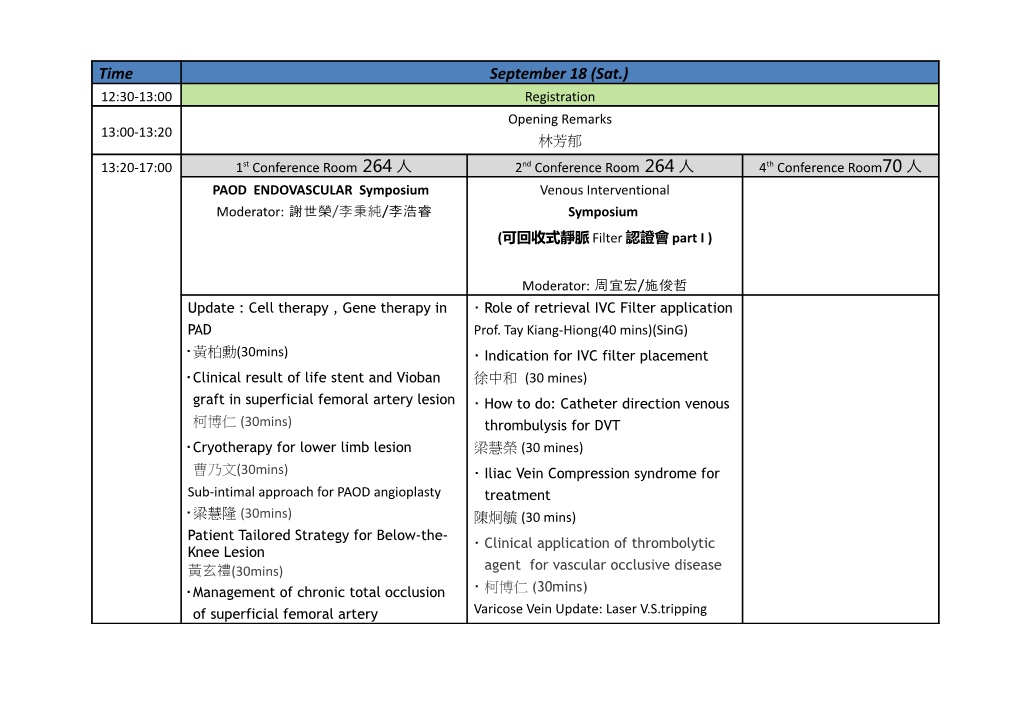
Time September 18 (Sat.) 12:30-13:00 Registration Opening Remarks 13:00-13:20 林芳郁 13:20-17:00 1st Conference Room 264 人 2nd Conference Room 264 人 4th Conference Room70 人 PAOD ENDOVASCULAR Symposium Venous Interventional Moderator: 謝世榮/李秉純/李浩睿 Symposium (可回收式靜脈 Filter 認證會 part I )
Moderator: 周宜宏/施俊哲 Update : Cell therapy , Gene therapy in Role of retrieval IVC Filter application PAD Prof. Tay Kiang-Hiong(40 mins)(SinG) 黃柏勳(30mins) Indication for IVC filter placement Clinical result of life stent and Vioban 徐中和 (30 mines) graft in superficial femoral artery lesion How to do: Catheter direction venous 柯博仁 (30mins) thrombulysis for DVT Cryotherapy for lower limb lesion 梁慧榮 (30 mines) 曹乃文(30mins) Iliac Vein Compression syndrome for Sub-intimal approach for PAOD angioplasty treatment 梁慧隆 (30mins) 陳炯毓 (30 mins) Patient Tailored Strategy for Below-the- Clinical application of thrombolytic Knee Lesion 黃玄禮(30mins) agent for vascular occlusive disease Management of chronic total occlusion 柯博仁 (30mins) of superficial femoral artery Varicose Vein Update: Laser V.S.tripping 林佳勳(30mins) 袁明琦(30mins) Discussion (10 mins)
14:40-15:00 Coffee Break 17:00-18:00 To 僑園 Speech /Dinner Symposium Moderator: 施俊哲/邱肇基 司儀:袁明琦 高秋惠 18:00-19:00 More weapons,better control? 蔡世澤 (30mins) Lower, Sooner, and Cheaper: Can We Have Them ALL?江晨恩 (30mins) 19:00-21:00 樂團表演+Gala Dinner
September 19 (Sun.) Time 1st Conference Room 2nd Conference Room 4th Conference Room 08:00- Moderator:周財福/李國禎/顏旭霆 09:00 會員 Recorded Case Presentation 6 個 Special Lecture Moderator:蔡宗博/楊友任 09:00- Speaker:邀請中 09:30 TEVAR Word Current Trend and management of challenge anatomy 09:30- Moderator: 陳復銓/蔡建松 10:00 Speaker: 邀請中 Current update and future September 19 (Sun.) Time 1st Conference Room 2nd Conference Room 4th Conference Room perspectives of aortic endografting 10:00- Coffee Break 10:10 Moderator: 柯博仁/李芳艷 10:00- The role of Viabahn in the 10:30 management of PAD Speaker: Peter H. Lin, MD(USA) Moderator:林萍章/張忠毅 TEVAR 術後的併 發症(30mins) 10:30- Speaker 符偉國(上海) 11:00 智深獎 優秀論文首 獎 者報告(30mins)
11:30- 九十九年度第三屆第二次會員大會 2010 Annual Meeting(1st Conference Room ) 12:30 12:30- EVAR Workshop 13:30 Lunch Symposium (主動脈支架血管認證會)
Lunch Symposium Moderator:翁仁崇/鄭伯智 Moderator: 謝宏昌/林佳勳 Moderator: 施俊哲/呂明仁 13:10 ~ 13:40 What is Endovascular Grafts Update of Carotid Stenting(30mins) Direct Renin Inhibitors in Isolated 施俊哲 Systolic Hypertension(30mins) Speaker:高憲立 13:40 ~ 14:10 Sizing and Speaker:陳震寰 CAS vs CEA from Surgeon’s Planning of Endovascular September 19 (Sun.) Time 1st Conference Room 2nd Conference Room 4th Conference Room view(30mins) Expanding Indications Of Statin Use In Aortic Aneurysms Repair Speaker:崔源生 Clinical Practice(30mins) 柯博仁 Speaker:陳隆景
Moderator:陳懷民/趙家聲/謝炯昭 Moderator:王志軒/張效煌 14:10 ~ 14:40 Essential Preparing & Setting for Endovascular Aneurysmal 13:30- Repair 14:50 會員 Recorded Case Presentation 顏旭霆 會員 Recorded Case Presentation 邀醫院為 主,會員演講 8 個(10mins) 邀醫院為 主,會員演講 8 個(10mins) 15:00 ~ 15:30 Device Description 吳毅暉 14:50- Coffee Break 15:20 Invited Speech 15:30 ~ 16:00 Patient Moderator:張燕/魏崢/謝敏暲 Selection 海峽兩岸論壇 林佳勳 主動脈瘤治療現況 15:20- 符偉國(上海) (30mins) 16:00 ~ 16:30 Hands On 16:50 許喬博 陳沂名 常 謙(北京) (30mins) / 鄭永強(香港) (30mins) 16:30 ~ 16:50 Q&A 施俊哲(台北) (30mins) 16:50- 頒獎&抽獎 (司儀:袁明琦 高秋惠) September 19 (Sun.) Time 1st Conference Room 2nd Conference Room 4th Conference Room 17:50
Peter H. Lin, MD Professor and Chief Division of Vascular Surgery & Endovascular Therapy Michael E. DeBakey Department of Surgery Baylor College of Medicine
符偉國
職 稱:主任醫師|教 授|博士生導師 供職機構:上海復旦大學附屬中山醫院 畢業院校:上海醫科大學 單位類別:臨床醫院 所屬科室:血管外科 職 務:主任|研 究所副所長 研究領域:血管外科方面的醫、教 、 研 工作 符偉國, 1962 生,上海市人,醫學博士、教 授、博士生導師。1985 年,上海醫科大學醫學系醫學專業畢業,獲學 士學位;1991 年,上海醫科大學研 究生院畢業,獲博士學位;現任復旦大學附屬中山醫院血管外科主任,復旦 大學血管外科研 究所副主任,中華外科分會血管外科學組委員,上海普外科學會委員,中華外科雜誌編委,中國 實用外科雜誌編委,外科理論與實踐雜誌編委,中國普通外科雜誌編委,中國內鏡雜誌編委,介入放射學雜誌編 委,亞洲血管學會委員,國際腔內血管外科學會委員。 主要從事血管外科的醫、教 、 研 工作 承擔各類課題共 8 項國家 863 攻關課題 1 項,國家自然基金 2 項、教 育部 1 項、衛生部 1 項、上海市科委課題 1 項 和上海
Name: Kao, Hsien-Li, Paul 高憲立
Date of Birth: 6 November 1964
Address: Office: Department of Internal Medicine National Taiwan University Hospital No. 7, Chung-Shan South Road, Taipei, Taiwan, R.O.C. Home: 9th Floor, No. 40, Lane 313, Fu-Shing North Road, Taipei, Taiwan E-mail: [email protected]
Education and Training: 1983-1990 National Taiwan University Medical College 1991-1994 National Taiwan University Hospital, Department of Internal Medicine, Residency 1994.1996 National Taiwan University Hospital, Cardiovascular Division, Fellowship
