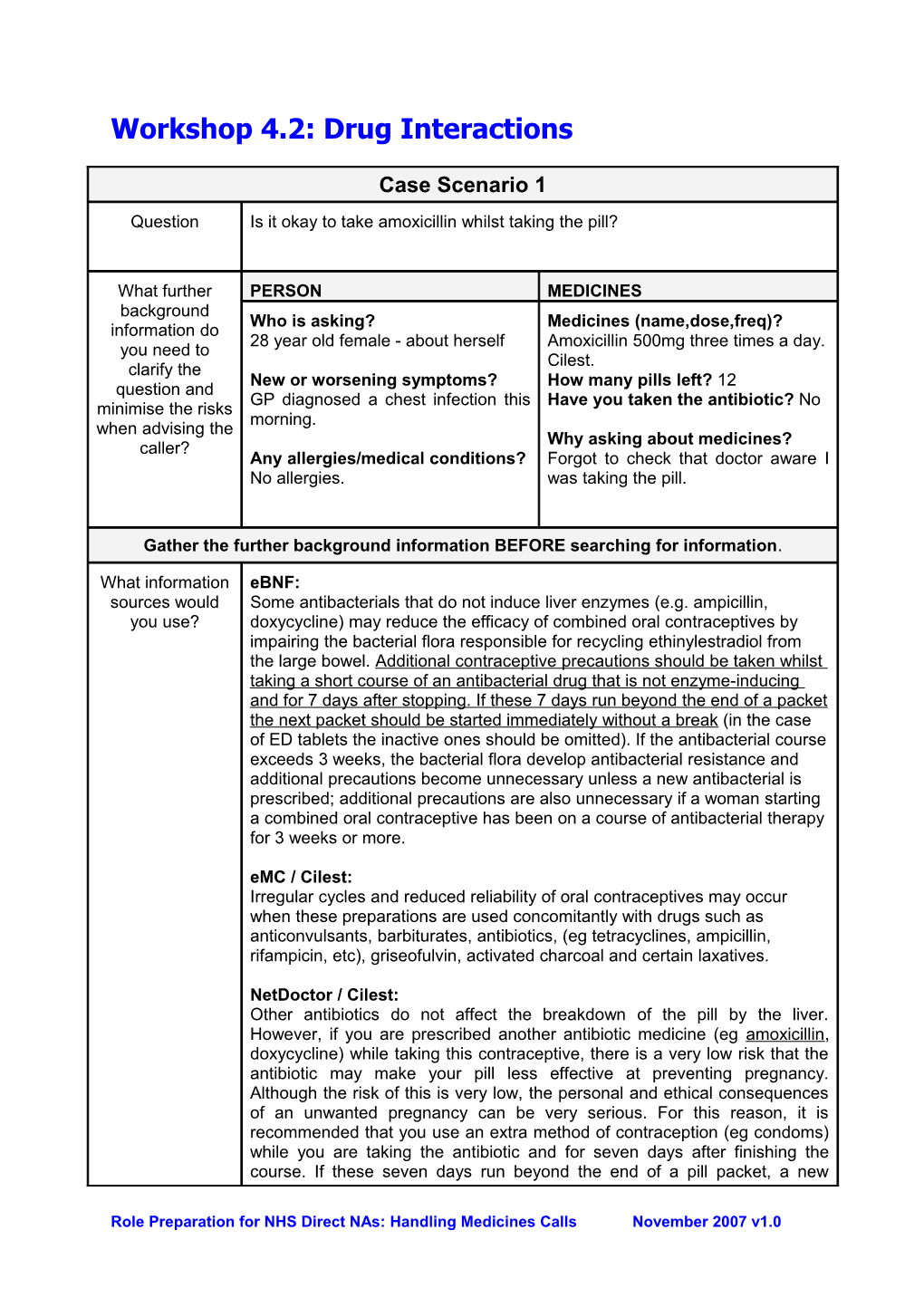
Workshop 4.2: Drug Interactions
Case Scenario 1
Question Is it okay to take amoxicillin whilst taking the pill?
What further PERSON MEDICINES background Who is asking? Medicines (name,dose,freq)? information do 28 year old female - about herself Amoxicillin 500mg three times a day. you need to Cilest. clarify the New or worsening symptoms? How many pills left? 12 question and GP diagnosed a chest infection this Have you taken the antibiotic? No minimise the risks morning. when advising the Why asking about medicines? caller? Any allergies/medical conditions? Forgot to check that doctor aware I No allergies. was taking the pill.
Gather the further background information BEFORE searching for information.
