Version 3.2 FINAL 8-Aug-2014
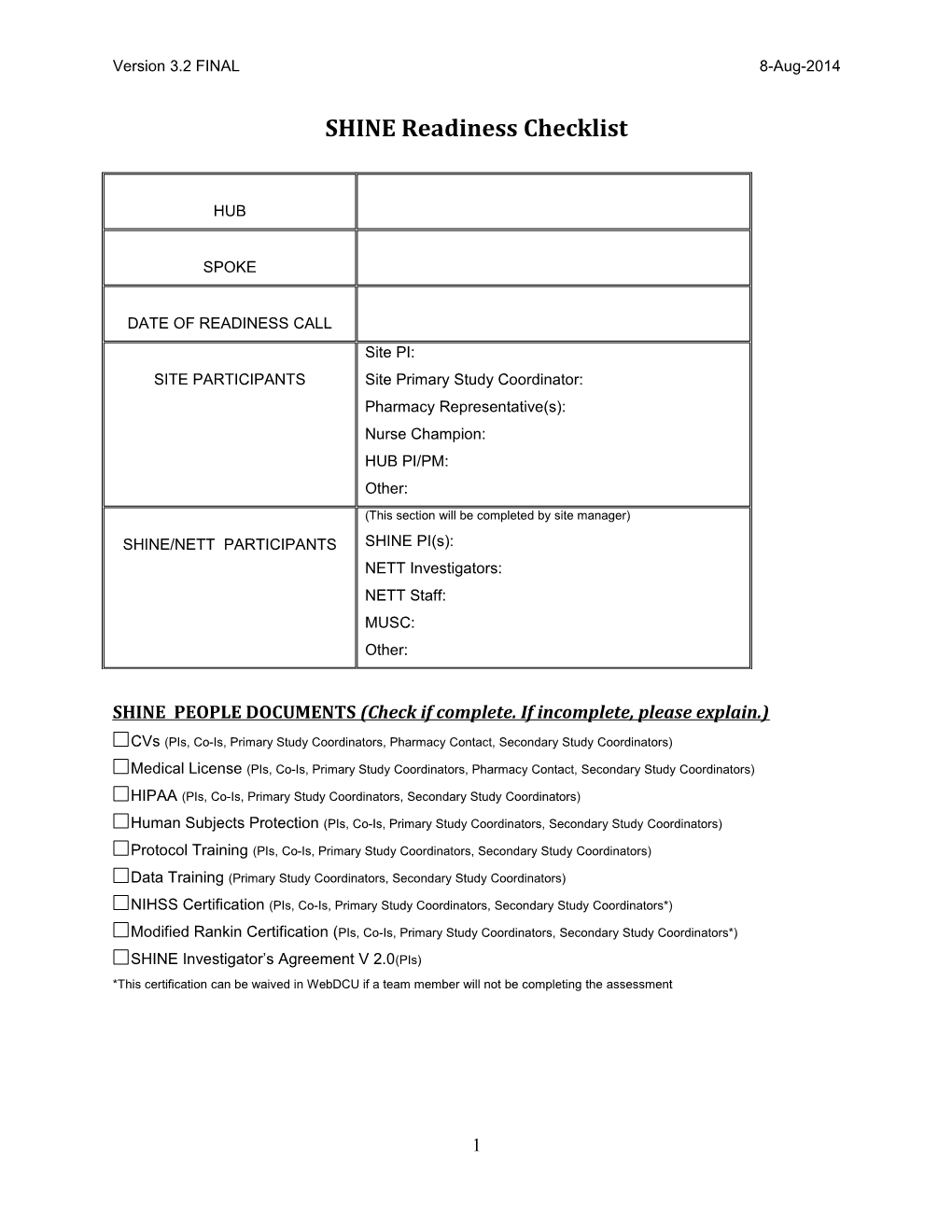
SHINE Readiness Checklist
HUB
SPOKE
DATE OF READINESS CALL Site PI: SITE PARTICIPANTS Site Primary Study Coordinator: Pharmacy Representative(s): Nurse Champion: HUB PI/PM: Other:
(This section will be completed by site manager) SHINE/NETT PARTICIPANTS SHINE PI(s): NETT Investigators: NETT Staff: MUSC: Other:
SHINE PEOPLE DOCUMENTS (Check if complete. If incomplete, please explain.)