Experience: 1997-1999 National Taiwan University Hospital, Coronary Intensive Care Unit, Attending Physician 1998-2003 National Taiwan University Medical College, Clinical Lecturer in Medicine (Cardiology) 2002.2006National Taiwan University Hospital, Cardiac Cath Lab, Director 2002-2006 Executive Board, Society of Atherosclerosis and Vascular Disease, Taiwan 2003-2006 Advisory Board, Taiwan Society of Cardiovascular Intervention 2003-2010 National Taiwan University Medical College, Assistant Professor in Medicine (Cardiology)
Current appointment: National Taiwan University Hospital, Cardiovascular Division, Staff Interventionist (1996-) Interventional Committee, Society of Cardiology, Taiwan (2003-) Executive Board, Taiwan Society of Cardiovascular Intervention (2006-) Board of Founder Governor, Asian Interventional Cardiovascular Therapeutics (2006-) Fellow, Asian Pacific Society of Interventional Cardiology (2006-) Director, Cardiovascular center, National Taiwan University Hospital Yun-Lin Branch (2008-) Member, International Advisory Council, CRF (2008-) Member, CCRF (2009-) National Taiwan University Medical College, Associate Professor in Medicine (Cardiology) (2010-)
Licensing: 1990 Board of Physician 1994 Board of Internal Medicine 1995 Board of Cardiology 1995 Board of Emergency Medicine and Intensive Care
Membership: Society of Internal Medicine, Taiwan Society of Cardiology, Taiwan Society of Emergency Medicine and Intensive Care, Taiwan Society of Atherosclerosis and Vascular Disease, Taiwan Society of Cardiovascular Disease Prevention and Control, Taiwan Society of Intensive Care, Taiwan Taiwan Society of Cardiovascular Intervention Asian Pacific Society of Interventional Cardiology
Major fields of interest: General cardiology Intensive cardiac care Invasive cardiology Transcatheter endovascular intervention 崔源生醫師 主治專長 1.腦部創傷 2.脊椎手術 3.坐骨神經痛 4.腦部腫瘤 5.頸動脈支架術 6.腦血管內栓塞治療 專業經驗 台中榮民總醫院神經外科主治醫師 重要經歷/進修訓練 1.台北榮民總醫院神經外科專科醫師訓練 2.竹東榮民醫院神經外科主治醫師 3.日本國立東北大學腦血管治療科臨床研 究 學歷 國防醫學院醫學士 專科證照 1.外科專科醫師 2.神經外科專科醫師 3.重症專科醫師
Name: Stephen Wing Keung CHENG 鄭永強
Date of birth: May 9, 1960
Place of birth: Hong Kong
Marital status: Married, one child Current appointment: Professor Department of Surgery, The University of Hong Kong Honorary Consultant, Queen Mary Hospital Chief, Division of Vascular Surgery
Address: Department of Surgery, The University of Hong Kong. 2/F Professorial Block, Queen Mary Hospital, Pokfulam Road, Hong Kong (852) 2855 4962
QUALIFICATIONS
1984 M.B., B.S. The University of Hong Kong 1989 F.R.C.S. The Royal College of Surgeons of Edinburgh 1993 M.S. The University of Hong Kong 1993 F.H.K.A.M. The Hong Kong Academy of Medicine 1995 F.A.C.S. American College of Surgeons 2000 F.R.C.S. (ad eundem) The Royal College of Surgeons of England
EDUCATION
1972 - 1979 St. Paul's Co-educational College, Hong Kong 1979 - 1984 The University of Hong Kong, Hong Kong Undergraduate scholarships:
1979 - 1983 Digby Memorial Scholarship 1979 - 1984 Li Po Chun Scholarship 1981 - 1984 Li Shu Fan Medical Foundation Clinical Scholarship 1981 - 1984 Wong Ching Yee Medical Scholarship Undergraduate prizes:
1981 Ho Fook Prize for the highest place in the first and second MBBS examinations
1981 Li Shu Fan Medical Foundation Prize in Physiology
Distinctions: Distinctions in Anatomy, Physiology, and Obstetrics and Gynaecology
CERTIFICATIONS AND LICENCES
1985 Full registration The Medical Council of Hong Kong (M5756)
1985 ECFMG Educational Commission for Foreign Medical Certification Graduates, USA.
1990 Principal list General Medical Council, United Kingdom
1985 Member The Medical Defence Union (189280C/07)
1993 Member The Medical Protection Society (HK6239)
1998 Specialist registration The Medical Council of Hong Kong (S28-0021)
1998 Specialist registration General Medical Council, United Kingdom (Surgery) APPOINTMENT HISTORY
7/1985 - 8/1990 Medical Officer Department of Surgery The University of Hong Kong
9/1990 - 6/1994 Lecturer Department of Surgery The University of Hong Kong
9/1991 - 8/1992 Visiting assistantDepartment of Surgery professor University of California, San Francisco
7/1994 - 5/1996 Senior Lecturer Department of Surgery The University of Hong Kong
7/1994 - presentHonorary Consultant Department of Surgery Queen Mary Hospital
6/1996 - 6/1999 Associate Professor Department of Surgery The University of Hong Kong
7/1999 - present Professor Department of Surgery The University of Hong Kong 3/1999 - 2/2000 Honorary Consultant Department of Surgery Vascular SurgeryTung Wah Hospital
3/2000 - present Honarary Senior Department of Surgery Consultant in Tung Wah Hospital Vascular Surgery
