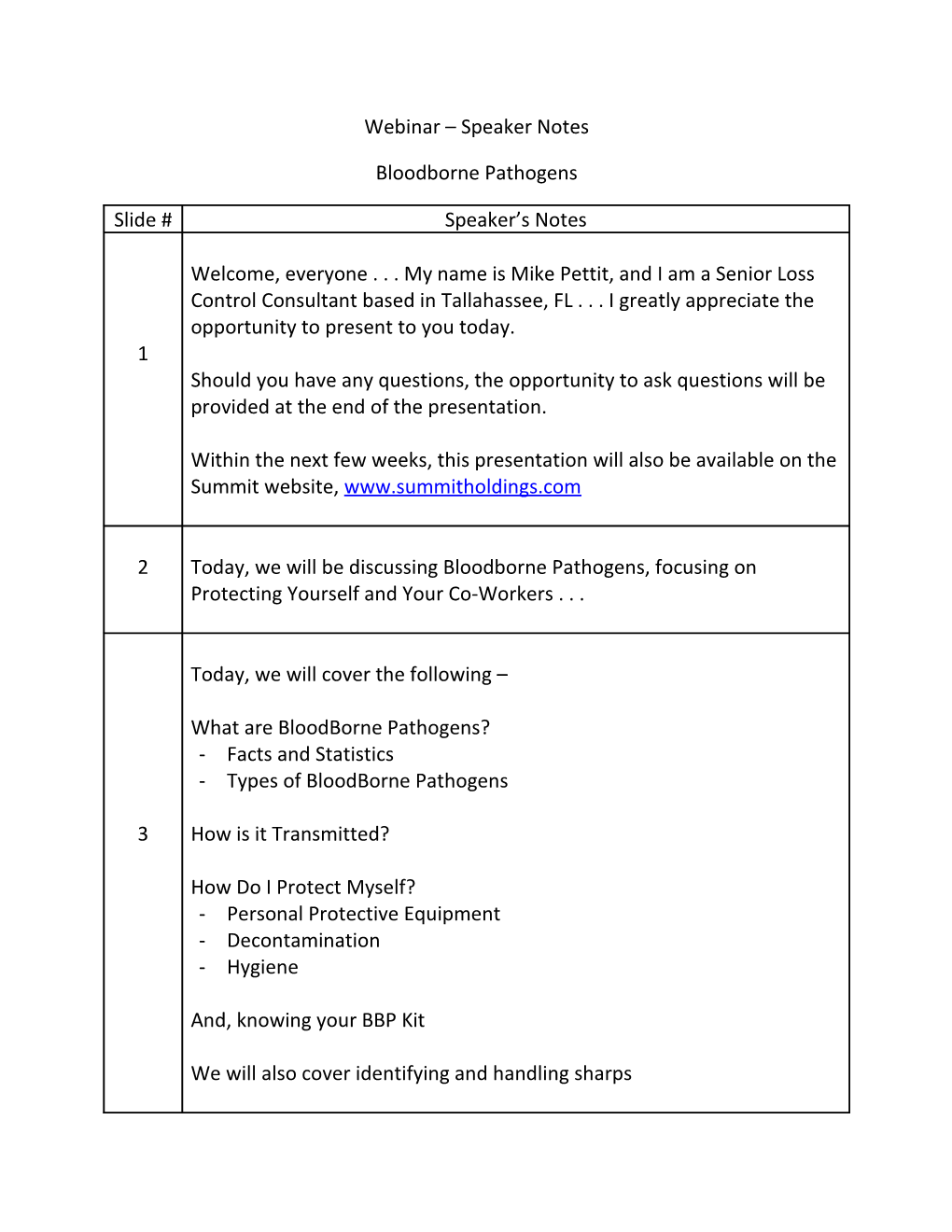
Webinar – Speaker Notes
Bloodborne Pathogens
Slide # Speaker’s Notes
Welcome, everyone . . . My name is Mike Pettit, and I am a Senior Loss Control Consultant based in Tallahassee, FL . . . I greatly appreciate the opportunity to present to you today. 1 Should you have any questions, the opportunity to ask questions will be provided at the end of the presentation.
