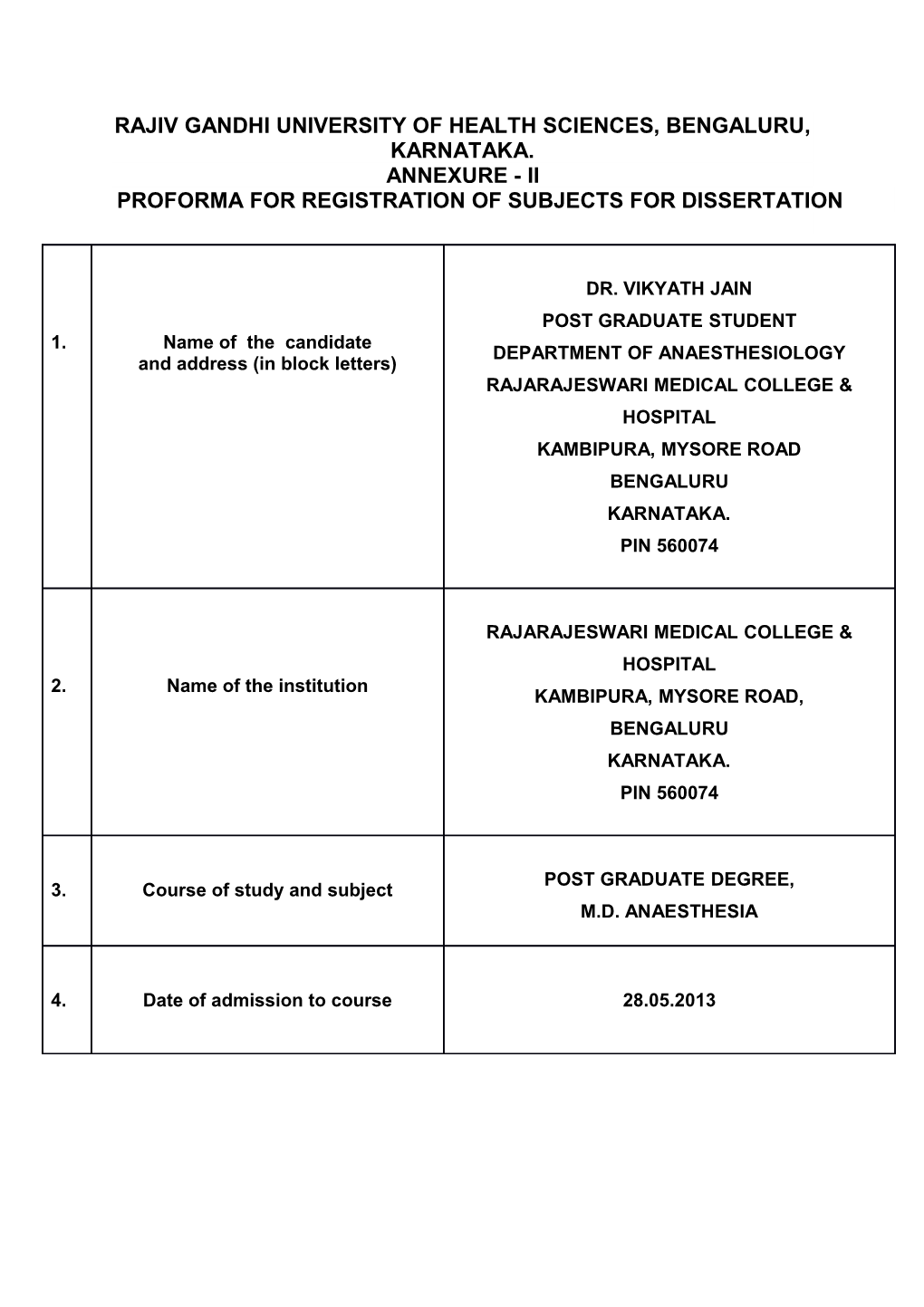
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES, BENGALURU, KARNATAKA. ANNEXURE - II PROFORMA FOR REGISTRATION OF SUBJECTS FOR DISSERTATION
DR. VIKYATH JAIN POST GRADUATE STUDENT 1. Name of the candidate DEPARTMENT OF ANAESTHESIOLOGY and address (in block letters) RAJARAJESWARI MEDICAL COLLEGE & HOSPITAL KAMBIPURA, MYSORE ROAD BENGALURU KARNATAKA. PIN 560074
RAJARAJESWARI MEDICAL COLLEGE & HOSPITAL 2. Name of the institution KAMBIPURA, MYSORE ROAD, BENGALURU KARNATAKA. PIN 560074
POST GRADUATE DEGREE, 3. Course of study and subject M.D. ANAESTHESIA
4. Date of admission to course 28.05.2013 " A COMPARISION OF TWO INSULIN REGIMEN FOR PERI-OPERATIVE GLYCEMIC CONTROL IN 5. Title of the topic PATIENTS WITH DIABETES MELLITUS UNDERGOING SURGERY UNDER GENERAL ANAESTHESIA "
6. BRIEF RESUME OF THE INTENDED WORK:
6.1 NEED FOR THE STUDY: Diabetes mellitus, is a group of metabolic diseases in which a person has high blood sugar, because the pancreas does not produce enough insulin, or cells do not respond to the insulin that is produced. India is often referred as the diabetes capital of the world. It is currently experiencing an epidemic of type 2 diabetes mellitus and has the largest number of diabetic patients. The International Diabetes Federation 2009 report reveals that the total number of diabetic subjects in India is 50.8 million. A population-based study, on the magnitude of the problem of diabetes was carried out in the KBN Medical College and Hospital, Gulbarga, during the period of April, 2009 to March, 2010. The result revealed that there was 19.78% prevalence of diabetes among the study participants [1] Patients with diabetes are more likely to undergo surgery than are people without diabetes. Maintaining glycemic control in subjects with diabetes presents a challenging problem during the perioperative period. Surgery in diabetic patients is associated with longer hospital stay, higher health care resource utilization, and greater perioperative mortality than nondiabetic subjects. The higher morbidity and mortality relates in part to the heightened incidence of coronary heart disease, hypertension, renal insufficiency, and increased rates of postoperative complications. In addition, several observational and interventional studies have indicated that hyperglycemia per se is associated with adverse clinical outcomes in surgical and critically ill patients [2] In hospitalized patients with hyperglycemia, three different components of insulin replacement require management: Basal insulin replacement consists of a long-acting insulin preparation administered regardless of the patient’s oral intake status, with the premise of matching hepatic (endogenous) glucose production Prandial insulin replacement requires a rapid-acting insulin preparation given to cover nutritional needs Supplemental (or correction) insulin