MEMBERSHIP IN PROFESSIONAL ORGANIZATIONS
1989 Fellow The Royal College of Surgeons of Edinburgh
1989 Member Societe Internationale de Chirurgie (Till 2003)
1989 Member Asian Surgical Association
1988 Fellow Hong Kong Surgical Society
1989 Founding member Hong Kong Medical Laser Association
1990 Foundation fellow The College of Surgeons of Hong Kong
1993 Foundation fellow The Academy of Medicine of Hong Kong 1995 Fellow American College of Surgeons
1996 Executive board Chinese Society of Vascular Surgery
1998 National delegate International Union of Angiology (Till 2002)
1999 Consultant Quangzhou Society of Vascular Surgery
2001 Member European Society for Vascular Surgery
2002 Advisory board 5th Congress of the Asian Vascular Society
2002 Council memberAsian Vascular Society
2002 Member Society for Vascular Surgery (SVS)
2003 Advisory board International Union of Angiology
2003 Member Western Vascular Society (WVS)
2003 Distinguished FellowSociety for Vascular Surgery (SVS)
2003 Board of Governors American College of Surgeons
EDITORIAL POSTS
1996 Editorial Board Chinese Journal of Vascular Surgery
2002 Editor Annals of the College of Surgeons of Hong Kong 2002 Co Editor-in-Chief Asian Journal of Surgery
2002 Editorial Board Cutting Edge, The College of Surgeons of HK Newsletter
2003 Editor in Chief Asian Journal of Surgery
Services / Administration
UNIVERSITY SERVICE
1992 Board of examiners, Final MBBS examination
1994 Board of examiners, BSc (Nurs. Stud.)
1995 Workgroup on Faculty MBBS New Curriculum Development
1995 Faculty computer committee
1996 Board of internal examiners, BDS third examination
1997 Undergraduate Committee Foundation Course Group
1999 Chairman, Committee on Madam SH Ho Residence for Medical Students (-01)
1999 Chairman, MBBS III (Phase I) New Curriculum Planning Group
2000 Undergraduate Education Committee 2001 Committee on Research and Conference Grants Research Panel for Medicine
2002 Chairman, MBBS III Coordinating Sub-Committee of the Undergraduate Education Committee
DEPARTMENT
1989 Director, Vascular Laboratory
1992 Director, Surgery Residency Training Program
1993 Chief, Division of Vascular Surgery, Department of Surgery
1996 Department Committee on Clinical Services
1996 American College of Surgeons, Hong Kong Chapter, Committee on Trauma
1996 Course Director, Instructor Course for ATLS Program
1996 Instructor, InterCollegiate Basic and Advanced Surgical Skills Course
1996 Chairman, Department Staff and Personnel Committee
1996 Strategic Planning Group, Department of Surgery
1996 Coordinator for Hospital Authority PRG Group - Diabetic Foot
1996 Director, The Francis Tien Vascular Disease Center
1997 Director, The Hong Kong Surgical Forum 1998 Working Group on the Review of Non-cardiac Vascular Diagnostic and Interventional procedures, Queen Mary Hospital 2002 Member, Queen Mary Hospital Adult ICU Management Committee
EXTERNAL
1995 Training Sub-committee (Surgery), Co-ordinating Committee in Surgery
1996 Externship subcommittee, The Licentiate Committee, Medical Council of Hong Kong
1996 Royal Australasian College of Surgeons, Board of General Surgery, Hong Kong Regional Subcommittee
1998 Accreditation Committee, Hong Kong Intercollegiate Board of Surgical Colleges
1998 Training Subcommittee, College of Surgeons of Hong Kong, General Surgery Board
1999 Ad Hoc Committee on Carotid Endovascular Stenting in the Management of Extracranial Carotid Artery Stenosis, Hong Kong Academy of Medicine.
1999 Hospital Authority Working Group in Vascular Surgery, member, Chairman
2000 Hospital Authority Commission on Stroke Service, member 2000 Hospital Authority e-Knowledge Gateway Surgery Editorial Panel (Honorary member)
2000 Examination subcommittee, The Licentiate Committee, Medical Council of Hong Kong
2001 Hospital Authority Expert Panel in Surgery
2002 Member of Scientific Committee, College of Surgeons of Hong Kong
2002 Member of Research Support Unit, College of Surgeons of Hong Kong
2002 Hospital Authority Specialty Group in General Surgery
2002 Program Director, Basic Surgical Training, Hong Kong West Cluster
2002 Program Director for Higher Surgical Training Committee, College of Surgeons of Hong Kong
2003 Member, Hospital Authority Central Committee on Surgical Training
EDITORIAL BOARDS
1996 Editorial Board Chinese Journal of Vascular Surgery PROFESSIONAL ORGANIZATIONS