Within the next few weeks, this presentation will also be available on the Summit website, www.summitholdings.com
2 Today, we will be discussing Bloodborne Pathogens, focusing on Protecting Yourself and Your Co-Workers . . .
Today, we will cover the following –
What are BloodBorne Pathogens? - Facts and Statistics - Types of BloodBorne Pathogens
3 How is it Transmitted?
How Do I Protect Myself? - Personal Protective Equipment - Decontamination - Hygiene
And, knowing your BBP Kit
We will also cover identifying and handling sharps So, What exactly are bloodborne pathogens? - By definition, Bloodborne Pathogens are microorganisms such as viruses or bacteria that are carried in blood and can cause disease in people 4 There are many different types of BBP but there are 2 types that OSHA specifically has in mind in regards to the Bloodborne Pathogen Standard. They are: - Hepatitis B (HBV) - Human Immunodeficiency Virus (HIV)
The reason for the focus here is because of the severity of these 2 diseases.
Let’s take the time to look at these two bloodborne pathogens. - As far as statistics are concerned, more than 300,000 people are infected with Hepatitis B each year in the US alone - that is far too many people.
The primary way that this disease is transmitted is through “blood to blood” contact. - If you have ever had your blood drawn or received a shot, this is why the nurses take such caution with the used needles. It is not because 5 they are afraid of getting stuck - there have been many advances in the medical field with “Safe” needle devices that enclose the needle before and after an injection, and a great deal of time and money has been spent coming up with products that help minimize this hazard. - The main reason nurses are so cautious is because they are working to avoid coming into contact with a bloodborne pathogen.
Most importantly, and as the 3rd bullet point indicates, there is no cure for Hepatitis B. Again, this is the reason for OSHA’s focus. There are some things that everyone needs to know when talking about Hepatitis B. - First of all, this virus is very durable - it will survive in dried blood for up to seven (7) days. That is why, no matter what, when attempting 6 to clean up or disinfect an area that has been possibly exposed to a bloodborne pathogen, you must use extreme caution.
In addition to housekeepers and janitors, responders should wear personal protective equipment (such as gloves, mask, etc.) which have been provided, as well as the safe work practices we will talk about today.
Symptoms of Hepatitis B exposure include . . . - Fatigue - Stomach pains - Nausea - Symptoms like a mild “flu” bug 7 - Loss of appetite - Jaundice - Darkened urine
Now these are just basic symptoms - any employee who believes they have come into contact with a blood borne pathogen should consult a physician immediately for proper diagnosis
After an exposure, it can take 1 to 9 months before symptoms even become noticeable - if you wait for symptoms to appear, it may be too late for treatment. This is why you have to seek medical attention after any exposure to make sure you receive the necessary treatment, if necessary. Hepatitis B is preventable before and after exposure. - You can be immunized before exposure with a series of 3 shots which, as you can see here, is 90% effective for up to 7 years.
8 Those not needing to be offered the series of shots include: - Those who previously received the series - Those who received antibody testing revealing they are immune; or, if - The vaccine is contradicted for medical reasons
Here you can see how Hepatitis B can also be combated post-exposure with a 2 step process - The first step is the vaccination series 9 - The second step is the immune globulin, which must be administered within one week of exposure. Together, these steps are 90% effective in controlling the disease. This is another example of why you must seek medical attention right away if exposed.
The other main bloodborne pathogen that OSHA is concerned with is the Human Immunodeficiency Virus, or HIV.
AIDS, or immune deficiency syndrome, is caused by the virus HIV. Once a 10 person is infected with HIV, it may take many years before they develop AIDS.
The way HIV works is that it attacks the body’s immune system and weakens it to the point it cannot fight other diseases.
Here are some facts associated with HIV - Over 35,000 people are infected every year in the United States. - AIDS is a fatal disease because there is no known cure at this time - 11 there have been a great deal of advancements made to extend your life span, but, again, there is no cure
As previously stated, you are strongly encouraged to immediately seek medical attention if you believe you may have contracted this virus. Unlike Hepatitis B, HIV is very fragile and cannot survive very long outside the human body - remember, Hepatitis B can last up to 7 days outside the human body 12 Providing medical care such as first aid is a situation where the HIV virus could be transmitted should the person in need or even the person administering the treatment has HIV.
As you can see in this slide, there is only a .4% chance for contracting AIDS in the workplace. However, given the consequences, all precautions must be taken.
