Highland NHS Board 1 May 2007 Item 8.4
THE CLINICAL LEADERSHIP PROGRAMME IN NHS HIGHLAND BENEFITS REALISATION REPORT
Report by Nigel Hobson, Associate Director of Nursing Jennifer Lobban, Lead Facilitator Clinical Leadership Programmes NHS Highland For Heidi May Board Nurse Director
The Board is asked to:
Note improvements in service quality for patients. Note the positive impact on staff motivation. Support the continuation of clinical leadership development programme.
1. Background
(i) NHS Highland’s Clinical Leadership Development Programmes run in association with the Royal College of Nursing enables clinical leaders to develop practical strategies to use with their teams to improve patient care. The programmes’ strengths lie in their practical, person and patient focused perspective. The programmes have been rigorously evaluated and quality assured at national and local levels.
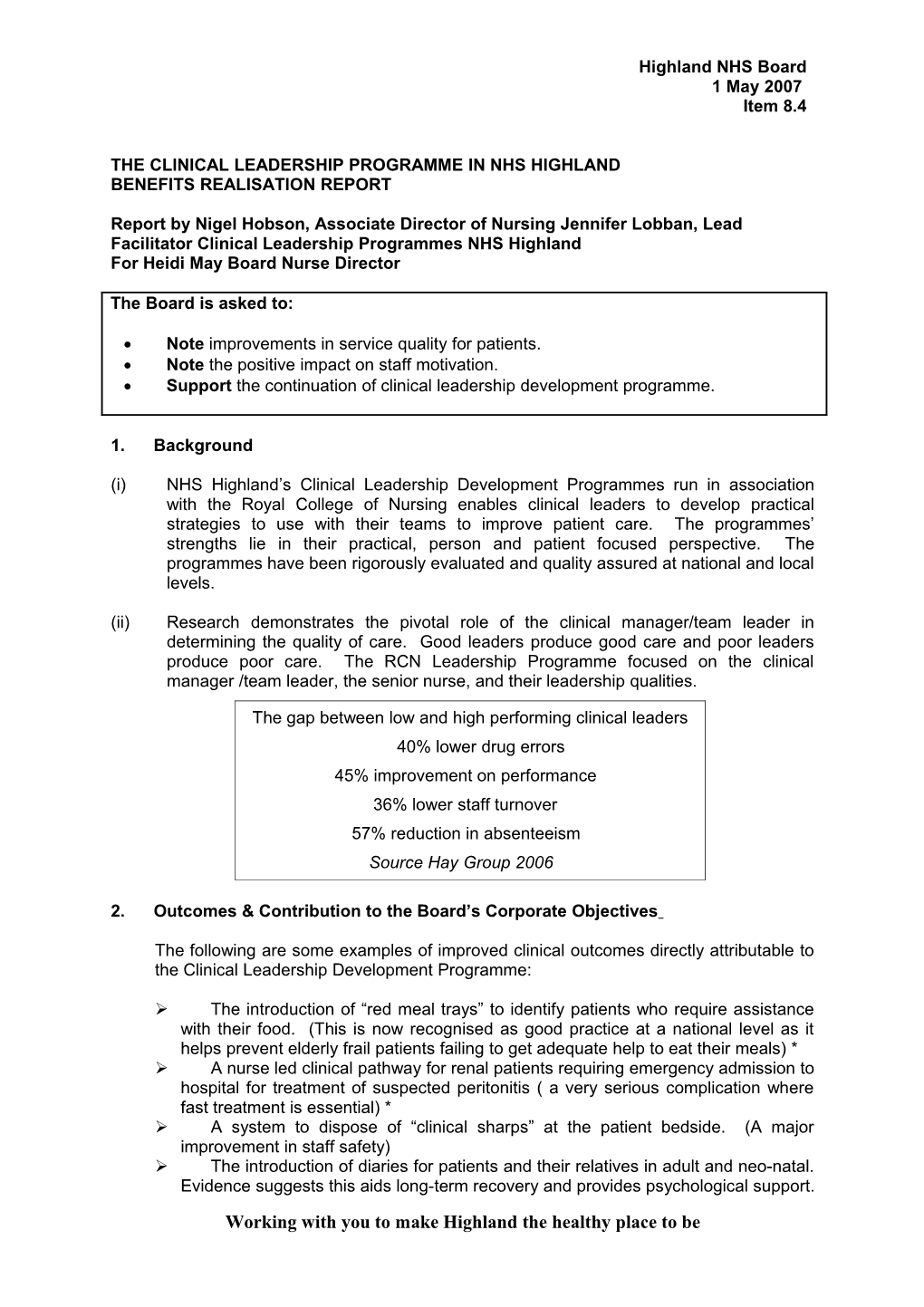
(ii) Research demonstrates the pivotal role of the clinical manager/team leader in determining the quality of care. Good leaders produce good care and poor leaders produce poor care. The RCN Leadership Programme focused on the clinical manager /team leader, the senior nurse, and their leadership qualities.
