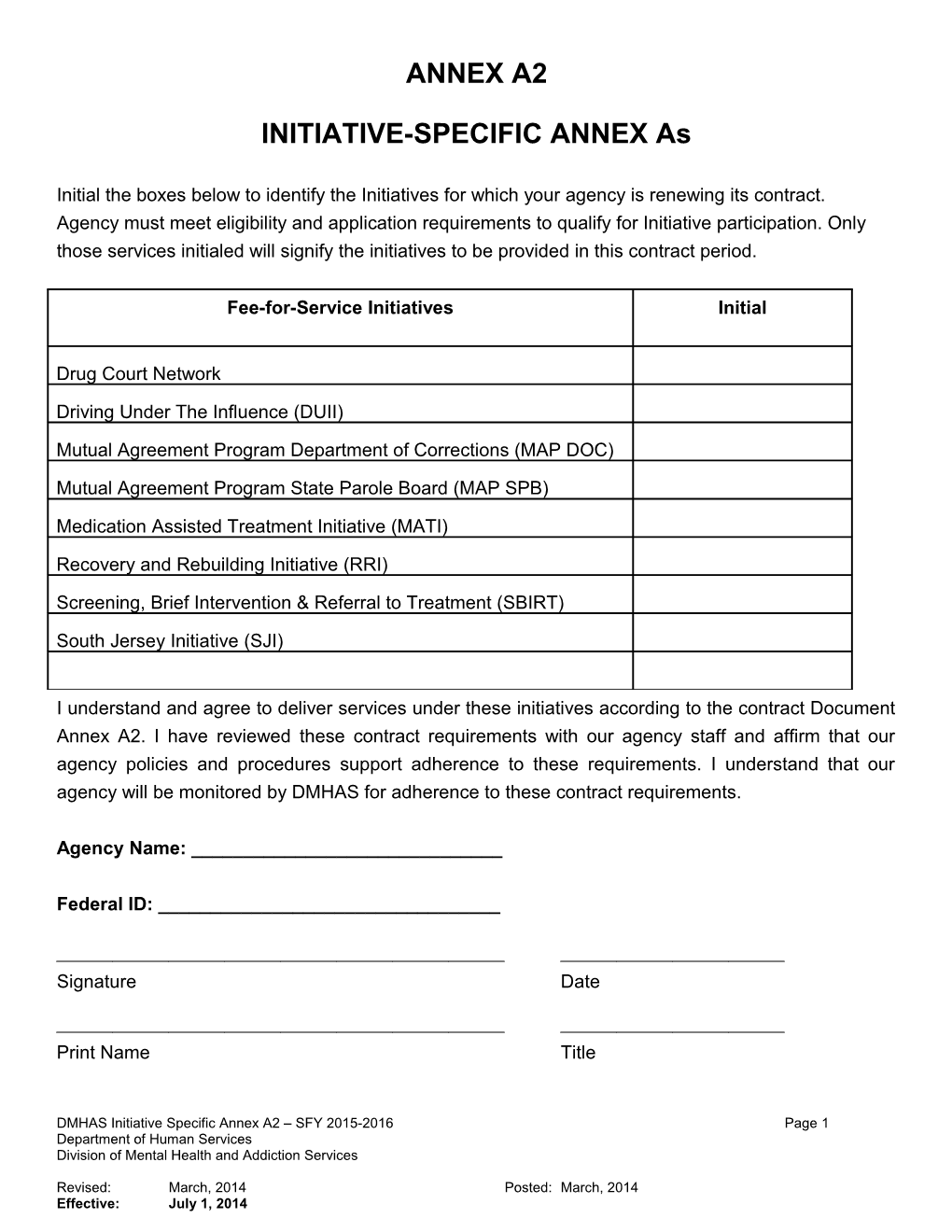
ANNEX A2
INITIATIVE-SPECIFIC ANNEX As
Initial the boxes below to identify the Initiatives for which your agency is renewing its contract. Agency must meet eligibility and application requirements to qualify for Initiative participation. Only those services initialed will signify the initiatives to be provided in this contract period.
