Chapter (1) Rapidly progressive glomerulonephritis
Chapter (1)
Rapidly progressive glomerulonephritis (RPGN)
RPGN is one of the nephrology emergencies which need special attention. RPGN is a clinical description which determines by symptoms and signs of glomerulonephritis (GN); edema, hypertension and gross hematuria, and evidence of acute renal failure (severe decrease in glomerular filtration rate presents as oliguria or anuria, and increased serum levels of BUN and creatinine) (George et al., 2015).
Definite diagnosis of the disorder is based on kidney biopsy's findings. Early diagnosis and appropriate treatment plays a critical role in renal saving and preventing permanent glomerular damage (George et al., 2015).
RPGN is defined as a syndrome with abrupt or insidious onset of hematuria, proteinuria, anemia, and rapidly progressing acute renal failure(ARF), and special findings on light microscopy examination of kidney biopsy's specimen; crescentic lesions which usually involved most glomerular architectures . It also characterized by rapid loss of renal function (GFR<50% within 3 months) with histological findings of crescent lesions which usually involves>50 % of glomeruli (Tarzi et al., 2011).
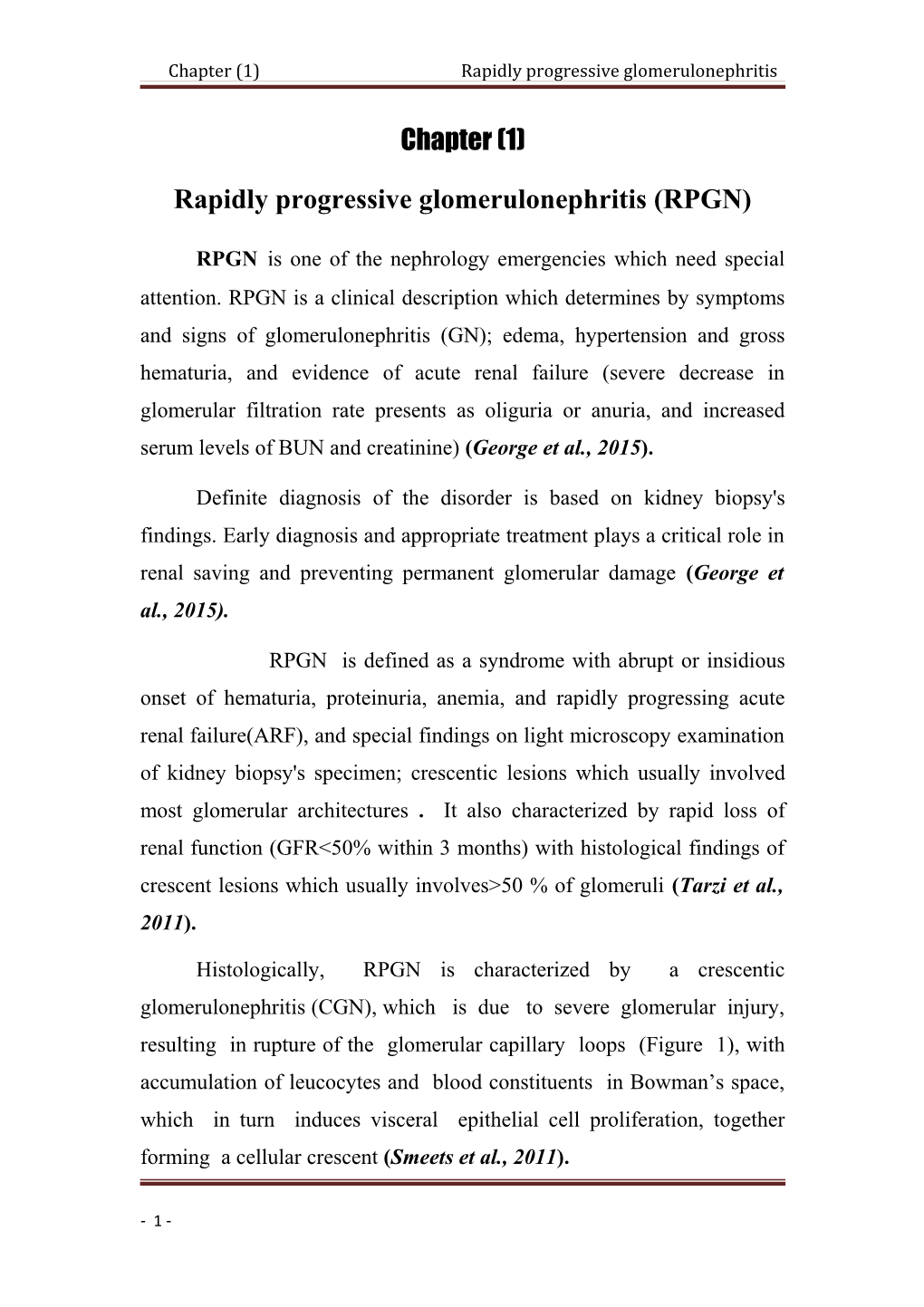
Histologically, RPGN is characterized by a crescentic glomerulonephritis (CGN), which is due to severe glomerular injury, resulting in rupture of the glomerular capillary loops (Figure 1), with accumulation of leucocytes and blood constituents in Bowman’s space, which in turn induces visceral epithelial cell proliferation, together forming a cellular crescent (Smeets et al., 2011).
- 1 - Fig. (1): Glomerulus showing crescentic glomerulonephritis due to pauci- immune ANCA-associated vasculitis, with a segmental area of thrombosis, tuft disruption and cells in Bowman’s space (Haematoxylin and eosin×400) (Smeets et al., 2011).