CVs (PIs, Co-Is, Primary Study Coordinators, Pharmacy Contact, Secondary Study Coordinators)
Medical License (PIs, Co-Is, Primary Study Coordinators, Pharmacy Contact, Secondary Study Coordinators)
HIPAA (PIs, Co-Is, Primary Study Coordinators, Secondary Study Coordinators)
Human Subjects Protection (PIs, Co-Is, Primary Study Coordinators, Secondary Study Coordinators)
Protocol Training (PIs, Co-Is, Primary Study Coordinators, Secondary Study Coordinators)
Data Training (Primary Study Coordinators, Secondary Study Coordinators)
NIHSS Certification (PIs, Co-Is, Primary Study Coordinators, Secondary Study Coordinators*)
Modified Rankin Certification (PIs, Co-Is, Primary Study Coordinators, Secondary Study Coordinators*)
SHINE Investigator’s Agreement V 2.0(PIs) *This certification can be waived in WebDCU if a team member will not be completing the assessment
1 Version 3.2 FINAL 8-Aug-2014
SHINE SPOKE DOCUMENTS FWA CLIA Certification Delegation of Authority Log Full Study IRB Application Submittal for SHINE V2 IRB Approval – Protocol v2 IRB Approved ICF v3 for Protocol V2 Pharmacy Plan - Must contain plans for labeling, dispensing of insulin/normal saline for study use, order set, etc. Recruitment Plan - Must contain in ½-2 pages of prose an individualized recruitment plan that captures the strategies proven or intended for your site by imagining tracing a possible SHINE patient from presentation to the ED through completion of final handoff to receiving RN on the bedding floor. Please include all aspects of the process you feel are relevant to successful recruitment at your site. (See Parameters Document and SHINE Toolbox for further guidance and contacts.)
SHINE TRAINING Nursing staff on key units trained in study procedures (upload sign in sheets)
SHINE WebDCU ACCESS SHINE data training certificates uploaded and accepted
ISPOT Readiness I-SPOT – Readiness checklist ** Site is not participating in ISPOT
**Send completed ISPOT readiness checklist to Hannah Reimer ([email protected]) or Dr. Nina Gentile ([email protected])
2 Version 3.2 FINAL 8-Aug-2014
SHINE LOGISTICS Please consider each of the questions listed below. Using this document as a template, please enter a text response to each item. The completed document will serve as a summary of how you will be conducting the trial at your site.
1 SCREENING AND ENROLLMENT 1.1 Who in the ED and on the patient units has been identified, trained and charged with the responsibility of identifying every patient with an ischemic stroke within 12 hours and blood glucose level >110 who could be a potential participants for the SHINE study? Who will be responsible for training these individuals?
1.2 Once a potential participant is identified, who will notify the study team immediately upon recognition to complete screening, both in ED and on the floor? How does this person know whom to contact?
1.3 Define what team member (title) is responsible for managing the 24/7 call schedule. How is the study team scheduled to make a responder or responder team available 24/7 or reasonable equivalent? What is your reasonable equivalent of 24/7 study team availability if not fully available 24/7? Are days different from nights and/or weekends?
1.4 Once a patient has been identified, the study team notified, and before the study team arrives, who is designated to champion the care of the potential SHINE participant? Performing assessments: Obtaining Labs: CT: Identifying the LAR, and asking them to remain in the ED for the study team to speak with them: Pulling prepackaged SHINE trial orders, etc.: Other (describe):
1.5 Define who on the study team is responsible for each component of the screening and enrollment process:
Determining eligibility: Getting lab values: Performing assessments: Consenting: Randomizing in WebDCU: Writing study orders: Faxing/delivering orders to pharmacy: Bringing the study computer to the bedside:
3 Version 3.2 FINAL 8-Aug-2014
Setting up the study computer: Obtaining an IV pump: Obtaining study drug STAT from pharmacy: Supporting bedside nurse: Other (describe): 1.6 What is your process for obtaining and documenting informed consent?