The gap between low and high performing clinical leaders 57% reduction in absenteeism 40% lower drug errors 45% improvementSource Hay on Groupperformance 2006 36% lower staff turnover 57% reduction in absenteeism Source Hay Group 2006
2. Outcomes & Contribution to the Board’s Corporate Objectives
The following are some examples of improved clinical outcomes directly attributable to the Clinical Leadership Development Programme:
The introduction of “red meal trays” to identify patients who require assistance with their food. (This is now recognised as good practice at a national level as it helps prevent elderly frail patients failing to get adequate help to eat their meals) * A nurse led clinical pathway for renal patients requiring emergency admission to hospital for treatment of suspected peritonitis ( a very serious complication where fast treatment is essential) * A system to dispose of “clinical sharps” at the patient bedside. (A major improvement in staff safety) The introduction of diaries for patients and their relatives in adult and neo-natal. Evidence suggests this aids long-term recovery and provides psychological support. Working with you to make Highland the healthy place to be Exchange training for staff from different NHS Highland sites. (An excellent form of staff development, and an increased understanding of different specialties/systems of work)
* The results of these projects were chosen by the RCN as detailed case studies included in their national evaluation document
3. Governance Implications
(i) Clinical & Patient Focus
The strength of these programmes is their clinical focus. In other words, they develop our clinical leaders in ways which help them to focus their team on clinical quality patient safety, and improved clinical processes. Part of the programme involves observing care in another clinical environment and conducting interviews with patients, both of which help the leaders to gain greater insight of the patient’s perspective. Action Learning Sets (ALS) are established for all course attendees. These ALS continue after a course has been completed and contribute significantly to the Clinical Supervision of Nursing, Midwifery and AHP staff.
(ii) Staff & Financial
The contribution health care professionals make towards delivering safe, high quality, patient focused care in NHS Highland is of the utmost significance.
Every contact NHS Highland staff have with patients and / or relatives be it in a hospital or community setting can make a profound difference to those individuals. As well as the patient themselves, it affects the wellbeing of their family and friends, and the reputation of NHS Highland stands or falls by what patients/relatives experience whilst the percentage of clinical leaders undertaking one or other programme remains small (circa 19% G Grades/Band 7). The outcomes in terms of improved clinical care, and better- motivated teams are quite evident.
Whilst the resource implications of the 9 month programme is significant in terms of staff time, the evidence from both national and local evaluations strongly support the cost benefit ratio. NHS Highland has opted to continue the RCN Leadership Programme during 2007/08 by renewing our license agreement. We believe this offers excellent value for money and enables our clinical leaders and their facilitator to network with colleagues nationally.
4. Impact Assessment
The programme itself enables clinical leaders to consider issues of diversity and access.
2 CLINICAL LEADERSHIP DEVELOPMENT PROGRAMMES IN NHS HIGHLAND BENEFITS REALISATION PAPER
1. Programme Aim and Intended Outcomes
1.1 This report is prepared for all stakeholders within NHS Highland. It will identify the main outcomes and involvement with the Royal College of Nursing (RCN).
1.2 The overall aim of the NHS Highland Clinical Leadership Development Programmes (NHS Highland CLDP) in association with the Royal College of Nursing (RCN) is to enable clinical leaders to develop practical strategies to use with their teams to improve care received by patients. The programmes’ strengths lie in its practical, needs led, person and patient focused perspective. The programme has been rigorously evaluated and quality assured.
2. Background
2.1 NHS Highland’s model of Clinical Leadership is based on the models described in the Leadership Qualities Framework of the Critical Leadership Behaviours and the RCN Clinical Leadership Development Programmes. The NHS Highland model seeks to combine the research that informs these models and to adapt them to meet the needs of NHS Highland. 2.2 The NHS Highland CLDP in association with the RCN is based on the understanding that although employers can influence the quality of patient care, it is the qualities of individual health care professional which have a more direct effect on how patients are looked after.