CGN is defined pathologically (for most glomerular diseases) when >50% of glomeruli have crescents, which are identified on light microscopy by the presence of at least two layers of cells in Bowman’s space. However, this cut-off is arbitrary and clearly severe glomerular injury can occur and result in a rapid decline of renal function with a lower proportion of crescents, There are other conditions that can lead to a clinical syndrome of RPGN, which are not caused by severe glomerular. These include thrombotic microangiopathies and rarely cases of tubulointerstitial nephritis, making it important to make a firm diagnosis based on clinical, haematological, serological and renal biopsy data (George et al., 2015). Chapter (1) Rapidly progressive glomerulonephritis
Causes of rapidly progressive glomerulonephritis
Table (1): Diagnostic Causes of Rapidly Progressive Renal Failure 1. Primary Renal Diseases a. Glomerular diseases a.i. Renal limited Vasculitis: Microscopic polyangiitis, ANCA neg. pauci-immune GN, Goodpasture’s disease a.ii. Post-infective crescentic glomerulonephritis a.iii. Idiopathic Collapsing glomerulopathy a.iv. IgA nephropathy, Membrano-proliferative glomerulonephritis a.v. Fibrillary glomerulonephritis b. Tubulo-interstitial diseases b.i. Acute interstitial nephritis b.ii. Acute tubular necrosis c. Vascular diseases c.i. Atheromatous and thrombo-embolic renovascular disease c.ii. Bilateral renal vein thrombosis 2. Systemic diseases affecting the kidney a. Systemic vasculitis a.i. Wegener’s granulomatosis a.ii. Churg-Strauss Syndrome a.iii. Goodpasture’s syndrome a.iv. Henoch-Schonlein Purpura a.v. Cryoglobulinemia a.vi. Drugs- hydrallazine, allopurinol, rifampicin, propylthiouracil, carbimazole a.vii. Rheumatoid vasculitis, paraneoplastic vasculitis b. Multiple myeloma c. Systemic Lupus Erythematosus c.i. Class IV lupus nephritis c.ii. Antiphospholipid antibody syndrome d. Thrombotic microangiopathy d.i. HUS / TTP d.ii. Malignant hypertension d.iii. Systemic sclerosis e. Infections e.i. Infective endocarditis e.ii. Occult viscera sepsis e.iii. Hepatitis C f. Sarcoidosis g. Obstructive nephropathy g.i. Retroperitoneal fibrosis g.ii. Pelvic malignancy eg carcinoma cervix
- 3 - (Dipankar et al., 2011)
RPGN can be primary or secondary. Secondary forms occur in any form of severe glomerulonephritis including membranoproliferative GN, IgA nephropathy, post infectious GN, and systemic lupus erythematous (SLE) (Appel et al., 2010).