1997 College Tutor, The Royal College of Surgeons of Edinburgh
1998-2002 International Union of Angiology - Administrative Board and National Delegate
2003 International Union of Angiology - Advisory Board
REVIEWER FOR JOURNALS
1992 European Journal of Vascular Surgery
1993-99 Asian Journal of Surgery
1996 Chinese Journal of Vascular Surgery
1997-99 Annals of the College of Surgeons of Hong Kong
1999 Cardiologia - Peripheral Vascular Diseases Section reviewer
2000 The British Journal of Surgery
2001 Asian Cardiovascular and Thoracic Annals
2002-3 Circulation 2002 Ethnicity and Disease
EXTERNAL EXAMINERSHIP
2001 External Examiner in Surgery, Final Professional M.B.,B.S. Examination
The National University of Singapore, March 19-23, 2001.
ADVISORY BOARDS
2002 Council Member, Asian Vascular Society
2002 Advisory Board Member, 5th International Congress, Asian Vascular Society, Singapore, May 23-26
2002 Vice-President, 4th International Congress on Vascular and Endovascular Surgery, Beijing, China October
17-20
OTHERS
2002 Reviewer for appointment of associate professor, NUS Singapore (Dr. Alex Chao).
2003 The University of Hong Kong Sau Po Center on Aging - Fellow 陳震寰 出生日期: 1957年11月25日 畢業學校: 國立陽明大學醫學院醫學系 重要經歷: 住院醫師: 1984年7月至1988年6月 台北榮民總醫院內科部 住院總醫師 1988年7月至1989年6月 台北榮民總醫院內科部 臨床研 究員 1989年7月至1989年12月 台北榮民總醫院內科部心臟科 主治醫師 1989年1月至2005年10月 台北榮民總醫院內科部心臟科 主治醫師 2005年11月迄今 台北榮民總醫院教學 研 究部 教師培育中心主任 2009年8月迄今 台北榮民總醫院教 學 研 究部 醫學系助教 1984年9月至1989年11月 國立陽明大學 醫學系講師 1989年12月至1995年4月 國立陽明大學 醫學系副教 授 1995年5月至2000年7月 國立陽明大學 醫學系教 授 2000年8月迄今 國立陽明大學 社會醫學科科主任 1998年8月至2003年10月 國立陽明大學 醫學系副主任 2000年8月至2003年10月 國立陽明大學 代理醫學系主任 2003年11月至2006年7月 國立陽明大學 醫學系主任 2006年8月迄今 國立陽明大學 研究主題: 心臟超音波 心臟血管流行病學 心臟血管血流動力學 臨床藥物試驗 國外進修: 時間: 1995年7月至1997年6月 地點: 美國約翰霍浦金斯醫院 進修題目: 心臟血管血流動力學
陳隆景 Chen Lung Ching 1968 年 5 月 24 日 112 台北市北投區石牌路二段 201 號台北榮民總醫院重症醫學部 私立中國醫藥學院醫學系學士 1987/ 09 至 1994/06 3、 現職及與專長相關之經歷 服務機關 服務部門/系所 職稱 起訖年月 現職:台北榮民總醫院 重症醫學部/內科部心臟 主治醫師 2002/01~迄今 經歷:法國里耳大學醫學中心 心臟醫院心科導管中心 進修醫師 2001/01~2001/03 台北榮民總醫院 內科部心臟科 資深住院醫師 2000/07~2001/12 台北榮民總醫院 內科部 部總醫師 1999/07~2000/06 台北榮民總醫院 內科部心臟科 科總醫師 1998/07~1999/06 台北榮民總醫院 內科部心臟科 資深住院醫師 1997/07~1998/06 台北榮民總醫院 內科部 住院醫師 1994/07~1997/06 機關 經歷 起訖年月 國立陽明大學 內科學科講師 2002/02~迄今 部定教 職證書字號: 講字第 066086 號 國防醫學院 臨床講師 1997~迄今 中華民國心臟學會 秘書處幹事 2001~2004 中華民國心臟學會 助理編輯 2000~2003 中華醫學雜誌 執行編輯 2005~迄今 臺灣介入性心臟血管醫學會 副秘書長 2007/04~2007/08 臺灣介入性心臟血管醫學會 秘書長 2007/08~2010/1 四、專長
1. 一般心臟內科 2. 冠狀動脈疾病及介入性心臟血管治療 3. 重症醫學 五、專業證照
2007 高級心臟救命術指導員 (ACLS instructor) 2003 重症專科醫師(中重專字第 SC1332 號) 1999 心臟內科專科醫師(中心專 026 號) 1997 內科專科醫師考試及格 1994 專門職業及技術人員檢覈考試醫師類科及格 1994 公務人員高等考試醫療職系公職醫師科及格 六、專科學會
中華民國內科醫學會 中華民國心臟學會 中華民國重症醫學會 中華民國血脂及動脈硬化學會 臺灣介入性心臟血管醫學會
林佳勳醫師
私立台北醫學大學畢業(1984-1991)
長庚醫院見實習醫師 (1989-1991)
長庚醫院第一年外科住院醫師 (1991-1992)
新光醫院第二年外科住院醫師 (1992-1993)
新光醫院第三、四、五年心臟外科住院醫師 (1993-1996)
新光醫院心臟外科主治醫師 (1996-迄今) 美國杜克大學醫學中心心臟外科研 究員
(Duke University Medical Center, 1997)
教育部定輔仁大學醫學院醫學系專任講師 (2005)
輔大醫學系系務代表 (2005,2007)
新光醫院外科加護病房主任 (2005-迄今)
中央健保局醫事審查委員(2005-迄今)
血管外科醫學會教 育委員會委員 (2005-2009)
急救加護醫學會雜誌審稿委員 (2006-迄今)
美國亞歷桑納心臟中心進修(Arizona Heart Institute, Endovascular surgery, 2007)
教育部定輔仁大學醫學院醫學系專任助理 教 授 (2009)
血管外科醫學會常務監事 (2009)
血管外科醫學會臨床委員會主任委員 (2009) 外科醫學會雜誌審稿委員 (2010)
專門職業及技術人員高等考試及格 外科專科醫師 胸腔及心臟血管外科學會專科醫師 胸腔及心臟血管外科學會專科指導醫師 心臟學會心臟血管外科專科醫師 心臟學會心臟血管外科專科指導醫師 重症醫學會專科醫師 重症醫學會專科指導醫師 血管外科學會專科醫師 血管外科學會專科指導醫師 胸腔及心臟血管外科學會主動脈支架操作醫師:
血管外科學會血管腔內手術臨床技術指導醫師 許喬博 醫師
現職
1. 台北榮民總醫院外科部心臟血管外科 主治醫師
學歷 1. 陽明大學 醫學士
經歷
1. 台北榮民總醫院外科部 住院醫師 2. 台北榮民總醫院外科部 住院總醫師
專長
1. 成人心臟血管疾病的外科治療 2. 末期心臟衰竭的外科治療
專科醫師資格
1. 台灣外科醫學會專科醫師 2. 胸腔及心臟血管外科醫學會專科醫師
心臟醫學會專科醫師
施俊哲醫師
現職: 國立陽明大學臨床醫學研 究所 暨 醫學系外科 教授(2007 年 8 月至今) 台北榮民總醫院心臟血管外科 主治醫師(1994 年 7 月至今) 學經歷: 陽明大學臨床醫學博士 台北榮民總醫院外科部 住院醫師 台北榮民總醫院外科部 住院總醫師 台北榮民總醫院外科部 主治醫師 專長: 心臟移植 動脈瘤及主動脈剝離手術 微創人工支假血管治療動脈瘤 心臟瓣膜修補術及心律不整燒灼術 成人心臟血管疾病的外科治療 結合介入與傳統之微創手術治療周邊血管疾病 金屬表面氧化物奈米處理及藥物塗層技術人工血管支架表面材質 研究
黃柏勳醫師 台北榮民總醫院心臟內科主治醫師 專長學科 1. 心臟血管疾病診療,冠狀動脈疾病心導管介入性治療(PTCA, Stenting) 2. 臨床心臟學研究,基礎醫學研究 學歷 陽明大學醫學院醫學士 經歷 台北榮民總醫院內科部住院醫師 台北榮民總醫院內科部心臟科總醫師 台北榮民總醫院內科部心臟科主治醫師 日本東京大學循環器內科客員研究員 專科證書 中華民國內科專科醫師 中華民國心臟專科醫師 專科學會 中華民國內科醫學會 中華民國心臟學會 中華民國動脈硬化及血脂學會
Name: Ko, Po-Jen 柯博仁
Sex: Male
Birth Date: July 23, 1966
Birth Place: ChiaYi, Taiwan
Citizenship: Taiwan
Home Address: 10, Al 14, Ln 16, Sec 1, Chung-Cheng Rd. , Taipei, Taiwan
Tel: 02-28341151
Office Address: Thoracic & Cardiovascular Surgery, Chang Gung Memorial Hospital 5, Fu-Hsing Street, Kuei-Shan Hsiang, Taoyuan Hsien, Taiwan.
