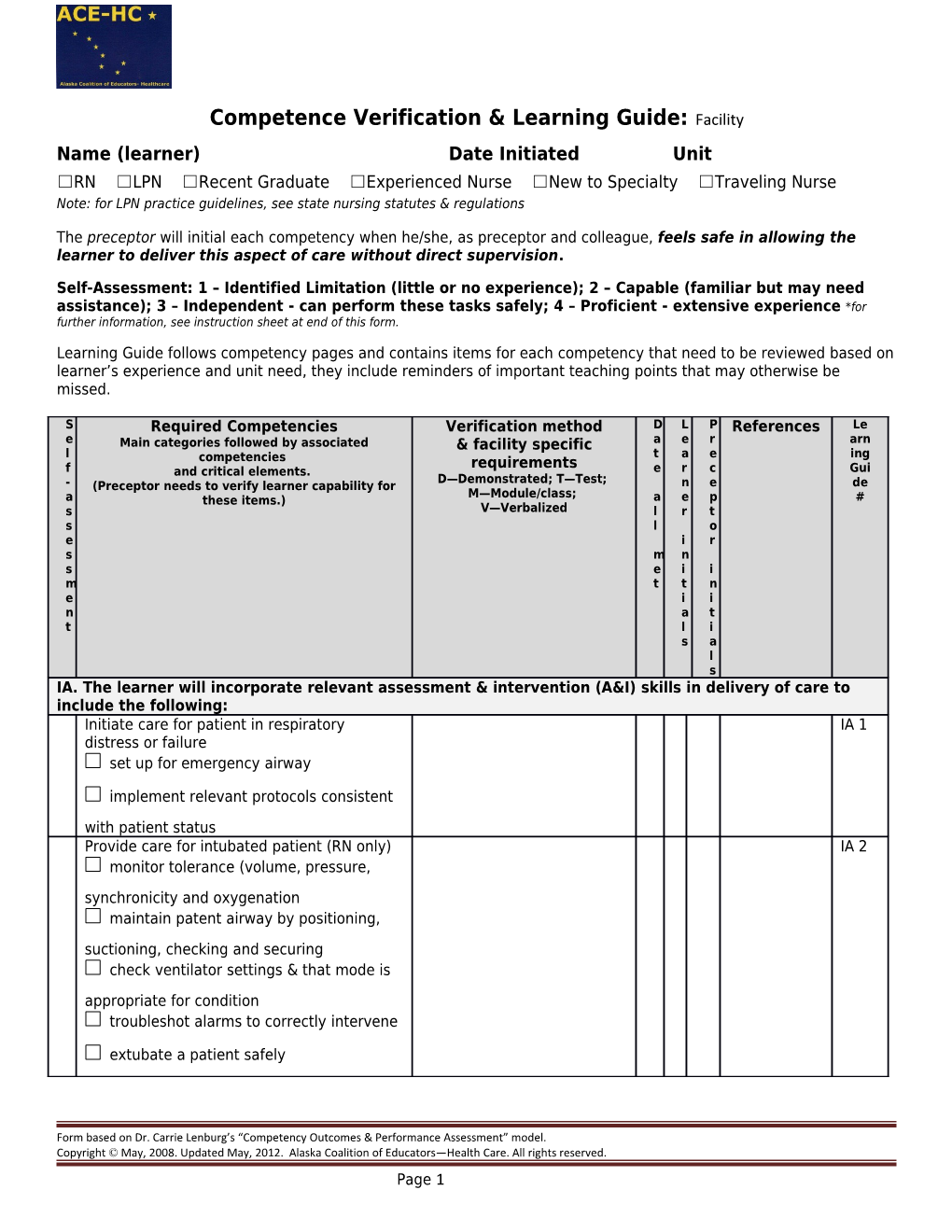
Competence Verification & Learning Guide: Facility Name (learner) Date Initiated Unit ☐RN ☐LPN ☐Recent Graduate ☐Experienced Nurse ☐New to Specialty ☐Traveling Nurse Note: for LPN practice guidelines, see state nursing statutes & regulations
The preceptor will initial each competency when he/she, as preceptor and colleague, feels safe in allowing the learner to deliver this aspect of care without direct supervision.
Self-Assessment: 1 – Identified Limitation (little or no experience); 2 – Capable (familiar but may need assistance); 3 – Independent - can perform these tasks safely; 4 – Proficient - extensive experience *for further information, see instruction sheet at end of this form.
Learning Guide follows competency pages and contains items for each competency that need to be reviewed based on learner’s experience and unit need, they include reminders of important teaching points that may otherwise be missed.