Fee-for-Service Initiatives Initial
Drug Court Network
Driving Under The Influence (DUII)
Mutual Agreement Program Department of Corrections (MAP DOC)
Mutual Agreement Program State Parole Board (MAP SPB)
Medication Assisted Treatment Initiative (MATI)
Recovery and Rebuilding Initiative (RRI)
Screening, Brief Intervention & Referral to Treatment (SBIRT)
South Jersey Initiative (SJI)
I understand and agree to deliver services under these initiatives according to the contract Document Annex A2. I have reviewed these contract requirements with our agency staff and affirm that our agency policies and procedures support adherence to these requirements. I understand that our agency will be monitored by DMHAS for adherence to these contract requirements.
Agency Name: ______
Federal ID: ______
Signature Date
Print Name Title
DMHAS Initiative Specific Annex A2 – SFY 2015-2016 Page 1 Department of Human Services Division of Mental Health and Addiction Services
Revised: March, 2014 Posted: March, 2014 Effective: July 1, 2014 ANNEX A2
DRUG COURT NETWORK
Drug Court Program Summary
Piloted in 1996 and implemented statewide in 2004, the mission of the Drug Courts (DC) is to stop the abuse of alcohol and other drugs and related criminal activities. Drug Court programs are rigorous, requiring intensive supervision based on frequent drug testing and court appearances, along with tightly structured regimens of treatment and recovery services. This level of supervision permits the program to actively support the recovery process and react swiftly to impose appropriate therapeutic sanctions or to reinstate criminal proceedings when participants cannot comply with the program. Approval to provide services to DC participants is predicated on an agency's ability and agreement to adhere to the following:
Participating providers agree to cooperate with the monitoring requirements of DMHAS, the Administrative Office of the Courts (AOC) and the vicinages of the New Jersey Superior Court Drug Court Personnel, which includes site visits, on-site review of case files, billing/fiscal records and interviews of staff and clients to insure compliance with Drug Court procedures.
Contract Specific Requirements
In addition to the General Service Requirements stated in the Division of Mental Health and Addiction Services (DMHAS) Standard FFS Network Annex A, the Drug Court contractee shall comply with the following Drug Court specific requirements:
1. No paid or volunteer staff involved in the criminal justice system has authority over or access to any Drug Court client’s confidential information including, but not limited to, clinical reports, records and information disclosed in individual, group, family sessions or community meetings.
2. DMHAS and the referring Drug Court shall be notified in writing of clients’ program admission denials which includes referrals to a more suitable level of care. 3. All Drug Court primary counselors shall adhere to the Division of Consumer Affairs, State Board of Marriage and Family Therapy Examiners Alcohol and Drug Counselor Committee regulations regarding the practice of alcohol and drug counseling including the requirements for counselor interns. 4. All Drug Court primary counselors and any clinical staff assigned to conduct substance use evaluations shall receive training in ASAM and the completion and clinical justification of the LOCI. DMHAS Initiative Specific Annex A2 – SFY 2015-2016 Page 2 Department of Human Services Division of Mental Health and Addiction Services
Revised: March, 2014 Posted: March, 2014 Effective: July 1, 2014 ANNEX A2
Such training and staff competency in the area shall be evaluated annually and documented in the staff’s personnel file.
5. All non-clinical staff who has contact with Drug Court clients shall receive an orientation on Drug Court mandates.
6. Staff attendance is required at court staffing sessions and client court appearances.
7. The contractee shall maintain a Drug Court referral waiting list for those individuals who cannot be served immediately; the waiting list shall be maintained for all levels of care that the contractee is approved to provide services. a. The contractee shall ensure that referrals from Drug Court vicinages and subsequent admissions shall be based upon the order received. b. The contractee shall notify drug courts and document circumstances under which the waiting list order is not adhered to for a particular participant: such general reasons shall be made part of the waiting list policy. c. The contractee shall provide to the Drug Courts the status of the waiting list on a monthly basis.
8. The contractee shall complete monthly Drug Court reports for residential programs and weekly Drug Court reports for non-residential programs in accordance with vicinage specific requirements.
9. The contractee shall notify the referring Drug Court and DMHAS regarding client nonadherence to treatment and Drug Court program requirements within 2 hours of any relevant incident. If a client absconds, it must be reported immediately.
10.Discharge planning shall begin at admission and include client’s probation officer so that housing and continued care needs can be addressed throughout the course of treatment.