Tel: 03-3281200 ext.2118
Chinese Permanent Registration No: Q1212592249
Language: Mandarin, Taiwanese, English
Spouse: Hung, Yen-Ni Birth Date: Jan 11, 1970
Children: Ko, Ji-Ning Birth Date: May 4, 1996
Ko, Ji-Jung Birth Date: Sep 22, 1998
Education:
1985~1992 National Taiwan University, Taipei, Taiwan
Employment Record:
Aug 1994~Jul 1997 R1~R3, Dept of Surgery, Chang Gung Memorial Hospital, Taipei
Aug 1997~Jul 1999 Fellow, Div of Thoracic & Cardiovascular Surgery, CGMH
Aug 1999~Nov 2003 Attending Staff, Section of Cardiovascular Surgery, CGMH
Dec 2003 till now Attending Staff, Section of Vascular Surgery, CGMH
Jul 2005~ present Assistant professor, Div of Thoracic & Cardiovascular Surgery, CGMH Aug 2006~present Assistant professor of Surgery, Chang Gung University
Licensure: Chinese License No: 022438
Board Certification:
1. The Surgical Association of Taiwan, No: 4220
2. Taiwan Society of Cardiology, No: S834
3. Taiwan Association of Thoracic & Cardiovascular Surgery, No: 186
4. Taiwan Society for Vascular Surgery: S00129
Professional Affiliations:
1. The Surgical Association of Taiwan
2. Taiwan Society of Cardiology
3. Taiwan Association of Thoracic & Cardiovascular Surgery
4. International Society for Endovascular Surgery
5. International Society for Vascular Surgery
6. Taiwan Society for Vascular Surgery
Research Interest: Vascular Surgery, Endovascular Treatment for Dialysis Access, Peripheral Artery Disease and Aortic Aneurysm, Tracheobroncheal Stenting 姓名:梁慧隆 性別:男 出生年月日:1959 年 4 月 7 日 學歷:國立陽明大學醫學系 73 年畢業 進修學校:美國加州大學舊金山分校、賓州大學研究 專長:腹部放射線診斷、超音波影像學、介入性放射線學 現職:高雄榮總放射線部介入性治療科主任 國立陽明大學醫學系助理教授
曹乃文 Naiwen Tsao 學歷:國立陽明大學醫學系畢業 經歷:台北榮民總醫院外科部住院醫師、總醫師 桃園榮民醫院心臟血管外科主治醫師 台北醫學大學外科部心臟血管外科主治醫師、科主任 專長: 心臟血管手術 葉克膜體外循環 黃玄禮 經 歷: 林口長庚醫院內科部住院醫師 林口長庚醫院心臟內科總醫師 林口長庚醫院心臟內科主治醫師 林口長庚醫院心臟內科加護病房主治醫師 學 歷:台北醫學大學醫學系
專 長:冠狀動脈心臟病、診斷及介入性心導管、冠狀動脈氣球擴張術及支架放置、血管內超音波、週邊血管及糖尿病足部血管病變氣球擴張術及支架 放置、 廔管超音波檢查及氣球擴張術、支架治療、先天性心房中膈缺損阻隔器置放、心臟超音波、週邊血管超音波、高血壓、心律不整、瓣膜性心臟 病、一般心臟學
林佳勳醫師 私立台北醫學大學畢業(1984-1991) 長庚醫院見實習醫師 (1989-1991) 長庚醫院第一年外科住院醫師 (1991-1992) 新光醫院第二年外科住院醫師 (1992-1993) 新光醫院第三、四、五年心臟外科住院醫師 (1993-1996) 新光醫院心臟外科主治醫師 (1996-迄今) 美國杜克大學醫學中心心臟外科研究員 (Duke University Medical Center, 1997) 教育部定輔仁大學醫學院醫學系專任講師 (2005) 輔大醫學系系務代表 (2005,2007) 新光醫院外科加護病房主任 (2005-迄今) 中央健保局醫事審查委員(2005-迄今) 血管外科醫學會教育委員會委員 (2005-2009) 急救加護醫學會雜誌審稿委員 (2006-迄今) 美國亞歷桑納心臟中心進修(Arizona Heart Institute, Endovascular surgery, 2007) 教育部定輔仁大學醫學院醫學系專任助理教授 (2009) 血管外科醫學會常務監事 (2009) 血管外科醫學會臨床委員會主任委員 (2009) 外科醫學會雜誌審稿委員 (2010) 專門職業及技術人員高等考試及格 外科專科醫師 胸腔及心臟血管外科學會專科醫師 胸腔及心臟血管外科學會專科指導醫師 心臟學會心臟血管外科專科醫師 心臟學會心臟血管外科專科指導醫師 重症醫學會專科醫師 重症醫學會專科指導醫師 血管外科學會專科醫師 血管外科學會專科指導醫師 胸腔及心臟血管外科學會主動脈支架操作醫師: 血管外科學會血管腔內手術臨床技術指導醫師
陳炯毓醫師 PERSONAL:
Business Address: Department of Diagnostic Radiology, Yuan's general hospital No.162, Chenggong 1st Rd., Lingya District, Kaohsiung City 802, Taiwan
Business Telephone: 886-7-3351121 ext-2072
E-mail: [email protected]
Date of Birth: 12/12/1970
Place of Birth: Taiwan
Citizenship: Taiwan
Sex: Male
Martial Status: Married
Number of Children: One
EDUCATION AND QUALIFICATIONS:
Medical School: Taipei Medical University, Taipei, Taiwan Sep 1990-Jun 1997
Military Service: Lieutenant medical officer Oct 1997-May 1999 Residencies: Kaohsiung Veterans General Hospital Sep 1999-Sep 2003
Board Certification: Board of Radiology of ROC Oct 2003 ~
Member of Interventional Radiology of RSROC (IR 883) Nov 2006 ~
Specialist of Vascular Interventional Radiology of RSROC (IRS 003) Nov 2006~
The Lecturer of Department of Education, Taiwan (講字第 087458) Oct 2006~
袁明琦醫師檔案: 現職:台北榮總外科部心臟血管外科主治醫師 學歷: 1.國立陽明大學醫學系畢業 2.英國 University of Nottingham Queen’s Medical Center 臨床研究 3.美國加州大學舊金山分校醫學中心進修 4.美國史丹佛大學醫學中心進修 專長:心臟血管外科、各類型周邊血管疾病 Patient Tailored Strategy for below-the-knee lesions peripheral artery diseaseT Section of Cardiology, Tzu-Chi Buddhist General Hospital, Taipei Branch
Hsuan-Li Huang, MD
The primary goal of endovascular therapy for below-the-knee (BTK) lesions is the re-establishment of pulsatile, straight-line flow to the foot.
These treatments results in relieving ischemic pain, healing of ischemic ulcers, preventing limb loss, improving quality of life and potentially prolong survival. Balloon angioplasty is the currently established therapy, bare-metal stents are reserved for failed percutaneous transluminal angioplasty (PTA). Novel devices such as laser, excisional and rotational atherectomy systems, drug eluting stents or drug coated balloons still lack data demonstrating improved efficacy compared to conventional balloon angioplasty. The typical patient group of complex below-the-knee lesions represents an increasing population due to the increasing prevalence of diabetes and end-stage renal failure. Excellent acute technical success rates above 90%, a low frequency of complications, and high limb salvage rate of about 95% even in patients with long segment and diffuse disease seem to justify a more widespread use of endovascular therapy in tibial arteries. However, the current results of balloon angioplasty studies show a 1-year restenosis rate between 30% for short stenoses treatment and up to 80% following recanalization of an occlusion. In this presentation, we will illustrate different treatment strategy using new devices and techniques for different BTK lesions
Patient Tailored Strategy for below-the-knee lesions peripheral artery disease Section of Cardiology, Tzu-Chi Buddhist General Hospital, Taipei Branch Hsuan-Li Huang, MD The primary goal of endovascular therapy for below-the-knee (BTK) lesions is the re-establishment of pulsatile, straight-line flow to the foot. These treatments results in relieving ischemic pain, healing of ischemic ulcers, preventing limb loss, improving quality of life and potentially prolong survival. Balloon angioplasty is the currently established therapy, bare-metal stents are reserved for failed percutaneous transluminal angioplasty (PTA). Novel devices such as laser, excisional and rotational atherectomy systems, drug eluting stents or drug coated balloons still lack data demonstrating improved efficacy compared to conventional balloon angioplasty. The typical patient group of complex below-the-knee lesions represents an increasing population due to the increasing prevalence of diabetes and end-stage renal failure. Excellent acute technical success rates above 90%, a low frequency of complications, and high limb salvage rate of about 95% even in patients with long segment and diffuse disease seem to justify a more widespread use of endovascular therapy in tibial arteries. However, the current results of balloon angioplasty studies show a 1-year restenosis rate between 30% for short stenoses treatment and up to 80% following recanalization of an occlusion. In this presentation, we will illustrate different treatment strategy using new devices and techniques for different BTK lesions
Management of chronic total occlusion of superficial femoral artery Chronic total occlusions in the superficial femoral artery (SFA) are the longest and straightest lesions in the whole body. This presents additional technical challenges and the inability to cross the occluded lesion is a common cause of procedural failure in these percutaneous interventions. The objective of this study was to investigate the usefulness of a strategy using a hydrophilic 1.5 mm J-tip 0.035″ guidewire with an over-the- wire balloon catheter under ultrasound guidance for chronic total occlusions in the SFA. This strategy was performed in 32 consecutive patients (36 limbs). Average occlusion length was 17 ± 10 cm (3–40 cm). The crossover approach was performed in 26 cases (72%); in the remaining 10 cases, the antegrade ipsilateral approach was selected. The technical success rate was 92% (32/36). A secondary popliteal artery approach was performed in the three failed limbs and was successful in two limbs, increasing the final technical success rate to 97%. This novel procedure may be considered the preferred strategy for intervening in chronic total occlusions in the SFA
