Small strokes causing acute vestibular syndrome Saber Tehrani, et al.
Online Supplement for “Small Strokes Causing Severe Vertigo―Frequency of False- Negative MRIs and Non-Lacunar Mechanisms” (Saber Tehrani, et al.)
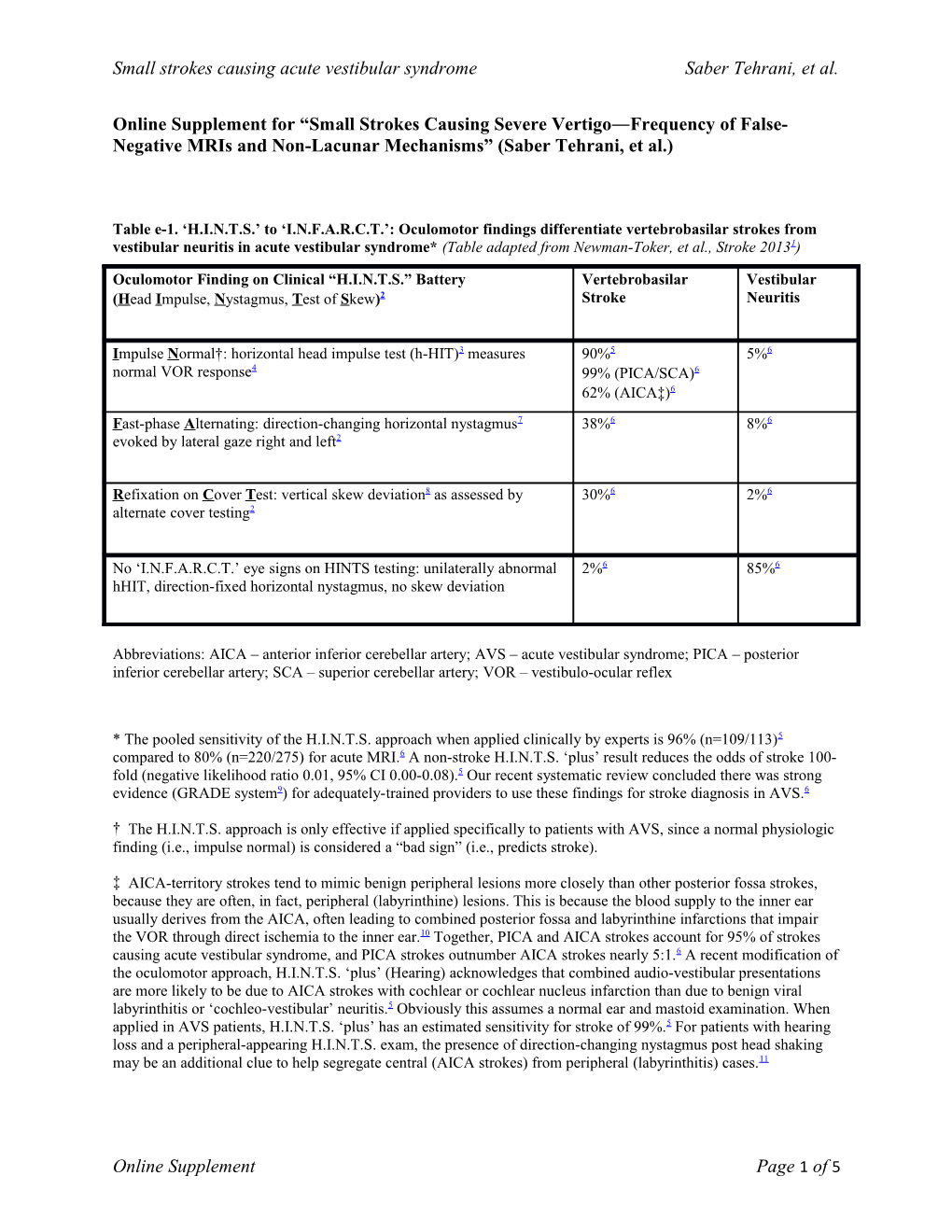
Table e-1. ‘H.I.N.T.S.’ to ‘I.N.F.A.R.C.T.’: Oculomotor findings differentiate vertebrobasilar strokes from vestibular neuritis in acute vestibular syndrome* (Table adapted from Newman-Toker, et al., Stroke 20131)
Oculomotor Finding on Clinical “H.I.N.T.S.” Battery Vertebrobasilar Vestibular (Head Impulse, Nystagmus, Test of Skew)2 Stroke Neuritis
Impulse Normal†: horizontal head impulse test (h-HIT)3 measures 90%5 5%6 normal VOR response4 99% (PICA/SCA)6 62% (AICA‡)6 Fast-phase Alternating: direction-changing horizontal nystagmus7 38%6 8%6 evoked by lateral gaze right and left2
Refixation on Cover Test: vertical skew deviation8 as assessed by 30%6 2%6 alternate cover testing2
No ‘I.N.F.A.R.C.T.’ eye signs on HINTS testing: unilaterally abnormal 2%6 85%6 hHIT, direction-fixed horizontal nystagmus, no skew deviation
Abbreviations: AICA – anterior inferior cerebellar artery; AVS – acute vestibular syndrome; PICA – posterior inferior cerebellar artery; SCA – superior cerebellar artery; VOR – vestibulo-ocular reflex
* The pooled sensitivity of the H.I.N.T.S. approach when applied clinically by experts is 96% (n=109/113)5 compared to 80% (n=220/275) for acute MRI.6 A non-stroke H.I.N.T.S. ‘plus’ result reduces the odds of stroke 100- fold (negative likelihood ratio 0.01, 95% CI 0.00-0.08).5 Our recent systematic review concluded there was strong evidence (GRADE system9) for adequately-trained providers to use these findings for stroke diagnosis in AVS.6