replacement requires a rapid-acting preparation (usually the same insulin type as for prandial coverage) to correct blood glucose values that exceed predetermined glycemic targets. For most patients, basal insulin replacement might be appropriate preoperatively to control fasting glucose, whereas during surgery, especially if prolonged or high risk, an intravenous (IV) insulin drip is the most effective means of glucose control [3] Currently, there are no uniform standards and methods for perioperative glycemic control. In our study we are comparing sliding scale regimen with patients on bolus/basal insulin regimen.
6.2 REVIEW OF LITERATURE: The prevalence of Diabetes in Indians is reaching an epidemic scale. The prevalence of Type 2 Diabetes Mellitus in Asian Indians ranges from 2.7% in rural India to 14% in urban India by Gupta A et.al [4][5]
Indian J Public Health, Forhad Akhtar Zaman and colleagues in year 2011, describe diabetes mellitus is a multifactorial disease with both genetic and environmental factors contributing to its development. Diabetes has noteworthy involvement with hypertension, overweight, and obesity, and other long-term vascular complications as the main causes of morbidity and mortality. Recognizing the magnitude of the growing problem, a study was undertaken to assess the magnitude of the problem of diabetes and its association with hypertension, obesity, and positive family history [1]
Moghissi ES et.al say the recent consensus statement from the American Association of Clinical Endocrinologists and the American Diabetes Association recommends using insulin therapy if blood glucose levels exceed 180 mg/dL, with target glucose levels less than 180 mg/dL in critically ill patients and less than 140 mg/dL in non–critically ill patients [6]
Anesthesia may induce an increase in levels of stress hormones (epinephrine, cortisol, growth hormone) and inflammatory cytokines (interleukin-6 and tumor necrosis factor– alpha), resulting in insulin resistance and impaired insulin secretion (even among patients who present with adequate insulin secretion). These in turn contribute to lipolysis and protein catabolism, leading to hyperglycemia and, if a patient is severely insulin deficient, ketoacidosis by LUIGI F. MENEGHINI [7]
Dagogo-Jack S say, sustained hyperglycemia is a known risk factor for vascular endothelial cell dysfunction, infection, thrombosis, and non-healing postoperative surgical wounds [8]
Dronge AS et.al, say preoperative glycemic control has a significant impact on the risk of infectious complications including pneumonia, wound infection, urinary tract infection, and sepsis in patients with diabetes across a variety of surgical procedures [9]
Perioperative glycemic control can reduce morbidity, particularly the incidence of infectious complications, in surgical patients, even in those without diagnosed diabetes.