S Required Competencies Verification method D L P References Le e Main categories followed by associated & facility specific a e r arn l t a e ing competencies requirements f and critical elements. e r c Gui D—Demonstrated; T—Test; - (Preceptor needs to verify learner capability for n e de M—Module/class; a these items.) a e p # s V—Verbalized l r t s l o e i r s m n s e i i m t t n e i i n a t t l i s a l s IA. The learner will incorporate relevant assessment & intervention (A&I) skills in delivery of care to include the following: Initiate care for patient in respiratory IA 1 distress or failure set up for emergency airway
implement relevant protocols consistent with patient status Provide care for intubated patient (RN only) IA 2 monitor tolerance (volume, pressure, synchronicity and oxygenation maintain patent airway by positioning, suctioning, checking and securing check ventilator settings & that mode is appropriate for condition troubleshot alarms to correctly intervene
extubate a patient safely
Form based on Dr. Carrie Lenburg’s “Competency Outcomes & Performance Assessment” model. Copyright © May, 2008. Updated May, 2012. Alaska Coalition of Educators—Health Care. All rights reserved. Page 1 S Required Competencies Verification method D L P References Le e Main categories followed by associated & facility specific a e r arn l t a e ing competencies requirements f and critical elements. e r c Gui D—Demonstrated; T—Test; - (Preceptor needs to verify learner capability for n e de M—Module/class; a these items.) a e p # s V—Verbalized l r t s l o e i r s m n s e i i m t t n e i i n a t t l i s a l s Integrate ABG results into care (RN only) IA 3 interpret results correctly
act to correct abnormalities
Initiate care of patient with cardiac IA 4 emergency per protocols Identify ischemia, injury or infarct on a 12 IA 5 lead ECG Provide care for client with transvenous or IA 6 transcutaneous pacemaker per policy (RN only) demonstrate setting rate and sensitivity and stimulation thresholds identify complications
Provide care for patient with hemodynamic IA 7 monitoring(RN only) check for safety (balloon, placement, etc.)
correctly performs monitoring/calculations remove catheter safely
zero and calibrate lines
troubleshoot waveform changes
intervene as needed
Use bedside and central monitors for all IA 8 pertinent functions
Apply interventions for sepsis as indicated IA 9
Provide initial burn treatment per protocols IA 10
Form based on Dr. Carrie Lenburg’s “Competency Outcomes & Performance Assessment” model. Copyright © May, 2008. Updated May, 2012. Alaska Coalition of Educators—Health Care. All rights reserved. Page 2 S Required Competencies Verification method D L P References Le e Main categories followed by associated & facility specific a e r arn l t a e ing competencies requirements f and critical elements. e r c Gui D—Demonstrated; T—Test; - (Preceptor needs to verify learner capability for n e de M—Module/class; a these items.) a e p # s V—Verbalized l r t s l o e i r s m n s e i i m t t n e i i n a t t l i s a l s Apply interventions for brain hemorrhage or IA 11 trauma per protocols
Manage patient with intracranial pressure IA (ICP) monitor (RN only) 12 identify waveforms, cerebral perfusion pressure (CPP), patient symptoms and their significance implement measures to decrease/minimize increases in ICP Monitor patient to identify complications of IA 13 critical illness
Integrate measures to ensure patient safety IA 14 in the unit setting Administer IV drips IA 15 calculate drip rate correctly
titrate drip per orders/need
wean drips per protocols
Correlate clinical condition with drug IA 16 indications, desired effects, dosage and contraindications for commonly given IV drips Optimize patient comfort with sedation, pain IA 17 control and paralytics
Administer chemotherapy safely (RN only) IA 18 check dosing per policy
state hazardous waste precautions
Form based on Dr. Carrie Lenburg’s “Competency Outcomes & Performance Assessment” model. Copyright © May, 2008. Updated May, 2012. Alaska Coalition of Educators—Health Care. All rights reserved. Page 3 S Required Competencies Verification method D L P References Le e Main categories followed by associated & facility specific a e r arn l t a e ing competencies requirements f and critical elements. e r c Gui D—Demonstrated; T—Test; - (Preceptor needs to verify learner capability for n e de M—Module/class; a these items.) a e p # s V—Verbalized l r t s l o e i r s m n s e i i m t t n e i i n a t t l i s a l s Perform role during a high risk unit IA 19 procedure set up for procedure
provide nursing assistance during procedure monitor patient during and after for complications Respond to hospital emergencies per policy IA 20
Operate specialty equipment per manuals IA 21 and policies
Comments/alternative learning plans:
All preceptors are to sign & initial below. Ideally new graduates should have only one to two preceptors for the entire orientation.