11.The Contractee shall include agency name, contact number and e-mail on all correspondence sent to the referring Drug Court and to DMHAS.
12. The contractee shall maintain in the client file documentation of case management efforts in
DMHAS Initiative Specific Annex A2 – SFY 2015-2016 Page 3 Department of Human Services Division of Mental Health and Addiction Services
Revised: March, 2014 Posted: March, 2014 Effective: July 1, 2014 ANNEX A2
the acquisition of prescription insurance for individuals utilizing the reimbursable provision of physical and psychotropic medication. Agencies are permitted to reimburse for 60 days of psychotropic and physical medication per episode of treatment at the actual cost of medication. This provision may be altered or revoked at the discretion of the Administrative Office of the Courts (AOC) and the vicinages of the New Jersey Superior Court Drug Court Personnel or the Division of Mental Health and Addiction Services. Requests for prescription reimbursement are submitted to the Drug Court Initiative program manager.
DMHAS Initiative Specific Annex A2 – SFY 2015-2016 Page 4 Department of Human Services Division of Mental Health and Addiction Services
Revised: March, 2014 Posted: March, 2014 Effective: July 1, 2014 ANNEX A2
DRIVING UNDER THE INFLUENCE INITIATIVE (DUII)
Driving Under the Influence Initiative Program Summary
Implemented in November 2005, the Driving Under the Influence initiative (DUII) supports treatment services for individuals convicted of Driving Under the Influence and who meet financial and program eligibility as set by the Division of Mental Health and Addiction Services (DMHAS).
Contract Specific Requirements
In addition to the General Service Requirements stated in the DMHAS FFS Standard Network Agreement Annex A, the DUII Contractee shall comply with the following DUII requirements:
1. Affiliation and network requirements:
a. All treatment contractees shall be affiliated through the Affiliation Agreement Process as defined in New Jersey Administrative Code 10:162-5 et seq. , New Jersey Statute 39:4-50 (NJ Statutes annotated version as per State Law Library).
i. Outpatient Contractees shall be affiliated with the referring County Intoxicated Driver Resource Center (IDRC).
ii. All DMHAS licensed residential programs will be affiliated with the DMHAS Intoxicated Driving Program (IDP).
b. All Affiliated Contractees shall comply with N.J.A.C. 10:162-5 et seq.
2. Initiative eligibility guidelines:
a. Clients shall have a DUI conviction on or after October 17, 2005.
b. Clients shall be a resident of New Jersey.
c. Clients shall have proof of income less than 350% of the Federal Poverty Level (FPL).
DMHAS Initiative Specific Annex A2 – SFY 2015-2016 Page 5 Department of Human Services Division of Mental Health and Addiction Services
Revised: March, 2014 Posted: March, 2014 Effective: July 1, 2014 ANNEX A2
3. The following documents shall be reviewed as part of the assessment process and retained in the client’s chart: • SI-AOD Screening Tool • Driving History Report/notes • Lifetime drug and alcohol driving offenses • Blood Alcohol Content Report • History of addiction treatment • Outside/Family information report • Underage driving/alcohol offenses • IDRC Interviewer notes • Records release
4. DUII Treatment Requirements: The treatment contractee agrees to schedule the client for an intake/assessment within 30 days of referral from the IDRC. If the client cannot be scheduled within 30 days, client will be directed back to the referring IDRC in order that another treatment referral may be obtained. DUII clients should not be placed on a waiting list before treatment can commence. All documentation shall be reported in NJSAMS.
5. Urine Drug Screens: The treatment contractee shall ensure that all clients will be randomly screened for alcohol and other drug use. Results are to be documented in NJSAMS monthly report.
6. Reporting for IDRC Clients: The treatment contractee shall utilize the NJSAMS ASI and LOCI and all other reporting requirements of the NJSAMS IDRC reporting module in accordance with N.J.A.C. 10:162-6
7. All DUII funded consumers must be connected to an IDRC/IDP for monitoring purposes. All DUII funded consumers must have monthly reports completed in NJSAMS in order to ensure IDRC/IDP monitoring.