Primary RPGN is an autoimmune disease which is divided into three immunopathologic categories :
-Type 1 RPGN: glomerulonephritis with antibodies directed against the glomerular basement membrane (GBM) (anti-GBM mediated GN) .
-Type II RPGN: immune-complex induced glomerulonephritis
-Type III RPGN: Antineutrophil cytoplasmic antibody associated glomerulonephritis (ANCA-associated glomerulonephritis or pauci- immune GN) (Appel et al., 2010).
Type 1 account for only 10% of crescentic GN. Goodpasture syndrome is the typical example of this category. In normal GBM, alpha 3, alpha 4, and alpha 5 type IV collagen have a hexamer structure and are cross-linked to adjacent NC1 domains to form dimers (D isoform).In patients with Goodpasture syndrome, there are linear deposits of immunoglobulins G (IgG) directed against the non-collagenous 1(NC1) domain of the alpha-3 chain of type IV collagen in the GBM and in the membrane of pulmonary alveoli. Antibodies against alpha 5(IV)NC1 have also been identified in anti GBM disease (Pedchenko et al., 2010).
The etiology of Goodpasture syndrome is still unknown. Genetic and environmental factors may predispose patients to the development of the Goodpasture syndrome. It has been shown that autoimmunity to the NC1 domain of the alpha3-chain of type IV collagen is strongly associated with HLA-DR15. However, alpha3 (IV) NC1 presentation to Chapter (1) Rapidly progressive glomerulonephritis
T cells seems to be determined more by “processing factors” than by the preferences of relatively indiscriminate DR15 molecules . Smoking, viral respiratory infection or exposure to hydrocarbon solvents may be frequently associated with Goodpasture syndrome and may contribute to its development. (Pedchenko et al., 2010).
Other defined Goodpasture syndrome as an autoimmune “conformeropathy”. Accordingly, the disease is triggered by a perturbation of the quaternary structure of the alpha345NC1 hexamer, inducing a pathogenic conformational change in the alpha3NC1 and alpha5NC1 subunits, which in turn elicits autoantibody formation (Dammacco et al., 2013).
The injury caused by antibodies can produce gaps in the glomerular capillary wall that allow the entrance of coagulation factors and inflammatory cells in the Bowman space, where they promote crescent formation Although direct injury involving local production of complement and polymorph nuclear activation is probably the main cause for activating parietal epithelial cells, it is likely that T cell response and regulation may also play a pathogenetic role (Tarzi et al., 2011).
Almost all cases of Goodpasture syndrome present with rapidly progressive GN. The nephritic syndrome is often associated with anemia, pulmonary hemorrhage and dyspnea. The diagnosis can be confirmed by detecting anti-GBM antibodies in the blood and by immunofluorescence analysis of kidney tissue showing linear deposits of IgG along the GBM .In 10 to 38% of patients, anti-myeloperoxidase cytoplasmic antibodies (p-ANCA) or, more rarely, anti-proteinase-3 neutrophil cytoplasmic antibodies (c-ANCA) may also be detected (Lahmer et al., 2012).
- 5 - Rare cases of membranous nephropathy preceding or following recovery from Goodpasture syndrome have been reported, suggesting the possibility of increased antigen synthesis, exposure of cryptic epitopes, and/or capping and shedding of antigen–antibody complexes ( Troxell et al., 2006).