2.3 Current national policy places clinical leadership at the heart of modernising the NHS. (Delivering care, enabling health, November 2006). There is now global recognition that quality improvement can be achieved by empowering and enabling health care professionals, at a local level, to become more effective problem solvers and team players (RCN, 2000., Scottish Executive, 2006)
2.4 It is clear from existing research the pivotal role of the clinical manager/team leader in determining the quality of care delivered within a clinical area (hospital or community). Good leaders produce good care and poor leaders produce poor care. The RCN Ward Leadership Project focused on the clinical manager /team leader, the senior nurse, and their leadership qualities. The project aimed to promote better practice by identifying the skills needed by the clinical manager/team leaders to make them more effective, thus demonstrating how those skills could then be transferred to themselves, to their patients, their teams and to the organisation.
The gap between low and high performing clinical leaders
40% lower drugs errors 45% improvement on performance 36% lower staff turnover 57% reduction in absenteeism
Source Hay Group 2006 : Nurse Leadership: being nice is not enough
3 3. Evaluation
3.1 The NHS Highland programmes were evaluated using a variety of qualitative and quantitative methods including 360-degree clinical leadership feedback, action learning audit, one to one feedback, appreciative enquiry, action plans from patient narratives and observations of care.
3.2 An independent evaluation of NHS Highland managers, Senior Nurses and Allied Health Professionals, (Caldwell, 2005) concluded the following: -
91% of those interviewed were supportive of the programme and wanted its continuation 83% believed that the programme has successfully targeted the right people There is a wider need within NHS Highland for clinical leadership development The organisation needs to consider the best vehicle for delivering wider clinical leadership development 63% considered a reduction in the programme duration. This was achieved in September 2005 by a reduction of 25% time reduction with no detrimental effects.
Fig. 1 Percentage of NHS Highland Attendees on CLDP
Leadership at the Point of Learn to Lead Care Clinical Group Total Numbers 4 Month Programme 9 month Programme Nurse D+E/ Band 5 1535 51 n/a Nurse F/Band 6 667 35 67 Nurse G+H/Band 7 560 17 92 Nurse I/Band 8 25 2 0 Pharmacy 50 0 0 AHP 353 12 12 Doctor + Others 3 2 Total Numbers 3190 120 173
August 2004 - April Dates of Programmes 2007 September 2001- June 2007
4. Some examples of improved clinical outcomes undertaken by staff attending the CLD programme include:-
Food, fluid, and nutrition. Introduction of red food trays to identify which patients require assistance with nutrition
Nurse led and developed pathway for renal patients’ emergency access to commence treatment for peritonitis without delay
Immediate sharps disposal beside patient
Introduction of diaries for ITU and Neo-natal ITU patients and relatives
Exchange training for staff from different NHS Highland sites
Positive Partner Scheme/ The Orchard – A collaborative venture with social work colleagues
4 New Ante Natal Care Pathway on trial at present
Older adults falls at home (25% of older adult admissions). Core plan introduced to get patient back into the community and not unnecessarily admitted to hospital
Information pamphlets translated into other languages including Polish and German
Use of bed rails audited following clinical governance issues. Bed sensor alarm systems now being trialled and policy under development
Eating assessment team developed at New Craigs to encourage more healthy eating
Increased awareness of stress, and how staff can access appropriate assistance
Obesity pathway to assist staff to manage patients in the community (now being audited)
Quality System introduced in Caithness General Hospital following a cleanliness audit
More information on improved quality to patients’ services is available via the Intranet on NHS Highland CLDP reports.
5. Setting Direction
5.1 The National Workforce Plan outlines the need for staff with such leadership capabilities to equip them to work strategically and interdependently with diverse partners in an ever changing political landscape.
5.2 The modernisation and reform of health services will not happen without effective clinical leadership. ( Delivering care, enabling health, 2006)
5.3 Clinical leadership can be developed across the whole service, with the appropriate investment, support and targeted activity.
5.4 Clinical leadership and management, whilst different in complexion are both necessary and related, and that development in both will be required to support the modernisation and reform of the services. (Delivering care, enabling health, 2006)
6. Contribution to Heat Targets
6.1 The evidence presented in this paper demonstrates that the clinical leadership development programmes significantly contributes to the work of NHS Highland including many aspects of the Heat Targets. Furthermore, it is entirely congruent and supportive of the NHS Highland Clinical Strategy and other local and national initiatives. E.g. Delivering Care, Enabling Health, Charge Nurse Review, Visible, Accessible and Integrated Care, Developing Community Hospitals.
Nigel Hobson, Associate Director of Nursing Jennifer M Lobban, Lead Facilitator CLDP NHS Highland
5 20 April 2007
6