8. The contractee shall meet agency criteria to participate in the co-occurring network and have demonstrated readiness to provide integrated care for dually diagnosed client. New contractees must submit a co-occurring application no later than 60 days following the execution of their new FFS contract.
DMHAS Initiative Specific Annex A2 – SFY 2015-2016 Page 6 Department of Human Services Division of Mental Health and Addiction Services
Revised: March, 2014 Posted: March, 2014 Effective: July 1, 2014 ANNEX A2
MUTUAL AGREEMENT PROGRAM – DEPARTMENT OF CORRECTIONS (MAP DOC)
Mutual Agreement Program Department of Corrections Program Summary
The Mutual Agreement Program (MAP) was implemented in 1984 as a cooperative effort between the New Jersey State Parole Board (SPB), Department of Corrections (DOC) and the Department of Human Services, Division of Mental Health and Addiction Services (DHS DMHAS). The goal of the MAP program is to afford the opportunity of community based substance use treatment as a special condition of parole for the NJDOC inmates who otherwise might not achieve parole status.
MAP DOC agencies are licensed residential fee-for-service substance use treatment programs located throughout the state of New Jersey. These facilities provide a highly structured environment, which introduces intensive therapy for behavioral and psychological problems related to addiction.
Contract Specific Requirements
In addition to the General Service Requirements stated in the Division of Mental Health and Addiction Services (DMHAS) Standard FFS Network Annex A, the Mutual Agreement Program Department of Corrections (MAP DOC) network contractee shall comply with the following MAP DOC requirements:
1. No paid or volunteer staff actively involved in the criminal justice system can have authority over or access to any MAP DOC client’s confidential information including but not limited to, clinical reports, records and information disclosed in individual, group and family sessions or community meetings.
2. Contractee shall identify and maintain at least one staff person to coordinate MAP DOC services. This staff person shall act as a liaison with the DOC and DMHAS’ MAP Coordinator regarding all MAP DOC issues and concerns.
3. In addition to DMHAS Licensure Standards regarding Reportable Events, MAP DOC network contractee shall ensure that their facility’s policy and procedures manual include and adhere to the following:
DMHAS Initiative Specific Annex A2 – SFY 2015-2016 Page 7 Department of Human Services Division of Mental Health and Addiction Services
Revised: March, 2014 Posted: March, 2014 Effective: July 1, 2014 ANNEX A2
a. The manner by which immediate notification is made to DOC of any incidents which require a parolee be discharged from the program and returned to the jurisdiction of the Department of Corrections. Such incidents might include any disciplinary action that requires the inmate be removed from the program, and should include how written notification will be provided to the DOC as well as including a copy of the incident report and discharge summary, as applicable.
b. Written notification will be provided to the DOC including a copy of the incident report regarding problematic client behaviors in any instance where a DOC client is found to be in possession of illegal substances or items (e.g., drugs, paraphernalia, weapons, etc.).
c. Internal agency policy regarding inmate walkaways or escapes utilizing components from N.J.A.C. 10A:20-4.39.
4. The contractee shall provide weekly MAP DOC client rosters electronically to DMHAS’ Criminal Justice Unit MAP Coordinator and DOC evaluator by close of business each Friday. The agency must also submit a daily roster to the DOC evaluator by 7am following each business day.
5. Contractee shall ensure bed availability for DOC referrals once admission confirmation is given to DOC. Within 7 days of receiving a referral from DOC, contractee will provide written confirmation to the Department of Corrections with a determination if a referral will be accepted.
6. DMHAS MAP DOC network contractee shall assist clients in obtaining prescribed medications that are required beyond the two week supply provided by prisons at time of release.
7. Contractee shall participate in meetings/trainings as requested by DMHAS.
DMHAS Initiative Specific Annex A2 – SFY 2015-2016 Page 8 Department of Human Services Division of Mental Health and Addiction Services
Revised: March, 2014 Posted: March, 2014 Effective: July 1, 2014 ANNEX A2
MUTUAL AGREEMENT PROGRAM – STATE PAROLE BOARD (MAP SPB)
Mutual Agreement Program State Parole Board Program Summary
The Mutual Agreement Program (MAP) was implemented in 1984 as a cooperative effort between the New Jersey State Parole Board (SPB), Department of Corrections (DOC) and the Department of Human Services, Division of Mental Health and Addiction Services (DHS DMHAS). The goal of the MAP program is to provide the opportunity for substance use disorder treatment to SPB parolees as required under special conditions of parole, for the purpose of reducing the likelihood of returning back to criminal behavior.