Cell therapy , Gene therapy in PAD Critical limb ischemia (CLI) continues to form a substantial burden on Western health care. Despite recent advances in surgical and radiological vascular techniques, a large number of patients is not eligible for these revascularisation procedures and faces amputation as their ultimate treatment option. Growth factor therapy and stem cell therapy – both therapies focussing on augmenting postnatal neovascularisation – have raised much interest in the past decade. Based on initial pre-clinical and clinical results, both therapies appear to be promising strategies to augment neovascularisation and to reduce symptoms and possibly prevent amputation in CLI patients. However, the underlying mechanisms of postnatal neovascularisation are still incompletely understood. Both fundamental research as well as large randomised trials are needed for further optimisation of these treatment options, and will hopefully lead to needed advances in the treatment of no-option CLI patients in the near future. Clinical result of life stent and Vioban graft in superficial femoral artery lesion Result of Endovascular stenting in superficial femoral artery Femoropopliteal bypass was the standard treatment for femoral arterial occlusive disease. however, Endovascular treatment has become one of the options for femoral arterial disease in recent years not only for shirt lesions but also for long lesions due to it's less invasiveness. According to the peer reviewed articles, Endovascular treatment for femoral lesions had gained it's roles in clinical practice and achieved comparative outcome to traditional bypass . We had just adopted Endovascular therapy such as stenting and stentgrafting as one of our routine options for the SFA revascularization since 2009. we found that the immediate and midterm outcomes were rather promising. Experience of Cryoplasty in Peripheral Arterial Disease
Naiwen Tsao Department of Cardiovascular Surgery, Taipei Medical University Hospital Background: To evaluate the perioperative and midterm follow-up results of cryoplasty in treating peripheral arterial disease. Method: A retrospective study was carried out in 17 patients and 22 limbs treated by cryoplasty (Polar Cath, Boston Scientific)from October 2007 to May 2009. All limbs were suffered from peripheral arterial disease with the range of ankle-brachial index from 0.2 to 0.63. The perioperative and midterm follow-up results were collected and analyzed. Results: The number of cryoplasty procedures was 19, bilateral revascularizations were performed simultaneously in three patients. Revascularization success rate was 90.9%(20/22). Perioperative mortality was zero. One patient suffered from cerebrovascular accident during hemodialysis on the fisrt postoperative day and one patient received femoral puncture site pseudoaneurysmectomy, the perioperative morbidity was 10.5%(2/19). Follow-up interval periods ranged from 3 to 32 months (mean 17.3 months). The clinical patency rate (freedom from target lesion revascularization or major amputation) was 77.2%. Conclusions: The midterm follow-up data indicate that cryoplasty is a durable therapy for peripheral arterial disease. Key words: Peripheral arterial disease, cryoplasty, femoropopliteal artery
Venous Interventional: DVT symposium
Title: Catheter-directed thrombo-aspiration in management of ilio-femoral deep vein thrombosis. Abstract: There are many ways to manage lower extremity deep vein thrombosis, of them, systemic heparinization is currently the mainstay treatment in Taiwan. The other two options are catheter-directed thrombolysis and surgical/endovascular thrombectomy. The objective of this presentation is to share a vascular interventional radiologist's experiences in dealing with ilio-femoral deep vein thrombosis by using catheter-directed thrombo-aspiration. The content will focus on 1) how I do it 2) for what indications I do it 3) brief discussions on interesting cases and 4) the results.
Title: Clinical application of thrombolytic agent for vascular occlusive diseas Abstract: The use of fibrinolytic agents to control the fibrinolytic enzyme system and lyse pathologic fibrin deposits or thrombus has now assumed a position with anticoagulants and vascular surgery in the physician's therapeutic armamentarium. The principal exogenous activators that are used clinically are streptokinase, urokinase, and tissue plasminogen activator. Acute arterial occlusions are more likely than chronic occlusions to respond to thrombolytic therapy, especially if treatment is instituted within a few hours of onset of symptoms and if the disease is due to embolic material rather than in situ thrombosis. Since the duration of drug infusion necessary to lyse arterial thrombus cannot be predicted, patients in whom tissue viability cannot be determined or in whom ischemia cannot be tolerated during the drug infusion interval are not candidates for intraarterial fibrinolytic drug infusion. In treating patients with venous occlusion, thrombolytic therapy is more effective against proximal clots than in calf thrombosis. No protective effect from pulmonary embolism has been noted in trials comparing heparin with streptokinase. Fifty percent of patients with an initial episode of deep venous thrombosis treated within 72 hours of onset will have complete resolution of thrombus with preservation of valve function.
Title: Varicose Vein Update: Laser V.S tripping Abstract: Sclerotherapy is a treatment using a tiny needle to inject a solution called sclerosant into the veins, irritating the lining of the veins, causing them to close. Sclerotherapy is also used to treat both varicose and spider veins that are seen on the surface of the leg. Problematic larger superficial veins [called varicose veins] are typically “ropey” and visible just below the surface of the skin. Sclerotherapy can help relieve symptoms due to varicose and spider veins. Sclerotherapy of spider and varicose veins is usually done without ultrasound guidance.
Title: The Role of retrieval IVC filter application
Prof. Tay Kiang-Hiong, Director, Interventional Radiology Centre, Singapore General Hospital
Abstract: Evidence-based guidelines from the American College of Chest Physicians and Society of Interventional Radiology recommend inferior vena cava (IVC) filter placement in patients with proven venous thromboembolism with a failure of, a contraindication to, or a complication secondary to anticoagulation. Before 2003, vena cava filters available in the United States were permanent implants. Removable vena cava filters for temporary protection from pulmonary embolism was first proposed in 1967. Currently available vena cava filters in the United States include devices intended as permanent implants and devices with an option of removal at a later date. In the latter case, such devices have approval as permanent implants, with the option for removal at some point in the future care of the patient. The classic example of the clinical use of an optional filter is that of a young trauma patient with multiple injuries, including long-bone fractures and head trauma, which could not receive anticoagulation and would be at significant risk for potential life-threatening venous thromboembolic events. The use of an optional vena cava filter in this setting would be a reasonable choice. Our objectives are to evaluate the effectiveness of retrieval IVC filter to prevention pulmonary embolism. Venous Interventional: DVT symposium Title: Indication for IVC filter placement
Abstract: Pulmonary embolism (PE) continues to be a major cause of morbidity and mortality in the United States. Estimates of the incidence of nonfatal PE range from 400,000 to 630,000 cases per year, and 50,000-200,000 fatalities per year are directly attributable to PE. The current preferred treatment for deep venous thrombosis (DVT) and PE is anticoagulation. However, up to 20% of these patients will have recurrent PE. Interruption of the inferior vena cava (IVC) for the prevention of PE was first performed in 1893 using surgical ligation. Over the years, surgical interruption took many forms (ligation, plication, clipping, or stapling), but IVC thrombosis was a frequent complication after these procedures. Endovascular approaches to IVC interruption became a reality in 1967 after the introduction of the Mobin-Uddin filter.
This guideline was revised by a collaborative panel of the American College of Radiology and the Standards of Practice Committee of the Society of Interventional Radiology (SIR) as following: A. Accepted 1. Patients with evidence of pulmonary embolus or IVC, iliac, or femoral-popliteal DVT and one or more of the following: a. Contraindication to anticoagulation. b. Complication of anticoagulation. c. Failure of anticoagulation. i. Recurrent PE despite adequate therapy. ii. Inability to achieve adequate anticoagulation.
2. Massive pulmonary embolism with residual deep venous thrombus in a patient at risk for further PE. 3. Free floating iliofemoral or inferior vena cava thrombus. 4. Severe cardiopulmonary disease and deep-vein thrombosis (DVT) (e.g., cor pulmonale with pulmonary hypertension). 5. Poor compliance with anticoagulant medications.