Detection of antibodies to phospholipase A2 is crucial to discriminate between patients with primary MN and those with a secondary form of the disease, as both forms require different diagnostic approaches and treatment strategies (Schlumberger et al., 2014).
Rarely, type 1 crescentic GN may develop in patients with Alport's syndrome who receive a kidney transplant. The presence in the transplanted kidney of antigenic epitopes that are lacking in the native kidneys can trigger the production of antibodies. In most cases there is a transient IgG linear deposition along the GBM without circulating anti- GBM antibodies, but in 3% to 12% of patients anti-GBM antibodies can produce severe crescentic glomerulonephritis (Byrne et al., 2002). The epitopes recognized by the anti-GBM antibodies in X-linked Alport’s syndrome are non-cryptic intact hexamer of the alpha5NCI, unlike those of the classic Goodpasture syndrome in the native kidneys (Pedchenko et al., 2010).
Type 2 accounts for 15–20% of crescentic GN. It is a heterogeneous group of rapidly progressive GN characterized by granular deposits of immunoglobulins. Different immune-complex diseases may contribute to develop type II crescentic GN, including post- infectious acute GN (Nasr et al., 2008), lupus nephritis (Borchers et al., 2012), Henoch–Schonlein Purpura, mixed cryoglobulinemia (Kawasaki et al., 2004), IgA nephritis, immune-complex mediated membrano- Chapter (1) Rapidly progressive glomerulonephritis proliferative glomerulonephritis, diabetic glomerulosclerosis and primitive or secondary amyloidosis (Nasr et al., 2008).
The occurrence of crescentic GN has been estimated to range around 16% for post infectious GN, 8% for lupus nephritis, 2.7% for adults with Henoch–Schonlein Purpura, and 11% for cryoglobulinemic nephritis (Moroni et al., 2002).
In these diseases the deposition of circulating immune complexes in the GBM or in situ formation of immune complexes within the glomerular capillaries activates inflammatory cells and complement causing damage to the GBM .Moreover the glomerular injury may trigger inflammation and activate the innate immune response with recruitment of macrophages, natural killer cells, granulocytes and maturation of dendritic cells which stimulate the adaptive immune response with production of TH1 and TH17 cell. (Summers et al., 2014).
Type 3 is the most common form of crescentic GN accounting for around 60–80% of all cases. It was the most frequent cause of acute renal kidney injury reported in the Italian registry of kidney biopsies. This type of crescentic GN is characterized by the absence of immune glomerular deposits and is now considered to be a small-vessel renal vasculitis. Actually, although in a few patients who present the typical clinical and pathological features of crescentic GN without immune deposits the signs of vasculitis are absent, most of the afflicted patients have circulating ANCA and signs of systemic vasculitis. type 3 crescentic GN classified as ANCA-associated vasculitis (AAV) .This term includes microscopic polyangiitis (MPA), granulomatosis with polyangiitis (GPA), eosinophilic granulomatosis with polyangiitis (EGPA) (Jennette et al., 2012).
- 7 - In study of 89 patients with AAV and renal involvement crescentic GN developed in 70% of patients with GPA and in 65% of patients with MPA. Crescentic GN was rarer in EGPA with renal involvement accounting for only 13.8% of cases (Sinico et al., 2006).
All these conditions, although with difference in prevalence, share renal lesions characterized by diffuse extra capillary proliferation and necrotizing inflammation of capillaries, venules, arterioles and small arteries (Lyons et al., 2012).However, the accompanying signs and symptoms are different. In all the three diseases lesions of skin, gastrointestinal system and neurologic system may be present . In GPA the renal lesions are usually associated with granulomatous involvement of the respiratory tract, ear, nose and throat. EGPA is associated with asthma, eosinophilia and granulomatous inflammation. In MPA asthma and granuloma are generally absent while pulmonary capillaritis often occurs. Around 75% of patients with GPA have circulating cANCA, 20% have pANCA and only 5% have negative ANCA. In MPA around 10% of patients have undetectable ANCA, while around 50% of patients are pANCA positive and 40% cANCA positive. About 1/3 of patients with EGPA do not have circulating ANCA, 60% are positive for pANCA, in particular those with renal involvement and only 10–20% are cANCA positive. The majority of patients with pauci-immune GN are pANCA positive (Jennette et al., 2012).