MAP SPB agencies are licensed substance use treatment programs located throughout the state of New Jersey. These facilities provide a highly structured environment that provides intensive therapy for behavioral and psychological problems related to addiction.
Contract Specific Requirements
In addition to the General Service Requirements stated in the Division of Mental Health and Addiction Services (DMHAS) Standard FFS Network Annex A, the Mutual Agreement Program State Parole Board (MAP SPB) contractee shall comply with the following MAP SPB requirements:
1. No paid or volunteer staff involved in the criminal justice system can have authority over or access to any SPB client’s confidential information but not limited to, clinical reports, records and information disclosed in individual, group and family sessions or community meetings.
2. Contractee shall identify and maintain at least one staff person to coordinate MAP SPB services. This staff person shall act as a liaison with SPB and DMHAS’ Criminal Justice Unit’s MAP Coordinator regarding MAP SPB issues.
3. In addition to DMHAS Licensure Standards regarding Reportable Events, MAP SPB Network contractee shall ensure that their facility’s policy and procedures manual include and adhere to the following:
DMHAS Initiative Specific Annex A2 – SFY 2015-2016 Page 9 Department of Human Services Division of Mental Health and Addiction Services
Revised: March, 2014 Posted: March, 2014 Effective: July 1, 2014 ANNEX A2
a. The components of the September 26, 2013 New Jersey State Parole Board memorandum regarding the Abscond Reporting Procedures. Such incidents might include a parolee absconding or any disciplinary action that requires the parolee to be removed from the program. b. How problematic client behaviors will be reported to SPB in any instance where an SPB client is found to be in possession of illegal substances or items (e.g., drugs, paraphernalia, weapons, etc.) or when removal of a parolee from the program is required.
4. For Residential Programs only: Provide electronic rosters to the DMHAS’ Criminal Justice Unit MAP Coordinator and SPB Coordinator by close of business each Friday. Contractee will provide written electronic notification on all parolee program arrivals as well a program discharges.
5. Within 7 days of receiving a referral from SPB, contractee will provide written confirmation to the SPB whether the referral will be accepted.
6. Prescription Reimbursement: The contractee shall maintain in the client file documentation of case management efforts in the acquisition of prescription insurance for individuals utilizing the reimbursable provision of psychotropic medication. Contractee is permitted to reimburse for 60 days of psychotropic medication per episode of treatment at the actual cost of medication. This provision may be altered or revoked at the discretion of the State Parole Board and the Division of Mental Health and Addiction Services. Requests for prescription reimbursement are submitted to the MAP SPB program manager.
7. Contractee shall participate in meetings/trainings as requested by DMHAS.
DMHAS Initiative Specific Annex A2 – SFY 2015-2016 Page 10 Department of Human Services Division of Mental Health and Addiction Services
Revised: March, 2014 Posted: March, 2014 Effective: July 1, 2014 ANNEX A2
MEDICATION ASSISTED TREATMENT INITIATIVE (MATI)
Medication Assisted Treatment Initiative Program Summary
Through funding legislated through the Bloodborne Disease Harm Reduction Act, the Division of Mental Health and Addiction Services (DMHAS) has developed the Medication Assisted Treatment Initiative (MATI). This initiative funds medication assisted treatment for indigent New Jersey residents with an opiate addiction, while also offering outreach, office-based services and case management, as well as the opportunity for supportive housing, sub-acute enhanced medically managed detoxification, authorizations for other treatment services, and an evaluation of the project.
In order for clients to attain services through the MATI, individuals must meet requirements set-forth in both the MATI Eligibility Criteria and DMHAS Income Eligibility Policy. If a client requires another level of care or support service not provided via the mobile unit or office-based program, the client may be eligible for an authorization through the MATI FFS Network, which would enable a client to receive services through one of the MATI Network Providers.