Joslin Clinical Guideline focuses on the unique needs of the patient with diabetes, designed to assist primary care physicians and specialists to individualize the care and set goals for adult patients with diabetes who are undergoing surgery[10]
7. 6.3 OBJECTIVES OF THE STUDY: a. Primary objective – To compare perioperative glycemic control in patients on sliding scale regimen with patients on bolus/basal insulin regimen.
b. Secondary objective – To compare baseline insulin and markers of stress during perioperative period.
MATERIALS AND METHODS:
7.1 Source of data: Diabetes Mellitus Patients admitted and posted for Elective Surgery in Rajarajeswari Medical College & Hospital.
7.2 Method of collection of data: (including sampling procedure if any): The data for study is collected from subjects fulfilling inclusion criteria/exclusion criteria and admitted as inpatients in RRMC&H Sample will be Number of patients who are coming to RRMCH for elective surgeries with diabetes mellitus from time of Nov-2013 to Nov-2015.
7.3 Regimens to be used for the study: Following 2 regimens will be used in the course of the study. - Regime A -- Sliding Scale method: Using Human Regular. Units Sugar Level 4 150-199mg/dl 8 200-249mg/dl 12 250-299mg/dl 16 300-349mg/dl 20 350-399mg/dl
- Regime B -- Basal & Bolus method: Using combination of 2 Insulin’s: NPH insulin and Human regular insulin, appropriate doses will be given according to patient’s needs.
STUDY DESIGN: A hospital based prospective, randomized controlled study.
STUDY PERIOD: 12-18 months.
INCLUSION CRITERIA: - Patients of age 18-65yrs with diagnosed Diabetes Mellitus. - Confirmed by Blood Sugar Level / HbA1c level. - Patients with ASA grade 1 – 3. - Patients willing to give consent. EXCLUSION CRITERIA: - Patients with ASA grade 4 and above - Patients with History of unstable coronary syndromes, or when considering coronary revascularization. - Patients with abnormal ECG &/or abnormal chest X ray - Patients with abnormal Liver function test[LFT] and Renal function test[RFT] - Patients with diabetic autonomic neuropathy. - Patients with history of allergy. - Patients participating in other research studies. - Patients with Blood sugar levels more than 200mg/dl.
Methodology of Study: Patients, aged 18 – 65years, admitted for elective surgery under general anesthesia will be included.
Written informed consent will be obtained from all participants before being enrolled in the study. The study is approved by the Ethical Review Committee, exclusion criteria is as same as mentioned above
Eligible subjects Detailed pre anesthetic checkup including history, clinical examination and all routine investigations like complete blood count, blood Sugar, LFT, RFT, Serum electrolytes, ECG and Chest X ray and will be screened and randomized into Regime A and Regime B and 2days prior to surgery they will be started on one of the two insulin regimes according to the regimes mentioned above. Patients will be monitored for GRBS everyday. On the day of surgery patient will be considered for surgery if blood sugar level less than 200mg/dl.
Patient will be premedicated with Inj Midazolam, Inj Glycopyrolate, Inj Fentenly. Patient will be preoxygenated for 3mins and Induced with Inj. Propofol and Inj Vecuronium and intubated with cuffed endotracheal tube and patient will be maintained with the Oxygen, Nitrous Oxide, Sevoflurane/Isoflurane. Patient’s Pulse, NIBP, SpO2, ETCo2 will be monitored throughout the procedure and study investigation will be done at 15mins, 1hour, 2hour for the GRBS, Serum Insulin, Serum Cortisol, Interlukine-6. Patients will be extubated after giving Reversal agent Inj.Neostigmine & Inj. Glycopyrolate. Intraoperatively if blood sugar level goes up 200mg/dl then insulin infusion will be started.