Symptoms and Signs
• General fatigue, slight fever, appetite loss, flu-like symptoms, and abnormal body weight loss are also frequently observed. Chapter (1) Rapidly progressive glomerulonephritis
• Microscopic, or occasionally macroscopic, hematuria is observed accompanied by dimorphism of red blood cells and cellular cast formation.
• Proteinuria is frequently present; however, nephrotic syndrome accompanying systemic edema is rare. Asymptomatic cases found through urinary screening during sporadic health checks are increasing
(Matsuo et al., 2011).
When the causative disease of RPGN is systemic (vasculitis, systemic lupus erythematosus, etc.), a variety of extra renal symptoms are observed, such as:
disorders of the upper respiratory tract, lung (pulmonary bleeding, interstitial pneumonitis),
skin (purpura, erythema),
Digestive organ (melena, abdominal pain), or neurons (Matsuo et al., 2011).
In blood chemistry tests:
• Elevation of serum creatinine
• Decrease of estimated glomerular filtration rate
• Elevation of C - reactive protein (CRP)
• Rapidly progressive anemia, gradual elevation of neutrophil- dominant white blood cells, and thrombocytes are frequently observed.
- 9 - • Complement levels tend to be elevated in RPGN because of systemic vasculitis; in contrast, systemic lupus erythematosus (SLE) decreases complement levels.
Autoantibodies for detecting the causative disease of RPGN, anti- glomerular basement membrane (GBM) antibody, ANCA, and anti-dsDNA antibody are highly specific.
Concerning signs in renal imaging, renal atrophy on echography is relatively rare.
Renal pathology frequently reveals crescentic glomerulonephritis (Matsuo et al., 2011).
Histopathology characteristics of RPGN :
1- Light microscopy findings
Histopathologically, RPGN is characterized by a vasculitis which involves glomerular capillaries, and results in formation of cellular crescents within most glomeruli .The hallmark histologic lesions are crescents; a morphologic expression of severe glomerular injury. In severe glomerular injury rupture of the glomerular capillaries allows inflammatory mediators to spill into Bowman's space, resulting in epithelial cell proliferation and invasion of monocyte and macrophage to Bowman's space (Thomas et al., 2001).
Crescents are divided into cellular, fibro cellular or fibrous types. Hallmarks of irreversible glomerular or tubulointerstitial injuries are glomerular sclerosis, fibrous or fibro cellular crescents, and interstitial fibrosis. The lesions usually are seen in various stages of activity or Chapter (1) Rapidly progressive glomerulonephritis resolution. Necrotizing inflammation in small cortical arteries is reported in 10 % of biopsy specimens .Inflammation of medullary vasarectae with papillary necrosis is another finding that may be found (Lionaki et al., 2007).
In acute pauci-immune glomerulonephritis (RPGN type III) fibrinoid necrosis accompanies crescents. These lesions occur at the same frequency irrespective of the presence or absence of associated vasculitis .Acute lesions range from focal segmental fibrinoid necrosis affecting less than 10 %of glomeruli to severe diffuse necrotizing and crescentic glomerulonephritis that may injure all glomeruli. Periglomerular granulomatous inflammation may occur, but is not specific for pauci-immune glomerulonephritis (Lionaki et al., 2007).
2-Histopathology characteristics on immunoflurecent microscopy:
Anti-GBM glomerulonephritis characterized by linear staining for IgG and usually C3 along the glomerular capillary. Immune complex- mediated glomerulonephritis, which is found in severe forms of various types of glomerulonephritis such as PSGN, IgA nephropathy, and lupus nephritis, characterized by granular glomerular staining for one or more immunoglobulins and/or complement components, and pauci-immune glomerulonephritis characterized by mild or absent glomerular tuft staining for immunoglobulins and/or complement (Rutgers et al., 2005) .