Contract Specific Requirements
In addition to the General Service Requirements stated in the Division of Mental Health and Addiction Services (DMHAS) Standard FFS Network Annex A, the Medication Assisted Treatment Initiative (MATI) contractee shall comply with the following MATI specific requirements:
1. The contractee will provide treatment services in accordance with the MATI service descriptions and comply with all State regulations/mandates.
2. The contractee will accept MATI clients within 24 hours or provide an appropriate referral.
3. The contractee will appoint appropriate staff to participate in monthly or bi-monthly consortium meetings, as well as attend any meetings/trainings requested by DMHAS.
4. The contractee agrees to coordinate with case management services provided by the mobile van/office-based services.
DMHAS Initiative Specific Annex A2 – SFY 2015-2016 Page 11 Department of Human Services Division of Mental Health and Addiction Services
Revised: March, 2014 Posted: March, 2014 Effective: July 1, 2014 ANNEX A2
5. The contractee agrees to accept the physical exam completed at the mobile van/office-based services to fulfill requirement for a physical exam at admission.
6. The contractee shall maintain policies and procedures to ensure non-discrimination towards clients who choose to utilize medication-assisted treatment to support their recovery.
7. The contractee shall adhere to all prior authorization procedures established by DMHAS.
8. The contractee shall meet agency criteria to participate in the co-occurring network and have demonstrated readiness to provide integrated care for dually diagnosed client. New contractees must submit a co-occurring application no later than 60 days following the execution of their new FFS contract.
DMHAS Initiative Specific Annex A2 – SFY 2015-2016 Page 12 Department of Human Services Division of Mental Health and Addiction Services
Revised: March, 2014 Posted: March, 2014 Effective: July 1, 2014 ANNEX A2
RECOVERY AND REBUILDING INITIATIVE
Recovery and Rebuilding Initiative Program Summary
The Recovery and Rebuilding Initiative (RRI) is funded through federal Supplemental Social Services Block Grant (SSBG) resources that have been made available to the New Jersey Department of Human Services to support its disaster recovery and response efforts in the aftermath of Superstorm Sandy. The RRI is designed to increase access and capacity for substance use disorder treatment services for consumers living in one of the ten significantly storm-impacted New Jersey counties (Atlantic, Bergen, Cape May, Cumberland, Essex, Hudson, Middlesex, Monmouth, Ocean, and Union) between the dates of October 28-30, 2012.
Participating RRI Treatment Network providers must be licensed by the NJ Department of Human Services, Office of Licensure to provide co-located detoxification and short-term residential services under the Standards for Licensure of Residential Substance Use Disorder Treatment Facilities at N.J.A.C. 10:161 A. As RRI funding will be tracked and reported separately from other DMHAS funding, each approved agency agrees to cooperate with all monitoring activities conducted by DMHAS, including site visits, on-site review of case files, review of billing/fiscal records, interviews of staff and consumers, and data collection and reporting requirements to ensure compliance with DMHAS and to identify potential vulnerabilities in both compliance and transparency.
Contract-Specific Requirements
In addition to the General Service Requirements stated in the DMHAS Standard FFS Network Annex A, the RRI Treatment Network contractee shall comply with the following initiative-specific requirements:
1. Eligibility:
To be eligible for services available through the RRI, consumers must:
a. Be a United States citizen or legal resident;
b. Be 18 years of age or older;
c. Have been living in one of the ten storm-impacted counties between October 28-30, 2012;
d. Meet ASAM criteria for Level III.7, Level III.7D or Level III.DE care.
2. Proof of United States citizenship or legal residency:
DMHAS Initiative Specific Annex A2 – SFY 2015-2016 Page 13 Department of Human Services Division of Mental Health and Addiction Services
Revised: March, 2014 Posted: March, 2014 Effective: July 1, 2014 ANNEX A2
Proof of United States citizenship or legal residency must be documented in the consumer’s file upon admission. A copy of at least one of the following credentials displaying the name of the consumer must be retained in the consumer’s file:
a. Current NJ digital driver license;
b. Current NJ digital non-driver ID card;
c. Current NJ digital boat license;
d. Active duty US military photo identification card;
e. Original or certified copy of civil birth certificate;
f. US Department of State birth certificate;
g. US Passport, current or expired less than three years;
h. Current US passport card;
i. Consular registration of birth abroad certificate;
j. Certificate of citizenship;
k. U.S. adoption papers;
l. Certificate of naturalization (Form N-550, N-570 or N-578);
m. Certificate of citizenship (Form N-560, N-561 or N-645);
n. Foreign passport with INS or USCIS verification and valid record of arrival/departure (Form I-94);
o. Foreign passport with INS or USCIS verification and valid Form I-551 stamp;
p. Current alien registration card (new Form I-551) with expiration date and verification from INS or USCIS;
q. Refugee travel document (Form I-571);
r. US re-entry permit (Form I-327);
s. Valid I-94 stamped “Refugee,” “Parolee,” “Asylee” or “Notice of Action” (Form I-797 approved petition) by INS or USCIS;
t. Valid I-94 with attached photo stamped “Processed for I-551…” by INS or USCIS.