B. Additional Indications for Selected Patients 1. Severe trauma without documented PE or DVT. a. Closed head injury. b. Spinal cord injury. c. Multiple longbone or pelvic fractures 2. High-risk patients (e.g., immobilized, ICU patients, prophylactic preoperative placement in patients with multiple risk factors for venous thromboembolism).
C. Suprarenal Filter Placement 1. Renal vein thrombosis. 2. IVC thrombosis extending above the renal veins. 3. Filter placement during pregnancy. Suprarenal placement is also appropriate in women of childbearing age. 4. Thrombus extending above previously placed infrarenal filter. 5. Pulmonary embolism following gonadal vein thrombosis. 6. Anatomic variants: duplicated IVC, low insertion of renal veins. Title: Catheter-directed thrombolysis in treatment of vessels thrombosis.
Abstract: The incidence of deep venous thrombosis (DVT) is highly dependent on the population and on the definition of DVT used. Two main complications of DVT are pulmonary embolism and post-thrombotic syndrome (PTS), and the incidence of PTS is higher in patients that only receive anticoagulation for the management of DVT. Most physicians consider that the delivery of a thrombolytic agent into a thrombus is more effective than systemic anticoagulation because this procedure reduces the complication rate of systemic anticoagulation. Contemporary venous thrombectomy has been reported to Two main complications of DVT are pulmonary embolism and post-thrombotic syndrome (PTS), and the incidence of PTS is higher in patients that only receive anticoagulation for the management of DVT. Most physicians consider that the delivery of a thrombolytic agent into a thrombus is more effective than systemic anticoagulation because this procedure reduces the complication rate of systemic anticoagulation. Contemporary venous thrombectomy has been reported to improve early and long term results in extensive iliofemoral DVT as compared with simple catheter-directed thrombolysis.
Our objectives are to evaluate the effectiveness of catheter-direction thrombolysis in treatment of vessel thrombusis patients.
TEVAR Word Current Trend and management of challenge anatomy Thoracic endovascular aortic repair (TEVAR) refers to the percutaneous placement of a stent graft in the descending thoracic or thoracoabdominal aorta to improve long- term survival in patients with aortic aneurysms. The complications of elective thoracic aneurysm repair using an open surgical (OS) technique are higher than most elective surgical procedures, given anatomic constraints and operative complexity. TEVAR was initially developed to treat patients who were considered to not be surgical candidates but is now considered a suitable alternative to OS in most cases.
Potential benefits of TEVAR relative to OS include avoidance of long incisions in the thorax or abdomen, no cross-clamping of the aorta, less blood loss, lower incidence of visceral, renal, and spinal chord ischemia (SCI), fewer episodes of respiratory dependency, and quicker recovery.
The pivotal trials of TEVAR for treatment of thoracic aortic aneurysm led to its approval by the United States Food and Drug Administration in 2005. TEVAR has been increasingly used for other aortic pathologies such as complicated type B dissection, traumatic aortic transection, and aneurysmal disease extending into the arch. Each will be mentioned in brief, but this topic will principally address the endovascular treatment of thoracic aneurysms.
Current update and future perspectives of aortic endografting
BACKGROUND: Surgical repair of thoracoabdominal aortic aneurysms remains a technically challenging operation that requires a multimodality approach to preventing ischemic complications. The purpose of this report is to update our experience and highlight our current clinical strategies.
METHODS: Between January 1, 1986 and December 31, 2001, 1,773 patients underwent thoracoabdominal aortic aneurysm repair. The majority of these patients (1,153, 65%) required Crawford extent I or II repairs. Segmental intercostal or lumbar arteries were reattached in 1,082 patients (61%); left heart bypass was used in 686 patients (38.7%), and 173 patients (9.8%) had cerebrospinal fluid drainage. RESULTS: The 30-day survival rate was 94.3% (1,672 patients). Postoperative complications included renal failure requiring hemodialysis in 105 patients (5.9%) and paraplegia or paraparesis in 79 patients (4.5%). Actuarial 5-year survival was 73.5% ± 1.6%.
CONCLUSIONS: This clinical experience demonstrates that current technical strategies enable patients to undergo thoracoabdominal aortic aneurysm repair with excellent early survival and acceptable morbidity.
Although results after the surgical repair of thoracoabdominal aortic aneurysms (TAAAs) continue to improve, patients remain susceptible to postoperative renal and neurologic complications, often culminating in death. Prevention of these complications requires a multimodality approach. The purpose of this report is to update our experience and highlight our current clinical strategies.
The role of Viabahn in the management of PAD The stratifications of aortoiliac, femoropopliteal, and infrapopliteal lesions included in the original comprehensive report of the TransAtlantic Inter-Society Consensus (TASC I) have been commonly used to formally characterize clinical trial populations and to channel investigative discussion among clinicians, while the associated treatment recommendations have become outdated as compared to current clinical practice. The TASC II report is an abbreviated update focusing on key areas of diagnosis and management of peripheral artery disease, with revised stratifications of aortoiliac and femoropopliteal lesions but not infrapopliteal disease. The consensus document keeps new lesion stratifications linked to the same structure of recommendations for initial treatment: endovascular for type A, endovascular (with qualifications) for type B, open surgical (with qualifications) for type C, and open surgical for type D. In general, each TASC II lesion category includes more severe disease than in TASC I, but the TASC II report does not recommend specific endovascular modalities for infrainguinal occlusive disease. We discuss how the new TASC II femoropopliteal lesion categories reflect current research outcomes and clinical practice, including summarized results from some more recent studies that have demonstrated the ability to treat by endovascular means increasingly complex femoropopliteal lesions that would actually be classifiable as type C. Noting that TASC II does not include a separate stratification of infrapopliteal lesions, as did TASC I, we review evidence of recent endovascular treatment of infrapopliteal lesions and contend that TASC classifications in this anatomical area should be upgraded.