Some of the basic symptoms from HIV infection include: - Weakness - Fever - sore throat - nausea - headaches 13 - a white coating on the tongue - weight loss - swollen lymph glands o If you remember from Hepatitis B, they sound very similar - almost flu-like
Again, these symptoms may take weeks to show - only a doctor can determine whether or not you have been infected. So what are some of the ways these bloodborne pathogens can be transmitted? 14 First of all, Hepatitis B, HIV, and other blood borne pathogens may be present in Blood and other body fluids
In order to cause infection . . .(next slide) . . .
. . . The virus must have a way to enter your body. Some likely ways are:
- Sexual contact with an infected partner - Sharing infected needles - Cutting yourself with a sharp object that is contaminated with infected blood or fluids 15 - Getting infected blood or fluids on your skin if you have open sores, nicks or cuts; - Getting contaminated blood or fluids in the mucous membranes in your eyes, nose or mouth, which is where proper hygiene comes into play in avoiding these exposures
Your skin is normally a protective barrier to keep viruses out, but if you have dermatitis, acne, chapped hands or broken cuticles, you have ways for the HIV or HBV to enter your body.
As we see in this slide, the OSHA Standard requires training - At time of initial assignment where exposure to blood or other 16 potential infectious materials may take place - Retraining efforts should then be provided every year, thereafter
Training must also include (next slide) . . . - Hepatitis B vaccine information - Explanation of related symptoms - post-exposure follow-up procedures 17 - means of transmission, as well as - the location and handling of personal protective equipment
We have already reviewed HIV and Hepatitis B information, symptoms, and post-exposure follow-up procedures – we will include the remaining and additional aspects during the remainder of this presentation, starting with prevention . . .
- If you choose to help an injured co-worker, always take time to put on a pair of leak-proof gloves and wear them under your regular work gloves. Also, make sure you are wearing eye protection to 18 prevent the transmission of blood borne pathogens through the eyes. - If you get blood or other potentially infectious materials on your skin, immediately wash with soap and water
- If potentially infectious materials get in your eyes, nose or mouth, 19 immediately flush with running water at a sink or eyewash fountain.
You should report any unprotected contact with blood or other bodily fluids to your supervisor so proper medical follow-up can be made When blood or body fluids are being cleaned up after an accident, you should always: - Restrict access to the area – this is to keep others from becoming exposed; you should also . . . - Wear two pairs of leak-proof gloves – do everything possible to avoid tearing the gloves 20 - Wear a leak-proof apron to protect your clothes - Do not pick up contaminated sharp objects (glass, nails, sharp metal, etc.) with your hands--sharp objects might cut both your glove and your hands. Use brooms and dust pans or tongs to pick up these objects. - Use disposable towels to soak up most of the blood
You must also (next slide) . . . - Place all contaminated towels and waste in sealed, color-coded or labeled leak-proof container - these are included in BBP kits - Dispose of as a regulated waste - Don’t just toss it in the dumpster, as you may need to contact you sanitation provider on how they would want you to handle this effort 21 - Clean with an appropriate disinfecting solution - A solution of 10 parts water to 1 part bleach will kill both HIV and the Hepatitis B Virus - After cleaning, promptly disinfect mops and any other cleaning equipment – otherwise, you may spread viruses to other areas of the facility So, How do I know if what I am cleaning is infected with a BBP? - The best rule of thumb is to use Universal Precautions - Since you don’t know who might be infected, the best rule of thumb is to use Universal Precautions, which is to treat all blood and body fluids as if they are infected. 22 - It only takes one exposure to become infected--Don’t Take Chances. - Assume the worst when cleaning, and properly protect yourself during these efforts
Fortunately, HIV and the Hepatitis B Virus aren’t spread through the air like cold or flu germs. You can’t get either disease from working alongside someone who is infected, or from casual contact. Now let’s talk about the various types of Personal Protective Equipment
You must: 23 - Always wear PPE in exposure situation - this could be gloves, goggles, aprons and so on - You must remove and/or replace Personal Protective Equipment that is damaged, such as those torn, punctured, or showing signs of wear - And, you must remove Personal Protective Equipment before leaving the work area - don’t risk exposing other areas or people
The first thing to do to protect yourself is to wear personal protective equipment such as latex or protective gloves. This prevents blood from coming in contact with your skin.