Anti-neutrophil cytoplasmic antibodies (ANCAs) associated glomerulonephritis are usually pauci immune; however, immunofluorescence microscopy often reveals a low level of staining (less than +2, in the 0–4 scale Figure2
- 11 - Fig. (2): Histopathologic findings in light and immunoflurecent microscopy a/left; light microscopic demonstration of ANCA-associated necrotizing GN (with a crescent), arrows; (alveolar capillaritis with intra-alveolar hemorrhage); arrow; middle (and pulmonary necrotizing granulomatous inflammation with a multinucleated giant cell) arrow; right b/middle; Immunofluorescence microscopy can separate crescentic glomerulonephritis into anti-GBM with linear IgG staining, ( left) immune complex with granular staining, (right); or pauci-immune categories with little or no immunoglobulin staining(Lionakiet al., 2007). 3-Electron microscopy findings:
On electron microscopy examination absence of electron-dense immune complex deposits (type I RPGN), multiple electron-dense deposits (type II RPGN), and few or no electron-dense deposits (typeIII RPGN) are main findings (figure 3) (Haas et al., 2004). Chapter (1) Rapidly progressive glomerulonephritis
Fig. (2): Electron microscopy findings C: Electron microscopy showing multiple sub-epithelial electron-dense deposits, some appearing partially resorbed, with extension of the glomerular basement membrane (GBM) around the deposits (uranyl acetate and lead citrate stain, original magnification ×6300) F: Electron microscopy showing a large sub epithelial deposit in a “notch” area (arrow), as well as mesangial deposits (uranylacetate and lead citrate stain, original magnification×3800(Haas &Eustace, 2004).
Anti-neutrophil cytoplasmic and anti-GBM antibodies:
Anti-neutrophil cytoplasmic antibodies (ANCAs )are characteristic markers of small vessel vasculitides; Wegener’sgranulomatosis(WG), Microscopic polyangiitis(MPA), Churg-Strauss Syndrome(CSS), and idiopathic pauci-immune necrotizing glomerulonephritis for them the term ANCA associated vasculitides(AAV) has long being used (Seo et al., 2004).
The standard approach for detection of ANCA is indirect immunofluorescence (IIF) technique followed by antigen-specific quantitative assays .Myeloperoxidase (MPO) and proteinase3 (PR3) are major ANCA antigens (Hauer et al., 2002).
In patients with RPGN, there are two major sub classes of ANCA, namely perinuclear (p -ANCA) and cytoplasmic (c -ANCA) .The main epitope of p-ANCA is myeloperoxidase(MPO), and that of c-ANCA is proteinase-3 (PR3) (Lionaki et al., 2007).
MPO-ANCA is a useful serum marker for MPA and idiopathic pauci-immune crescentic GN, and PR3-ANCA is regarded as a serum marker for Wegener’s granulomatosis and MPA (Lionaki et al., 2007).
Approximately80- 85% of cases of pauci-immune crescentic glomerulonephritis are ANCA positive. Greater than 95% of cytoplasmic
- 13 - ANCA are PR3-ANCA and >95 %of perinuclear ANCA are MPO- ANCA (Lionakiet al., 2007).
Anti-GBM antibodies which are directed to the non-collagenous part of the α 3 chain of type IV collagen, can also be evaluated by both IIF and ELISA(Rutgers et al., 2005) .The ANCA-GBM dot-blot is a qualitative assay that uses nitrocellulose strips on which purified antigens are blotted at preset spots .MPO and PR3 antigens that are used in these tests are produced from human leukocytes .The GBM-ANCA dot-blot assay has been revealed reactivities that had not been detected by ELISA(Table 2) (Rutgers et al., 2005).
Table (2): Characteristics of the GBM-ANCA Dot-Blot Assay
(Rutgers et al., 2005).