† The H.I.N.T.S. approach is only effective if applied specifically to patients with AVS, since a normal physiologic finding (i.e., impulse normal) is considered a “bad sign” (i.e., predicts stroke).
‡ AICA-territory strokes tend to mimic benign peripheral lesions more closely than other posterior fossa strokes, because they are often, in fact, peripheral (labyrinthine) lesions. This is because the blood supply to the inner ear usually derives from the AICA, often leading to combined posterior fossa and labyrinthine infarctions that impair the VOR through direct ischemia to the inner ear.10 Together, PICA and AICA strokes account for 95% of strokes causing acute vestibular syndrome, and PICA strokes outnumber AICA strokes nearly 5:1.6 A recent modification of the oculomotor approach, H.I.N.T.S. ‘plus’ (Hearing) acknowledges that combined audio-vestibular presentations are more likely to be due to AICA strokes with cochlear or cochlear nucleus infarction than due to benign viral labyrinthitis or ‘cochleo-vestibular’ neuritis.5 Obviously this assumes a normal ear and mastoid examination. When applied in AVS patients, H.I.N.T.S. ‘plus’ has an estimated sensitivity for stroke of 99%.5 For patients with hearing loss and a peripheral-appearing H.I.N.T.S. exam, the presence of direction-changing nystagmus post head shaking may be an additional clue to help segregate central (AICA strokes) from peripheral (labyrinthitis) cases.11
Online Supplement Page 1 of 5 Small strokes causing acute vestibular syndrome Saber Tehrani, et al.