胸主動脈瘤支架置入術(TEVAR)併發症分析
腹主動脈瘤使用支架型血管進行腔內修復治療的優勢已通過過去 10 年的多個隨機研究得到充分證實。隨著這種治療方法被廣泛地 應用,與之相關的併發症也被逐漸認知。雖然多數與治療相關的併發症可以用腔內的方法進行解決,但是如動脈瘤擴張,移植物感染 或移位元,需要應用傳統的開放手術方法進行治療。 胸主動脈瘤腔內修復術也經歷了類似的發展過程。2005 年,美國 FDA 首次批准使用胸主動脈瘤支架,這種微創治療方法大大改變 了胸主動脈瘤的治療模式,因為這種腔內修復術的風險已被一致認為大大低於傳統開胸手術。由於這種治療方法被廣泛採用,隨之一 些嚴重的併發症將會出現,無論是由於器械問題或其他災難性的不良事件發生時,需要中轉開刀手術治療。在這篇文章中,我們將介 紹腔內治療失敗後中轉外科手術的經驗。 1 臨床資料 2002 年 11 月至 2008 年 8 月,有 253 名胸主動脈瘤病人在 Medicine Daffiliated 醫院接受了胸主動脈腔內修復治療。其中 201 例為胸主 動脈瘤,28 例(11%)為 B 型夾層,7 例(3%)為外傷性胸主動脈損傷,8 例(3%)為潰瘍穿孔或壁間血腫,9 例(4%)為既往行 胸主動脈瘤開刀手術治療後出現吻合口假性動脈瘤而行腔內修復治療。病人通常在術後 6 個月,12 個月及以後每年進行隨訪,行 CT 檢 查,並進行對照。 所有操作均在手術室進行,常規進行全麻。225 例(89%)的病人通過切開暴露股動脈為入路,另外 28 例(11%)則必須通過髂動 脈為入路。25 例(10%)患者需要從肱動脈放置血管造影導管。通過最後的造影證實瘤體被完全修復,技術成功。 7 例降主動脈瘤患者(4.4%)中轉接受外科手術,瘤體修復前需要將支架型血管取出。另外還有 9 例病人是最初在其它醫院接受胸主 動脈廇腔內修復術後,轉我院進行開刀手術治療。這 16 例患者都是在接受腔內修復術失敗後需要外科手術進行補救。 我們把在同一次麻醉期間腔內修復術後立即中轉外科開刀稱為一期中轉,把擇期第二次麻醉進行的中轉開放手術稱為二期中轉。 外科手術時,原來的支架被取出,可以看到主動脈及周圍血管均受到不同程度損傷。所有病例都是通過胸腹聯合切口,應用滌綸人工 血管進行主動脈置換。 2 結果 共 16 名患者行中轉手術,平均年齡為 67 歲(59~79 歲)。其中 2 名患者由於術中出現主動脈夾層逆向撕裂行一期中轉,其餘 14 名個患者行二期中轉。原因包括 1、動脈瘤持續擴張導致 I 型內漏(n=3);2、動脈瘤持續擴張導致支架置入失敗(n=1);3、急性 B 型主動 脈夾層相關的併發症(n=4);4、主動脈夾層及結締組織疾病產成的併發症(n=6)。這些患者住院期間死亡率為 18.8%(3/16)。兩例患者 一期中轉是因為夾層逆向撕裂引起的。其餘 14 例患者二期中轉之間的時間是在 5 天至 43 個月期間(平均 11 個月)。
Update of Carotid Stenting
Carotid artery stenting (CAS) is a non-surgical, catheter-based procedure which unblocks narrowing of the carotid artery lumen to prevent a stroke. Carotid artery stenosis can present with no symptoms (diagnosed incidentally) or with symptoms such as transient ischemic attacks (TIAs) or cerebrovascular accidents (CVAs, strokes). The largest clinical trial to date, CREST, reported no significant differences out to four years of follow-up between surgery and carotid stenting in average risk patients[1]. Younger patients (<70 years old) had better outcomes with stenting than with surgery. Patients had fewer heart attacks with stenting, but they did have more minor strokes. There was no difference between surgery or stenting for major (disabling) strokes.
Several European trials have reported results in symptomatic carotid artery stenosis patients comparing surgery and stenting. The SPACE trial[2], conducted in Germany, Austria, and Switzerland found no difference in outcomes between surgery and stenting. The also noted that younger (< 67 years old) patients had better outcomes with stenting. The noted that more experienced centers had better results than inexperienced centers.
CAS vs CEA from Surgeon’s view
Watertown, MA - Data from a national registry suggest that outcomes at 30 days are better with carotid endarterectomy (CEA) than with carotid artery stenting (CAS) [1]. Investigators report that the combined rate of death, stroke, and MI was significantly lower with the surgical approach vs the less invasive interventional technique.
"The debate about the interpretation of the results of this study as well as results of other CAS studies will continue until randomized trials such as International Carotid Stenting Study (ICSS) in Europe and [the Carotid Revascularization Endarterectomy vs Stenting Trial] CREST in North America are reported," note lead investigator Dr Anton Sidawy (Washington Veterans Affairs Medical Center, DC) and colleagues in the January 2009 issue of the Journal of Vascular Surgery.
The data, from the Society for Vascular Surgery (SVS), are the latest in a number of head-to-head comparisons between CEA and CAS that have often shown conflicting results. Two carotid-artery stenting studies—Stent-Supported Percutaneous Angioplasty of the Carotid Artery versus Endarterectomy (SPACE) [2] and Endarterectomy versus Angioplasty in Patients with Symptomatic Severe Carotid Stenosis (EVA-3S) [3]— were published in 2006, and both showed stenting to be inferior to endarterectomy. Direct Renin Inhibitors in Isolated Systolic Hypertension Chen-Huan Chen, MD
Department of Medical Research and Education Taipei Veterans General Hospital
Isolated systolic hypertension (ISH) is commonly recognized as a wide pulse pressure hypertension and is arbitrarily defined as having systolic blood pressure >140 mmHg and diastolic blood pressure<90 mmHg. Patients with ISH tend to be older and most have advanced cardiovascular disease. However, the phenotype of isolated systolic hypertension is quite heterogeneous. Young adults with ISH are usually characterized as tall males with elevated peripheral blood pressure and normal central aortic pressures, who are active in sports and are nonsmokers. The increased pulse pressure pattern in young patients with ISH may be due to elevated stroke volume with normal peripheral resistance, or normal stroke volume and increased pulse wave velocity. Therefore, ISH in young individuals is not always benign. In contrast, ISH in the elderly is always due to vascular aging and arterial stiffening. Framingham study has underscored the prognostic significance of both systolic and pulse pressures as independent risk factors in older persons. Compelling data from three large placebo- controlled, double-blind, randomized clinical trials (Systolic Hypertension in the Elderly Program, The Systolic Hypertension in Europe Trial, and The Systolic Hypertension in China Trial) directly demonstrate the benefits of treating systolic hypertension. Because angiotensin II contributes to arterial stiffening, Inhibitors of renin-angiotensin system may be superior to other classes of antihypertensive agents in the treatment of ISH in the elderly. Although angiotensin-converting enzyme inhibitors (ACEIs) are recommended therapies for controlling blood pressure in patients with hypertension, including the elderly, ACEIs are associated with distinctive adverse events that may limit their tolerability, including a dry, persistent cough. Consequently, alternative antihypertensive therapies are required to improve the management of hypertension in elderly patients. In a 36-week, randomized, double-blind, parallel-group, active-controlled, optional-titration study in 901 patients 65 years of age with systolic blood pressure 140 mm Hg, aliskiren proved to be more effective and better overall anti-hypertensive therapy compared to ramipril.
Expanding Indications Of Statin Use In Clinical Practice
Lung-Ching Chen, MD Department of Critical Care Medicine, Taipei Veterans General Hospital 陳隆景 台北榮民總醫院重症醫學部
The use of statin has almost become a routine in the management of patients with atherosclerotic vascular disease. Based on the evidences obtained from observational studies, randomized controlled trials and meta-analyses, current US and European guidelines recommend a more aggressive approach of lipid lowering with statin to achieve a lower LDL cholesterol target which will translate into better CV outcome. Apart from benefit derived from chronic statin use, growing evidence also demonstrated potential improvement in patient outcome when statin treatment is initiated in an acute setting, such as in the early phase of acute coronary syndrome, shortly before performing percutaneous coronary intervention (PCI), or before doing a vascular surgery. Attenuation of injury and inflammation associated with vascular procedure or PCI is an important concept in cardiovascular medicine. Vascular injury and inflammation occurring in the context of vascular surgery or PCI leading to periprocedural infarction is likely the result of embolization of particulate matter into the microcirculation. Many studies have demonstrated an association between elevated inflammatory states and adverse events following PCI. Attempts to suppress inflammation during vascular surgery or PCI may therefore have the potential to lead to favorable outcomes. The potential mechanisms of atherosclerotic plaque stabilization resulting from statin treatment include reduction of inflammation, improvement of endothelial function, increase of NO availability, thickening of fibrous cap, removing lipids and reduction of thrombosis. The ARMYDA-ACS study showed that even a short atorvastatin pretreatment prior to PCI may improve outcome in patients and acute coronary syndrome, in which the benefit is mostly driven by a reduction of peri-procedural myocardial infarction. The ARMYDA-RECAPTURE study suggested that reloading with high dose atorvastatin is associated with improved clinical outcome in patients on chronic statin therapy undergoing PCI. Results from the above two studies may potentially influence our routine clinical practice when we manage our ACS or PCI patients.