RPGN, Pulmonary–renal syndrome (PRS), and ANCA-associated vasculitis (AAVs):
The ANCA-associated vasculitis(WG, MPA, and CSS) are a group of autoimmune conditions characterized by the development of necrotizing vasculitis .They share a number of clinical features and are therefore treated using similar treatment protocols.The AAVs are rare with an annual incidence of 20/million in Europe, with WG as the most common and CSS the least frequent (Ntatsaki et al., 2011).
In far-east, MPA is more common than WG .It's thought that they arise from interaction between an environmental factor and a genetically predisposing agent(Ntatsaki et al., 2011). Chapter (1) Rapidly progressive glomerulonephritis
Pulmonary–renal syndrome (PRS) is defined as combination of diffuse alveolar hemorrhage (DAH) and glomerulonephritis(Seo et al., 2004).
This syndrome is caused by different diseases, including various forms of primary systemic vasculitis especially WG and MPA, ANCA- associated systemic vasculitis(AAV), Good pasture's syndrome, SLE, and infection-associated or drug induced glomerulonephritis (Mitra Naseri, 2011).
Immunologic injuries or non-immunologic mechanisms are involved in pathogenesis of PRS .Immunologic mechanisms such as production of anti-GBM antibodies, ANCA, immune complexes mediated injuries and non-immunologic mechanisms such as thrombotic microangiopathy have been suggested .Pulmonary involvement in the majority of cases is the result of small-vessel vasculitis that involves arterioles, venules and alveolar capillaries (necrotic pulmonary capillaritis). These lesions are clinically expressed with diffuse alveolar haemorrhage (DAH)(Jayne et al., 2000).
In the majority of cases the underlying renal pathology is a form of focal proliferative glomerulonephritis with fibrinoid necrosis, as well as micro vascular thrombi, and extensive crescent formation accompanies glomerular tuft disease (Walters et al., 2010).
According to results of ANCA pulmonary renal syndrome can be categorized into two sub-groups:
1. ANCA-positive Pulmonary–renal syndrome
2. ANCA-negative Pulmonary–renal syndrome
- 15 - Majority of cases of pulmonary-renal syndromes are related to ANCA associated vasculitis (Mitra Naseri, 2011).
Pulmonary–renal syndrome in ANCA-negative systemic vasculitis is very rare and has been reported in Behçet’s disease, HSP, IgA nephropathy and in mixed cryoglobulinaemia and rarely in thrombotic thrombocytopenic purpura(TTP) (Mitra Naseri, 2011).
Wegener's granulomatosis (WG): Their diagnosis was based on upper and lower respiratory tract complications, renal disease, and variable involvement of other organs with disseminated vasculitis .Tissue biopsies confirmed the characteristic clinical findings , Pathologically Wegener’s granulomatosis was characterized by small-vessel necrotizing vasculitis and granulomatous inflammation involving mostly the upper and lower respiratory tracts and the kidneys (Mitra Naseri, 2011).
Diffuse alveolar hemorrhage (DAH) is the most serious complication in small-vessel vasculitis. Respiratory symptoms including cough and hemoptysis. CXR or chest CT-scan may reveal diffuse lung infiltrate. Clinical manifestations, pathologic and serologic findings play important role in the diagnosis of WG. 75- 90 %of patients with active disease have PR3-ANCAs (Ozaki et al., 2007).
The role of PR3-ANCA in the pathogenesis of the disease is not clear, but in vitro evidence suggests that PR3-ANCA can directly or indirectly damage endothelial cells (Mitra Naseri, 2011 ).
ANCA-positive patients with clinical presentations of WG such as sinusitis, pulmonary infiltrates, nephritis, and documented necrotizing vasculitis, but without biopsy-proven granulomatous in flammation. Both classic Wegener’s granulomatosis and Wegner's vasculitis are different manifestations of the same disease process. (Mitra Naseri, 2011 ). Chapter (1) Rapidly progressive glomerulonephritis
Microscopic polyangiitis (MPA):
Renal and pulmonary symptoms are characteristic in MPA, and interstitial pneumonitis and pulmonary hemorrhage are common clinical features .MPO-ANCA is positive in 50-75% of patients and biopsy of the lung and kidney reveals necrotizing vasculitis of arterioles, capillaries, and venules with few immune deposits necrotizing and crescentic GN (Ozaki; 2007).