1.7 Have you confirmed internet accessibility in your ED/patient unit for randomization?
1.8 Handling enrollments if you have competing clinical trials. 2 Does your site currently have any open trials competing with SHINE – i.e., eligibility criteria that overlap? Kindly list any competing studies. (Also include any competing studies that site anticipates will be opening to enrollment within the next 6-12 months).
3 For any studies that directly compete, provide a summary of your site’s proposed strategy for an unbiased method of alternating enrollments with SHINE (e.g. alternating preferred study week/month, etc).
3.1 How many patients do you expect to screen each month?
3.2 How many SHINE subjects do you expect to enroll each month?
4 PHARMACY/STUDY DRUG 4.1 What is your process for notifying pharmacy of a potential patient? Is there a special pharmacy that will be handling infusions for the study?
4.2 Describe how pharmacy will prepare/label the study drug infusions. How long is it expected to take?
4 Version 3.2 FINAL 8-Aug-2014
4.3 How will the study team know what is actually being given to the subject?
4.4 What is the process for obtaining additional study drug infusions as needed throughout the treatment period?
4.5 Describe plans for using floor stock for insulin/NS injections. Will D50% be available at the bedside, or on the unit?
4.6 How will study drug(s) appear in the clinical record? (What will clinicians and nurses see?) How will the nurses chart the study drug(s)?
4.7 How do you plan to assure that you will be able to retain one study drug sticker label for monitoring purposes?
5 SHINE STUDY LAPTOP 5.1 Have both study computers been inspected by biomedical engineering (if required)?
5.2 Have you verified wireless internet access in the emergency department and on the patient units for the study computers?
5.3 Where will the study computers be stored when not in use? How are they secured? Who will have access to them? How will they be moved to the patient care area/by whom?
5.4 Where do you plan to place the computers in/near the patient rooms to allow ready access by nursing while minimizing the chance for unblinding? How will they be secured? Consider this question in regard to the emergency department as well as the final bedding unit.
6 STUDY TREATMENT ADMINISTRATION 6.1 Describe the content and audience of the SHINE training you have conducted at your institution.
5 Version 3.2 FINAL 8-Aug-2014
6.2 Describe how the lead nurse will assist in protocol implementation.
6.3 What units at your hospital are capable of managing IV insulin drips? Where do you plan to admit study patients? Do you anticipate any problems with bed availability on these units? If so, how do you plan to manage this?
6.4 Who will be responsible for starting the SHINE study laptop?
6.5 What is your plan to handle the transition of care between the ED and admitting unit?
6.6 What is your plan to handle the shift-to-shift transition of care between nursing staff?
6.7 Describe your plan to interface with the clinical care team physicians for orders/clinical monitoring etc.
6.8 What is your study team’s plan to monitor the bedside nurses’ activities to make sure that there is protocol adherence?
6.9 Describe how you plan to monitor the patient on a daily basis throughout the treatment period (continue/discontinue study, data pull, moving up a level on control arm SS).
6.10 Describe how your study team will be made aware of and follow up on patients with hypoglycemia who require a follow up assessment.
6.11 Describe how you will assure that subjects receive the correct diet. How do you plan to order this 60 g carbohydrate diet? Have you discussed the dietary requirements with your site’s dietician? How will the subject be instructed not to eat unauthorized snacks?
6 Version 3.2 FINAL 8-Aug-2014
6.12 What is your plan to make sure that the nurse is able to directly supervise meal compliance with protocol (i.e., timing not too early, ability to count 20 minutes for meal insulin assessment)?
6.13 How will nurses document meals?
6.14 Describe how you will transition subjects off study treatment prior to discharge.
6.15 Who will be completing the CRFs? Handling DCRs, etc.?
7 FOLLOW-UP VISITS 7.1 Describe your plan to assure availability of a blinded reviewer to conduct the mRS, NIHSS, Barthal Index, and SSQOL for both the 6 week and 90 day visits.
7.2 Who will schedule the follow-up visits and complete the rest of the data collection?
7.3 What is your plan to prevent “lost to follow-ups”?
7 Version 3.2 FINAL 8-Aug-2014
COMMENTS:
ACTIONS REQUIRED PRIOR TO START-UP
Action Date Completed 1. 2. 3.
SITE ACTIVATION
DATE APPROVED FOR ACTIVATION
MUSC NOTIFIED?
STATUS CHANGED IN WebDCU?
8