Preceptor Signature Initials Preceptor Signature Initials
Signatures at completion of preceptorship/orientation:
Preceptee/orientee Date
Form based on Dr. Carrie Lenburg’s “Competency Outcomes & Performance Assessment” model. Copyright © May, 2008. Updated May, 2012. Alaska Coalition of Educators—Health Care. All rights reserved. Page 4 Primary Preceptor Date
Manager Date
Form based on Dr. Carrie Lenburg’s “Competency Outcomes & Performance Assessment” model. Copyright © May, 2008. Updated May, 2012. Alaska Coalition of Educators—Health Care. All rights reserved. Page 5 LEARNER GUIDE: Reference items in right-hand column that needs review. IA. The learner will incorporate relevant assessment & intervention (A&I) skills in delivery of care to include the following: IA 1 Initiate Care for patient in respiratory distress Review P & P and equipment for emergency respiratory or failure management including CPAP, BiPAP Review emergency airways: ETT, cricothyrotomy, tracheostomy
IA 2 Provide Care for intubated patient Review ventilator and intubation protocols, equipment, standing orders, and troubleshooting Review initiation and indications for jet vent if applicable Review SVO2 monitoring, set up and data analysis if done in unit Review extubation protocols
IA 3 Integrate ABG results into care Review ABG norms and interpretation of changes -complete checklist for drawing ABG’s if applicable -correctly verbalize ways to correct abnormalities
IA 4 Initiate care of patient with cardiac Review the following unit protocols emergency per protocols -initial chest pain management -dysrhythmias -significant BP change -CHP or pulmonary edema -cardiogenic shock -cardiac arrest -code cart management
IA 5 Identify ischemia, injury or infarct on a 12 Review ECG interpretation lead ECG IA 6 Provide care for client with transvenous or Review equipment, manufacturers recommendations, safety transcutaneous pacemaker considerations, how to operate the pacer, pacing modes Review complications: failure to pace, failure to sense, failure to capture, dysrhythmias, burns & pain (with transcutaneous)
IA 7 Provide care for patient with hemodynamic Review hemodynamic parameters monitoring -correctly performs monitoring/calculations -remove catheter safely -zero and calibrate lines -troubleshoot waveform changes -intervene as needed Review lines and monitoring equipment and practice with it Review protocols for changes in patient status
IA 8 Use bedside and central monitors for all Review setting parameters, calculating functions, changing pertinent functions modules, troubleshooting
IA 9 Apply interventions for sepsis as indicated Review protocols, fever reduction methods, circulatory support including vasoactive drips
IA Provide initial burn treatment per protocols Review procedures and initial burn management protocol 10 Review fluid replacement protocol, wound management and transfer criteria/procedure
Form based on Dr. Carrie Lenburg’s “Competency Outcomes & Performance Assessment” model. Copyright © May, 2008. Updated May, 2012. Alaska Coalition of Educators—Health Care. All rights reserved. Page 6 LEARNER GUIDE: Reference items in right-hand column that needs review. IA Apply interventions for brain hemorrhage or Review policy and pathophysiology and treatment of CVA, 11 trauma per protocols subarachnoid, subdural/epidural hemorrhage, trauma related damage and swelling Review radiology and neurology resources Review coma scale and interventions
IA Manage patient with intracranial pressure Review policies and manual for ICP monitor 12 (ICP) monitor -identify waveforms, cerebral perfusion pressure (CPP), patient symptoms and their significance -implement measures to decrease/minimize increases in ICP
IA Monitor patient to identify complications of Review protocols, labs and medications for the following: DIC, 13 critical illness PE, DVT, stroke, skin breakdown, delirium, line infection, medication & blood reactions, renal insufficiency & failure
IA Integrate measure to ensure patient safety in Review the following: 14 the unit setting -skin breakdown prevention -ventilator acquired pneumonia prevention protocol -visitor policy and teaching -equipment safety -spinal precautions, collar fit, alignment, turning &transferring
IA Administer IV drips Review all related policies, protocols and standing orders for 15 commonly used IV drips -calculate drip rate correctly -titrate drip per orders/need -wean drips per protocols
IA Correlate clinical condition with drug Review the following medications: dopamine, dobutamine, 16 indications, desired effects, dosage and norephinephrine, epinephrine, nitroglycerine, nitroprusside, contraindications for commonly given IV drips diltiazem, lidocaine, amiodarone, thrombolytics, procainamide, potassium, aminophylline, heparin, insulin, octreotide and others used in unit
IA Optimize patient comfort with sedation, pain Review sedation and pain scales and interventions 17 control and paralytics Review use of and interpretation of results from peripheral nerve stimulator Review policy for procedural sedation and complete any facility required training and or checklists