Table (3): Diagnostic criteria for microscopic polyangiitis(Ozaki, 2007).
- 17 - Allergic granulomatous angiitis (AGA) or Churg-Strauss syndrome(CSS)
Churg and Strauss was firstly described allergic granulomatous angiitis(Churg, & Strauss, 1951). The disease is characterized by presence of asthma, eosinophilia, and necrotizing granulomatous inflammation .Clinical manifestations of small-vessel vasculitis; palpable purpura of the lower extremities, mononeuritis multiplex, abdominal pain, and gastrointestinal bleeding develop several years after the onset of asthma. Positive MPO-ANCA are seen and skin biopsy shows necrotizing vasculitis of small vessels with massive eosinophilic infiltration and extravascular granulomatosis(Ozaki, 2007).
SLE and AAV Chapter (1) Rapidly progressive glomerulonephritis
Systemic lupus erythromatosis is an autoimmune disorder .Variety of autoantibodies are present in SLE patients including ANCA which have been reported in 3-69 %of cases( Pradhan et al., 2004).
In Pradhan et al's study predominant ANCA pattern was p-ANCAwhile c- ANCApattern was not found in any patient(Pradhan et al., 2004).
Their study revealed that ANCA can be used as a serological marker to differentiate vasculitides in lupus nephritis cases from SLE without nephritis.
Table (4): presents diagnostic criteria for CSS
(Ozaki, 2007).
- 19 - Epidemiology and prognosis
1) Epidemiology:
RPGN is a rare renal disease; however, the number of Japanese patients with RPGN has increased in last years. Although the precise incidence of RPGN in Japan or worldwide is not known. Based on a questionnaire survey of 1,772 Japanese cases collected from1989 to 2007, the most common clinical form of RPGN in this country is pauci- immune-type necrotizing glomerulonephritis without systemic vasculitis, and the second most common form is microscopic polyangiitis. In recent years, the age at onset has increased (Watanabe et al., 2011).
Crescentic glomerulonephritis is rare, it accounted for 13% out of patients submitted to renal biopsy over a period of 7 years in Italy . Although immune-complex crescentic GN may occur at any age, lupus is typical of women in childbearing age, Henoch–Schonlein purpura is more frequent in childhood and adolescence, mixed cryoglobulinemia and AAV present more frequently between the fifth and the seventh decades of life (Gabriella et al., 2014).
Goodpasture syndrome may have a bimodal distribution, being more frequent in the 2nd–3rd decades, when it mainly affects males, and in the 6th decade of life when it preferentially affects females (Fomegné et al., 2006).
Post- infectious GN is frequent in underdeveloped countries and in subjects with poor socioeconomic conditions. Lupus nephritis is more rare in Caucasian subjects than in Asian populations (Mahr et al., 2004).
2) Prognosis:
The survival and renal prognosis of RPGN or ANCA-associated RPGN has improved in last years. In contrast, patients with anti-GBM Chapter (1) Rapidly progressive glomerulonephritis antibody-associated RPGN show an extremely poor prognosis. Infection has been, and continues to be, the leading cause of death in patients with RPGN(Watanabe et al., 2011).
Independently of the original disease, the prognosis of crescentic GN was ominous until a few years ago. Modern treatment has improved the outcome .All patients who required immediate dialysis and had 100% crescents on renal biopsy remained dialysis dependent (Gabriella et al.,
- 21 - 2014).
Fig. (4): Algorithm for Differential diagnosis of Rapidly progressive glomerulonephritis (Dipankar et al., 2011) Chapter (1) Rapidly progressive glomerulonephritis
- 23 -