Postoperatively patients Pulse, NIBP, SpO2 will be moniterd and following investigations will be done- GRBS, Serum Insulin, Serum Cortisol, Interlukine-6 will be done at 15mins, 1hour, 3hours intervals. Patients will receive adequate analgesia, blood sugar will be monitored and as on sugar levels Oral Hypoglycemis will be started.
Statistical analysis will be performed using SPSS 20 version software, results will be expressed as Mean +/- SD, continuous variable will be analyzed using student‘t’ test between groups and intragroup comparisons will be done by paired ‘t’ test, categorical variable will be analyzed by Chi-sqare test.
7.3 DOES THE STUDY REQUIRE ANY INVESTIGATONS OR INTERVENTIONS TO BE CONDUCTED ON PATIENTS OR OTHER HUMANS OR ANIMALS? IF SO, PLEASE 8. DESCRIBE BRIEFLY:
1. Blood Sugar levels[ FBS / PPBS / RBS ] 2. Interleukins – 6 3. Serum. Cortisol 4. Blood Insulin Levels
7.4 HAS ETHICAL CLEARANCE BEEN OBTAINED FROM YOUR INSTITUTION IN CASE OF 7.3? YES
LIST OF REFERENCES: 1. Forhad Akhtar Zaman1.Glucose Indices, Frank and Undetected Diabetes in Relation to Hypertension and Anthropometry in South Indian Rural Population. Indian J Public Health. 2011 Jan-Mar;55(1):34-7.
2. Jacober SJ, Sowers JR. An update on perioperative management of diabetes. Arch Intern Med 1999;159:2405–2411.
3. Moghissi ES, Korytowski MT, DiNardo M, et al. American Association of Clinical Endocrinologists and American Diabetes Association consensus statement on inpatient glycemic control. Endocr Pract 2009; 15:353–369.
4. Gupta A, Gupta R, Sarna M, Rastogi S, Gupta VP,Kothari K. Prevalence of diabetes, impaired fasting glucose and insulin resistance syndrome in an urban Indian population. Diabetes Res Clin Pract 2003;61:69-76.
5. Ramachandran A, Snehalatha C, Kapur A, Vijay V, Mohan V, Das AK, et al . Diabetes Epidemiology Study Group in India (DESI): High prevalence of diabetes and impaired glucose tolerance in India-National Urban Diabetes Survey (NUDS). Diabetologia 2001;44:1094-101.
6. Moghissi ES, Korytowski MT, DiNardo M, et al. American Association of Clinical Endocrinologists and American Diabetes Association consensus statement on inpatient glycemic control. Endocr Pract 2009; 15:353–369.
7. LUIGI F. MENEGHINI. Perioperative management of diabetes: Translating evidence into practice. Cleveland Clinic Journal of Medicine November 2009vol. 76 Suppl 4 S53-S59.
8. Dagogo-Jack S, AlbertiKG. Management of diabetes mellitus in surgical patients. Diabetes Spectrum 2002; 15: 44-48.
9. Dronge AS, Perkal MF, Kancir S, et al. Long-term glycemic control and postoperative infectious complications. Arch Surg 2006; 141:375–380.
10.JOSLIN DIABETES CENTER and JOSLIN CLINIC GUIDELINE for INPATIENT MANAGEMENT OF SURGICAL and ICU PATIENTS with DIABETES [cited 10/02/09] Available from: http://www.joslin.org/docs/Inpatient_Guideline_10-02-09.pdf.
9 SIGNATURE OF THE CANDIDATE
Perioperative glycemic control is very important to 10 REMARKS OF THE GUIDE reduce morbidity. There are several new developments and new regimens being followed. This study will clear doubts about glycemic control in perioperative period.
Dr. RANGALAKSHMI S 11 NAME AND DESIGNATION OF: (IN PROFESSOR BLOCK LETTERS) DEPARTMENT OF ANAESTHESIA RRMC&H 11.1 GUIDE BENGALURU.
11.2 SIGNATURE (GUIDE) 11.3 CO-GUIDE(IF ANY) ---
11.4 SIGNATURE (Co –GUIDE) ---
DR. SAHAJANAND H 11.5 HEAD OF THE PROFFESOR AND HOD DEPARTMENT OF ANAESTHESIA DEPARTMENT RRMC&H BENGALURU.
11.6 SIGNATURE:
12 12.1 REMARKS OF THE CHAIRMAN
AND PRINCIPAL
12.2 SIGNATURE