Figure adapted from Newman-Toker et al., Academic Emergency Medicine 20135 Figure e-1. One possible diagnostic workup strategy in acute vestibular syndrome based on HINTS ‘plus’
Those with non-isolated acute vestibular syndrome (AVS) have obvious focal neurologic signs and are treated as with any other acute stroke (e.g., thrombolysis if within the appropriate time window and without evidence of intracranial hemorrhage; appropriate conservative treatments if outside the window for thrombolysis). Among those with isolated AVS, the approach identifies probable strokes using HINTS ‘plus’ findings (I.N.F.A.R.C.T. or new hearing loss, Table S1). These patients are assessed by MRI if >48-72 hours (after which time MRI sensitivity rises to its maximum).12 If <48 hours, then it may be appropriate to delay MRI (e.g., if the stroke etiology is known to be non-threatening and the patient is clinically stable); delaying reduces the need for duplicative MRIs. Obviously in cases of suspected evolving vertebrobasilar occlusion or dissection it may be necessary to obtain MRI and vascular neuroimaging (e.g., by CT angiography or MR angiography) more urgently. Isolated AVS patients with benign HINTS ‘plus’ findings should be diagnosed at the bedside as vestibular neuritis, without neuroimaging, and then be treated appropriately (e.g., meclizine +/- steroids; fluid repletion or anti-emetics for severe vomiting; early vestibular rehabilitation referral). HINTS ‘plus’ and related clinical findings that suggest neuritis (i.e., an acute peripheral vestibulopathy) in AVS can be remembered using an adaptation of a recently published13 mnemonic:
‘S.E.N.D. H.I.M. O.N. H.O.M.E. S.A.F.E.’―Straight Eyes [no skew deviation]; No Deafness [no new hearing loss, either side]; Head Impulse Misses [unilaterally abnormal horizontal VOR on the side opposite the nystagmus fast phase]; One-way Nystagmus [predominantly horizontal, direction-fixed in all gaze positions]; Healthy Otic and Mastoid Exam [pearly tympanic membranes; no pimples, pus, perforation, or pain on palpation of the mastoid]; Stands Alone [stands without holding on to another person or object]; Face Even [no facial palsy or weakness]).
Online Supplement Page 2 of 5 Small strokes causing acute vestibular syndrome Saber Tehrani, et al.
URLs for Bedside Eye Movement Videos Demonstrating Clinical Findings for HINTS Testing
Head Impulse (test of vestibulo-ocular reflex [VOR] function)
• Abnormal result in peripheral vestibulopathy due to vestibular neuritis http://stroke.ahajournals.org/content/vol0/issue2009/images/data/STROKEAHA.109.551234/DC1/Kattah_ Video1a_APV_HITabnormal.wmv
• Normal result in central vestibulopathy due to stroke http://stroke.ahajournals.org/content/vol0/issue2009/images/data/STROKEAHA.109.551234/DC1/Kattah_ Video1b_PICAStroke_HITnormal.wmv
Nystagmus Type (primary/lateral gaze testing for unidirectional vs. bidirectional with gaze-evoked change)
• Direction-fixed nystagmus in peripheral vestibulopathy http://content.lib.utah.edu/u?/ehsl-dent,1
• Direction-changing nystagmus (with gaze-evoked component) in central vestibulopathy due to stroke http://content.lib.utah.edu/u?/ehsl-dent,2
Skew (alternate cover test for vertical ocular misalignment)
• Skew deviation in central vestibulopathy due to stroke http://stroke.ahajournals.org/content/vol0/issue2009/images/data/STROKEAHA.109.551234/DC1/Kattah_ Video3_LatMedullaStroke_SkewAltCover.wmv
Acute vestibular syndrome videos listed above were published in association with the two manuscripts below:
• Newman-Toker DE, Kattah JC, Alvernia JE, Wang DZ. Normal head impulse test differentiates acute cerebellar strokes from vestibular neuritis. Neurology 2008;70:2378-85. www.neurology.org/cgi/content/full/70/24_Part_2/2378/DC1
• Kattah JC, Talkad AV, Wang DZ, Hsieh YH, Newman-Toker DE. H.I.N.T.S. to diagnose stroke in the acute vestibular syndrome: three-step bedside oculomotor exam more sensitive than early MRI diffusion-weighted imaging. Stroke 2009 Nov;40(11):3504-10. http://stroke.ahajournals.org/cgi/content/full/STROKEAHA.109.551234/DC1
Additional Related Resources may be found at the following links…
Neuro-Ophthalmology Virtual Education Library (NOVEL) http://library.med.utah.edu/NOVEL/Newman-Toker/ Select “Collection” link then “A. Ocular and neurologic examinations.”