What information eBNF: sources would Some antibacterials that do not induce liver enzymes (e.g. ampicillin, you use? doxycycline) may reduce the efficacy of combined oral contraceptives by impairing the bacterial flora responsible for recycling ethinylestradiol from the large bowel. Additional contraceptive precautions should be taken whilst taking a short course of an antibacterial drug that is not enzyme-inducing and for 7 days after stopping. If these 7 days run beyond the end of a packet the next packet should be started immediately without a break (in the case of ED tablets the inactive ones should be omitted). If the antibacterial course exceeds 3 weeks, the bacterial flora develop antibacterial resistance and additional precautions become unnecessary unless a new antibacterial is prescribed; additional precautions are also unnecessary if a woman starting a combined oral contraceptive has been on a course of antibacterial therapy for 3 weeks or more.
eMC / Cilest: Irregular cycles and reduced reliability of oral contraceptives may occur when these preparations are used concomitantly with drugs such as anticonvulsants, barbiturates, antibiotics, (eg tetracyclines, ampicillin, rifampicin, etc), griseofulvin, activated charcoal and certain laxatives.
NetDoctor / Cilest: Other antibiotics do not affect the breakdown of the pill by the liver. However, if you are prescribed another antibiotic medicine (eg amoxicillin, doxycycline) while taking this contraceptive, there is a very low risk that the antibiotic may make your pill less effective at preventing pregnancy. Although the risk of this is very low, the personal and ethical consequences of an unwanted pregnancy can be very serious. For this reason, it is recommended that you use an extra method of contraception (eg condoms) while you are taking the antibiotic and for seven days after finishing the course. If these seven days run beyond the end of a pill packet, a new
Role Preparation for NHS Direct NAs: Handling Medicines Calls November 2007 v1.0 packet should be started without a break. For more information talk to your pharmacist.
If you are prescribed an antibiotic for longer than three weeks, eg for treating acne, then you don't need to use extra contraception after you have been taking that antibiotic for three weeks or longer. But, if you are then also prescribed a short course of a different antibiotic, you will need to use extra contraception again, as above. For more information talk to your pharmacist.
Medicines Complete - Stockley: The oral contraceptive / penicillin interaction is inadequately established and controversial. The total number of failures is extremely small. However, the personal and ethical consequences of an unwanted pregnancy can be very serious. For this reason the general advice is that a second (barrier) method of contraception be used whilst taking the penicillin and for 7 days after finishing the course. The FPA recommend that if the 7 days run beyond the end of the packet then the new packet should be started without a pill-free break.
What advice There is a risk that amoxicillin may stop the pill from working properly. would you give? Advise to use a barrier method during the time that she is on the antibiotic Or would you and for 7 days following the end of the course (i.e. 14 days). refer? As there are only 12 tablets left in the pack, start the next pack of pills straight away without the 7-day pill free period. Explain that this is safe and that she will not get the usual withdrawal bleed.
Further learning points For questions about the contraceptive pill Ask how many pills are left in the pack Ask if the second medicine has already been taken. May need to assess the risk of contraceptive failure.
Role Preparation for NHS Direct NAs: Handling Medicines Calls November 2007 v1.0 Workshop 4.2: Drug Interactions
Case Scenario 2
Question I have just been to see my doctor. He has given me some ciprofloxacin. I am taking warfarin. Is it ok to take them together?
What further PERSON MEDICINES background Who is asking? Medicines (name,dose,freq)? information do 61-year old female - about herself. Warfarin 3mg once a day. you need to Ciprofloxacin 500mg twice a day for clarify the New or worsening symptoms? 1 week. question and Doctor has diagnosed a urinary tract minimise the risks infection. Why asking about medicines? when advising the Yellow dosing book warns about caller? Any allergies or medical taking other medicines with warfarin. conditions? No allergies. DVT 3 months ago. Gather the further background information BEFORE searching for information.
What information eBNF: sources would ciprofloxacin + coumarins - potentially hazardous you use? ciprofloxacin enhances anticoagulant effect of coumarins Change in patient's clinical condition, particularly associated with liver disease, intercurrent illness, or drug administration, necessitates more frequent testing. Major changes in diet (especially involving salads and vegetables) and in alcohol consumption may also affect anticoagulant control
eMC- SPC / Ciproxin®: Prolongation of bleeding time has been reported during concomitant administration of ciprofloxacin and oral anti-coagulants. eMC- PIL / Ciproxin®: Remind your doctor if you are taking drugs that thin the blood (anticoagulants) such as warfarin
NetDoctor Ciprofloxacin may enhance the anti-blood-clotting effect of anticoagulant medicines such as warfarin. As this may increase the risk of bleeding, your blood clotting time (INR) should be monitored more frequently if you are taking ciprofloxacin with an anticoagulant. What advice Ciprofloxacin can in some people enhance the effects of warfarin. This would you give? means it can make your blood too thin and increase the risk of bleeding.
Or would you Suggest you phone your GP. He may want to change your antibiotic or refer? monitor your blood more closely.
Signs that your blood is too thin include nosebleeds, easily bruising and blood in the urine. If these occur, speak to your GP immediately.
Role Preparation for NHS Direct NAs: Handling Medicines Calls November 2007 v1.0 Further learning points Warfarin is a narrow therapeutic range drug small increases in blood level can lead to haemorrhage including stroke small decreases in blood level can result in blood clots (stroke, DVT, PE) Ciprofloxacin inhibits the metabolism of many medicines.