IA Administer chemotherapy safely Review policy and complete any facility required training 18 and/or checklists Review hazardous waste precautions and spill response
IA Perform nursing role during a high risk unit Review procedure, equipment and risks of: thoracotomy, 19 procedure thoracentesis, pericardiocentesis, lumbar puncture, central line insertions, arterial line insertions and monitoring, hemodynamic pressure monitoring, Sengstaken-Blakemore tube, cardioversion, external pacing, endoscopy, chest tube
IA Respond to hospital emergencies per policy Review policy and role in emergency response throughout 20 hospital
Form based on Dr. Carrie Lenburg’s “Competency Outcomes & Performance Assessment” model. Copyright © May, 2008. Updated May, 2012. Alaska Coalition of Educators—Health Care. All rights reserved. Page 7 LEARNER GUIDE: Reference items in right-hand column that needs review. IA Operate specialty equipment per manuals Review manuals and facility policy for operating fluid/blood 21 and policies warmer, rapid transfuser, hypo/hyperthermia blanket, PCA pump, epidural
Other facility specific items to cover:
Form based on Dr. Carrie Lenburg’s “Competency Outcomes & Performance Assessment” model. Copyright © May, 2008. Updated May, 2012. Alaska Coalition of Educators—Health Care. All rights reserved. Page 8 REQUIREMENTS: All nurses will complete these competencies upon hire. Some competencies may be reviewed annually. This form follows the Competency Outcomes and Performance Assessment (COPA) model.
PRECEPTEE/LEARNER INSTRUCTIONS: Complete self-assessment: Rate your skill in each area to identify the areas where you need additional experience, access to teaching resources, and/or lab practice. Discuss your results with your preceptor to help establish a plan and goals for your learning experience and to aid in choosing patient assignments. Scoring per instructions at the top of page 1.
PRECEPTOR INSTRUCTIONS: A. Review self-assessment with preceptee/learner to establish plan. B. Required Competencies: The specialty area competency forms are required for independent practice on this unit. This column represents the Alaska Statewide required competencies per ACE-HC and should not be altered. The preceptor will sign each one off when he/she, as preceptor and colleague, feels safe in allowing the preceptee/learner to deliver this aspect of care without direct supervision. C. Verification Method & Agency Specific. Document comments/check marks for the competency and any agency specific requirements. Verification methods include: 1. Demonstration – Preceptor watches learner perform task/procedure in safe, capable manner in a simulated lab or computer setting or as part of direct care performance. The expectation for new graduates is that they demonstrate as many of the competencies as possible. 2. Test – Learner passes a test provided by the facility to measure competence for this skill. (Minimum passing grade indicated. Initial only after test passed.) 3. Module –Learner has completed a training tool (computerized or written module, class, video, etc.) provided by the facility to measure competence for this skill. 4. Verbalization - Learner explains to the preceptor the process and/or planning that evidences safe, reliable knowledge base. This may include case scenarios, discussion, and/or description of plan. NOTE: some competencies may have the verification method specified per facility guidelines (e.g. “test only”) Record N/A and initials only for items that never apply to this learner’s role or performance. D. Sign-off: Sign and date when all elements of the competency are met. If unable to sign off an area due to patient population issues or learner needs more time, document a plan in the comments section at the end of the form. Discuss alternative ways of meeting the requirement(s) as well as any additional time needed with the nurse manager and/or nurse educator. All preceptors assisting in orientation of a new staff member/intern must sign and initial in the signature chart at the end of this document. E. References: Competencies should be met in accordance with these. Add your facility approved references here. F. Learning Guide: These are memory ticklers. The amount of time spent on each of them depends on the learner’s experience. New graduates will likely need time on almost all of the areas listed.
REFERENCES COLUMN: List foundational documents to support the learning experience and to use as the official measure by which the competencies are assessed. The ACE-HC group recognizes the following as sources for evidence based practice that can be included in the reference list along with local policies, procedures and forms: Perry & Potter, Elsevier/Mosby, Lippincott, Kozier & Erb, ANA, nationally recognized hospital related regulatory organizations (CLIA, CDC, CMS, JC, etc.), and specialty nursing organizations’ scope, standards and core curricula. This column’s content may be changed to be facility specific.
NOTE: ACE-HC competency forms are intended to be used between facilities within Alaska.
Form based on Dr. Carrie Lenburg’s “Competency Outcomes & Performance Assessment” model. Copyright © May, 2008. Updated May, 2012. Alaska Coalition of Educators—Health Care. All rights reserved. Page 9