Before putting on latex gloves, it is also important to make sure that whoever is putting on the gloves does not have a latex allergy. In this case, another type of glove besides latex must be used.
- GLOVES should be made of an impervious material - if gloves are thin 24 or flimsy, double gloving can provide an additional layer of protection. - Also, if you know you have cuts or sores on your hands, you should cover with a bandage or similar protection as an additional precaution before donning your gloves. - Prior to putting them on, inspect your gloves for tears or punctures; if the gloves are damaged, DO NOT USE THEM!
And, as the next slide shows, we should take special precaution when removing gloves wit bare skin . . . (Next slide) . . . - All attempts should be made as to not touch the outside of the gloves with any bare skin
- First, you should disinfect gloves in solution, if possible 25 - Second, grasp the palm of the glove with the other hand, and remove that glove inside out
- Then, slide a finger down the wrist of the gloved hand, and remove the second glove inside out
As a reminder, the gloves should then be disposed of properly
The next type of Personal Protective Equipment we will discuss is eye protection – if there is any potential risk of splashing contaminated 26 fluids, you should wear eye protection.
- As you can see from this slide, splashing can occur while: • cleaning up a spill • while providing first aid or medical assistance.
- Consideration should also be made to only allow trained employees to provide first aid to other employees. Face shields and masks, and aprons and gowns are other forms of PPE
- Face Shields and Masks should be worn in addition to goggles or glasses, as they will provide additional protection against splashes to the nose and mouth. 27 - Aprons and Gowns should be worn to protect your clothing, and to keep blood or other contaminated fluids from soaking through to your skin.
If your clothes become contaminated, they should be laundered immediately - contaminated laundry should be handled as little as possible, and should be placed in an appropriate labeled bag or container until it is decontaminated, dispose of, or laundered.
With the exposures any employee could face, the extensive use of PPE will more than likely never occur. But, for educational reasons, we are still covering it during this presentation.
When it comes to Personal Protective Equipment, it must be: - Appropriate to the task – don’t wear safety glasses when you need goggles, and don’t wear cotton gloves that could soak up fluids when you should be wearing latex gloves - The PPE must also be readily available – You must have the equipment at your location - It must also be readily accessible - If you can’t get to it to use it, what 28 good will it be? - Personal Protective Equipment must also be properly maintained – Damaged PPE provides little to no protection. - And, Personal Protective Equipment must be used – all the training in the World and all of the gloves and goggles you could find do no good if it is not used – PPE is provided to prevent you from becoming infected.
Keep in mind – Personal Protective Equipment is free to employees - efforts have been made to keep everyone safe at work. Hygiene is also crucial when dealing with bloodborne pathogens!
- Wash any area of the body that comes into contact with infectious 29 materials thoroughly with soap and water
- For splashes into the eyes, flush eyes with running water for At least 15 minutes
- After removing PPE, wash hands with soap and water for At Least 20 Seconds
Proper hygiene will help keep you from exposing yourself after the fact.
Now we must decontaminate the area.
So, what exactly needs to be decontaminated?
30 - All exposed work surfaces such as floors, counters, sinks, etc. - All pails, bins, and/or receptacles that have come into contact with the Bloodborne Pathogen – As a note, we must also decontaminate broken glassware Before disposal
Why do we clean it before we dispose of it? Remember, Hepatitis B can live for 7 days. We must make sure that in the event someone else down the road comes into contact with it, they are not at risk of becoming infected - we will cover broken glassware decontamination efforts more comprehensively later in the presentation So how do we decontaminate?
You should always decontaminate after spills, and at the completion of the task 31 A simple recipe you can even use in your own home to decontaminate surfaces is to add ¼ cup bleach to 1 gallon of water
Please notice we are adding the bleach to the water - if we add the bleach first, we risk splashing bleach on ourselves - always add the concentrate to the water, not the water to the concentrate.
Give the solution time to work – usually, 10 minutes is a good rule of thumb
Never eat, drink, smoke, apply cosmetics, or handle contact lenses if you are working in an area where there is possible exposure – this is to prevent becoming infected through the mucus membranes, such as the 32 eyes and the mouth.