Medscape.com A description of the HINTS exam with videos of abnormal findings narrated by Dr. Newman-Toker is available at: www.medscape.com/viewarticle/710698
Washington University Emergency Medicine Podcast A podcast describing the HINTS exam by Dr. Newman-Toker can be found at:
Online Supplement Page 3 of 5 Small strokes causing acute vestibular syndrome Saber Tehrani, et al. https://drive.google.com/file/d/0B30p1vt4O1H3NkVraUw3RUtNMHM/edit?usp=sharing
Online Supplement Page 4 of 5 Small strokes causing acute vestibular syndrome Saber Tehrani, et al.
References
1. Newman-Toker DE, Saber Tehrani AS, Mantokoudis G, Pula JH, Guede CI, Kerber KA, Blitz A, Ying SH, Hsieh YH, Rothman RE, Hanley DF, Zee DS, Kattah JC. Quantitative video-oculography to help diagnose stroke in acute vertigo and dizziness: toward an ECG for the eyes. Stroke. 2013;44(4):1158-61. 2. Kattah JC, Talkad AV, Wang DZ, Hsieh YH, Newman-Toker DE. HINTS to diagnose stroke in the acute vestibular syndrome: three-step bedside oculomotor examination more sensitive than early MRI diffusion-weighted imaging. Stroke. 2009;40(11):3504-10. 3. Halmagyi GM, Aw ST, Cremer PD, Curthoys IS, Todd MJ. Impulsive testing of individual semicircular canal function. Ann N Y Acad Sci. 2001;942:192-200. 4. Newman-Toker DE, Kattah JC, Alvernia JE, Wang DZ. Normal head impulse test differentiates acute cerebellar strokes from vestibular neuritis. Neurology. 2008;70(24 Pt 2):2378-85. 5. Newman-Toker DE, Kerber KA, Hsieh YH, Pula JH, Omron R, Saber Tehrani AS, Mantokoudis G, Hanley DF, Zee DS, Kattah JC. HINTS Outperforms ABCD2 to Screen for Stroke in Acute Continuous Vertigo and Dizziness. Acad Emerg Med. 2013;20(10):986-96. 6. Tarnutzer AA, Berkowitz AL, Robinson KA, Hsieh YH, Newman-Toker DE. Does my dizzy patient have a stroke? A systematic review of bedside diagnosis in acute vestibular syndrome. CMAJ. 2011;183(9):E571-92. 7. Leigh RJ, Zee DS. The neurology of eye movements (4th edition). New York: Oxford University Press; 2006. 8. Brodsky MC, Donahue SP, Vaphiades M, Brandt T. Skew deviation revisited. Surv Ophthalmol. 2006;51(2):105-28. 9. Guyatt GH, Oxman AD, Kunz R, Falck-Ytter Y, Vist GE, Liberati A, Schunemann HJ. Going from evidence to recommendations. BMJ. 2008;336(7652):1049-51. 10. Lee H. Audiovestibular loss in anterior inferior cerebellar artery territory infarction: a window to early detection? J Neurol Sci. 2012;313(1-2):153-9. 11. Huh YE, Koo JW, Lee H, Kim JS. Head-Shaking Aids in the Diagnosis of Acute Audiovestibular Loss due to Anterior Inferior Cerebellar Artery Infarction. Audiol Neuro-otol. 2013;18(2):114-24. 12. Schwamm LH, Koroshetz WJ, Sorensen AG, Wang B, Copen WA, Budzik R, Rordorf G, Buonanno FS, Schaefer PW, Gonzalez RG. Time course of lesion development in patients with acute stroke: serial diffusion- and hemodynamic-weighted magnetic resonance imaging. Stroke. 1998;29(11):2268-76. 13. Newman-Toker DE. Symptoms and signs of neuro-otologic disorders. Continuum (Minneap Minn). 2012;18(5 Neuro-otology):1016-40.
Online Supplement Page 5 of 5