Role Preparation for NHS Direct NAs: Handling Medicines Calls November 2007 v1.0 Workshop 4.2: Drug Interactions
Case Scenario 3
Question Is it OK to take Nurofen® with my yellow tablets?
What further PERSON MEDICINES background Who is asking? Medicines (name, dose, freq)? information do 50 yr old man about himself. Methotrexate 7.5mg weekly as 3 x you need to 2.5mg tablets clarify the New or worsening symptoms? Nurofen® Liquid Capsules question and Have a really bad sore throat. minimise the Why taking? risks when Any allergies or medical Have had Rheumatoid Arthritis for advising the conditions? past 5 years. caller? No allergies.
Gather the further background information BEFORE searching for information.
What information MedicinesChest: sources would Nurofen® Liquid Capsules soft capsule containing: you use? Ibuprofen 200 mg
eBNF: methotrexate + ibuprofen - potentially hazardous Excretion of methotrexate reduced by ibuprofen (increased risk of toxicity)— but for concomitant use in rheumatic disease see Methotrexate, section 10.1.3 Aspirin and other NSAIDs If aspirin or other NSAIDs are given concurrently the dose of methotrexate should be carefully monitored. Patients should be advised to avoid self-medication with over-the-counter aspirin or ibuprofen. Important The dose for methotrexate is a weekly dose. To avoid error with low-dose methotrexate, it is recommended that: the patient is carefully advised of the dose and frequency and the reason for taking methotrexate and any other prescribed medicine (e.g. folic acid); only one strength of methotrexate tablet (usually 2.5 mg) is prescribed and dispensed. the prescription and the dispensing label clearly show the dose and frequency of methotrexate administration; the patient is warned to report immediately the onset of any feature of blood disorders (e.g. sore throat, bruising, and mouth ulcers), liver toxicity (e.g. nausea, vomiting, abdominal discomfort, and dark urine), and respiratory effects (e.g. shortness of breath).
eMC - SPC: Maxtrex® Interaction with other medicinal products and other forms of interaction Methotrexate dosage should be monitored if concomitant treatment with NSAIDs is commenced, as concomitant use of NSAIDs has been associated
Role Preparation for NHS Direct NAs: Handling Medicines Calls November 2007 v1.0 with fatal methotrexate toxicity.
Patients should report all symptoms and signs suggestive of infection, especially sore throat. eMC – PIL: Maxtrex® Check with your doctor before taking any other medications including any you have bought without a prescription in particular: NSAIDs (non-steroidal anti-inflammatory drugs) e.g. ibuprofen, indometacin or aspirin (for pain relief or inflammation), antibiotics (chloramphenicol, penicillin, sulphonamides, co-trimoxazole, trimethoprim and tetracyclines), thiazides (a group of diuretics for fluid retention), hypoglycaemics (for lowering blood sugar levels), p-aminobenzoic acid, acritretin (treatment for psoriasis or skin disorders), diphenylhydantoins (for epilepsy), probenicid, sulphinapyrazone (used to treat gout), phenytoin (an antiepileptic), including vitamin preparations containing folic acid or its derivatives, and non-prescription remedies, or receiving the anaesthetic gas nitrous oxide.
Methotrexate can make you more likely to catch infections. If you think you have an infection, a sore throat, fever, chills, or achiness during treatment you should tell your doctor immediately.
NetDoctor: Salicylate medicines such as aspirin, and non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen, ketoprofen and diclofenac can reduce the removal of methotrexate from the body. This can cause levels of methotrexate can build up in the blood, increasing the risk of side effects. For this reason, people taking methotrexate should avoid buying aspirin or NSAIDs such as ibuprofen to take as painkillers or anti-inflammatories. These medicines should only be used on the advice of the doctor who is monitoring your methotrexate treatment, so that changes can be made to your methotrexate dose if necessary.
This medicine may rarely cause a decrease in the normal amounts of blood cells in the blood. For this reason you should consult your doctor immediately if you experience any of the following symptoms: unexplained bruising or bleeding, purple spots, sore throat, mouth ulcers, high temperature (fever), feeling tired or general illness. Your doctor may want to take a blood test to check your blood cells.
What advice Patients taking Methotrexate should only be taken ibuprofen under the would you give? supervision of their doctor. Or would you refer? Sore throat symptoms may be a sign of a serious blood disorder. The patient should see the doctor as soon as possible for tests. Further learning points Methotrexate is a type of medicine called a cytotoxic antimetabolite. Methotrexate is used to treat three different conditions: rheumatoid arthritis, psoriasis and cancer of various types.
Treatment with methotrexate is usually only initiated by hospital specialists, and regular blood tests are needed to monitor for potential side effects.
Role Preparation for NHS Direct NAs: Handling Medicines Calls November 2007 v1.0