In addition, no food or drink is permitted in laboratories or lab refrigerators designated for lab use - same as the other point - it can be spread and enter the body through our mouths
Use warning labels Post the biohazard symbol similar to the one on this slide; Use red bags / containers; and, 33 Post signage – agent, entry requirement, contact info - All of these are included in BBP kits
Also, provide training – inform everyone of the hazards of Bloodborne Pathogens, and how to protect themselves and others If I were to visit your workplace and ask, “Where is your BBP kit located?,” could everyone provide an accurate answer?
34 Remember, the kit must be readily available and it must be readily accessible - those performing the assistance must know where it is located at all times
What else is available in the Bloodborne Pathogens Kit? Other items include: Gloves 35 - Bio hazard bags - Antiseptic cleaners; and, - Goggles
What else is available? - We should know what is included in the kit, and be knowledgeable of how to use them . . .
As previously reviewed, broken glassware that has been visibly contaminated with blood must be sterilized with an approved 36 disinfectant solution before it is disturbed or cleaned up - this can be the solution we spoke of earlier with the 10% bleach and 90% water mix.
After spraying the glass with the solution, carefully use brooms and dust pans, or tongs, disposing of the items in an appropriate sharps container similar to the one shown on this slide –
This type of container is designed to prevent glass from protruding through the sides and possibly coming into contact with the person handling the waste
Again, please keep in mind . . . only those trained should be handling these items. Look for warning labels to be affixed to containers of regulated waste, refrigerators, and/or freezers containing blood or other potentially infectious material.
The labels should be - florescent red 37 - orange - and/or orange-red
For additional information, you are encouraged to contact the EPA at the listed phone number or website
Again, this pertains more to OSHA’s standard for BBP training, and not necessarily something you would come across on a routine basis.
To reiterate the previous discussion, if you suspect you have potentially 38 been exposed to any Bloodborne Pathogen, you must seek medical attention
- Go to the nearest medical facility - the quicker you take action, the better you chances are of avoiding any life-long consequences
When responding to an exposed worker 39 - Arrange for an immediate and confidential medical evaluation - Document how the exposure occurred – this is for both medical needs, as well as future preventative measures - Identify and test the source individual, if possible – this is the person who is bleeding . . . You should then (next slide) . . .
- Have the exposed employee’s blood tested - some of the medical attention received by the person exposed to the blood will depend 40 on whether or not there has been an infectious exposure - You should also provide counseling, and - Evaluate any reported illness When an exposure is experienced, a confidential medical evaluation and 41 follow-up is available – only the affected individual, the medical provider, and an assigned company representative have access to the information – it is not shared with other employees
42 Medical records are available to employees at all times, and a copy can be provided to the employee at the conclusion of employment
The medical records provided to an employee must include the information listed on this slide: 43 - Employee name and social security # - Status of Hepatitis B vaccination, and - The results of all exams, testing, and follow-up efforts
The medical records should also include (next slide) . . .
- A copy of the physician’s professional opinion, which would include 44 diagnosis, treatment, etc. - And, a copy of the information provided to the healthcare professional
Due to the hazards recognized by OSHA in regards to Bloodborne 45 Pathogens exposures, OSHA Standards require exposure control plans for every employer
These plans must include (next slide) . . . - A policy statement, - The steps needed to be taken to determine employee exposure, as well as - The implementation of control measures 46 Control Measures include: - Universal Precautions (again, this is treating all blood as though it is contaminated or infectious) - Engineering and work practice controls (eliminating, when possible, all potential contamination exposures - Personal Protective Equipment; and, - Housekeeping and post-exposure clean-up procedures
The Plans must also include (next slide) . . .
- The offer to provide the Hepatitis B vaccination - The post-exposure evaluation and follow-up efforts - Communicating the hazards to employees through training 47 - Maintaining required recordkeeping efforts; and, - The procedures for evaluating circumstances surrounding exposure incidents such as accident investigations
On a side note - the employee has the option to decline vaccination; if the vaccination is declined, he or she should be requested to sign a form of declination
48 At this website, a sample Exposure Control plan is available through OSHA – within a few weeks, this presentation and link will be available on the Summit website at www.summitholdings.com Remember, for an individual to receive the necessary treatment following an exposure, Time is of the Essence! 49 An employee should immediately inform his or her supervisor of a potential exposure, and the sequence of events previously provided must be initiated
50 Thank You for participating in this web-based training presentation – at this time, the muting function on the phones will be removed as to allow any questions you may have . . .