DMHAS Initiative Specific Annex A2 – SFY 2015-2016 Page 14 Department of Human Services Division of Mental Health and Addiction Services
Revised: March, 2014 Posted: March, 2014 Effective: July 1, 2014 ANNEX A2
3. Proof of Residence:
Proof of residence in a storm-impacted county must be documented in the consumer’s file at the time of admission. A copy of at least one of the following credentials displaying the name of the consumer and a valid street address (P.O. Boxes are not acceptable) must be retained in the consumer’s file:
a. New Jersey driver’s license issued before October 28, 2012;
b. United States passport issued before October 28, 2012;
c. School records showing an address for the period between October 28-30, 2012;
d. Utility bill for services between October 28-30, 2012;
e. Credit card bill for the period between October 28-30, 2012;
f. Bank or credit union statement, with account numbers redacted, for services between October 28-30, 2012;
g. 2012 state or federal tax return;
h. Lease or rental agreement effective between October 28-30, 2012;
i. Shelter records of housing between October 28-30, 2012;
j. Property tax bill, statement, record or receipt between October 28-30, 2012;
k. Signed attestation from a community social service provider, on agency letterhead, of the consumer’s residence between October 28-30, 2012;
l. Signed attestation from a community social service provider, on agency letterhead, of the consumer’s residence between October 28-30, 2012.
4. Alternative Proof of Residence:
a. If none of the credentials listed in 3, above, are available, the consumer may provide a signed attestation of residence for the period October 28-30, 2012; which explains why no other credential is available. The original signed attestation must be retained in the consumer’s file.
5. Payer of Last Resort:
DMHAS Initiative Specific Annex A2 – SFY 2015-2016 Page 15 Department of Human Services Division of Mental Health and Addiction Services
Revised: March, 2014 Posted: March, 2014 Effective: July 1, 2014 ANNEX A2
a. Federal funding for treatment services provided to RRI consumers must be accessed as the payer of last resort. Participating treatment contractee must document the income and program eligibility status of all consumers who may be eligible for the RRI using the NJSAMS DASIE module;
b. RRI providers may only request authorization for services provided to eligible consumers through the RRI when all funding options have been explored and/or exhausted and no other funding is available;
c. Authorization or payment for services should be obtained from other payers, including third-party commercial or public insurance/payer, if available;
d. Consumers receiving services under the RRI must sign an attestation that indicates one of the following:
i. The consumer has no third party insurance coverage;
ii. The consumer has third party insurance coverage but services to be delivered under the RRI are not a covered benefit;
iii. The consumer has third party insurance coverage and the services to be delivered under the RRI are a covered benefit, but that coverage has been exhausted;
iv. The consumer has third party insurance coverage and the services to be delivered under the RRI are a covered benefit, but the carrier will not authorize reimbursement for the service;
1. Should authorization for reimbursement by third party coverage be provided following an appeal then the agency is required to notify the program Manager and to void all FFS claims on a per diem basis;
2. Contractee may only request payment for enhancements under the RRI when the Level of Care core service package is also funded through RRI on the same day.
e. The attestation must be signed by the consumer and the staff member who verified the information. The original must be retained in the consumer’s file;
f. Contractee may not utilize RRI funding, in whole or in part, to offset the reimbursement rate of third party insurance;
DMHAS Initiative Specific Annex A2 – SFY 2015-2016 Page 16 Department of Human Services Division of Mental Health and Addiction Services
Revised: March, 2014 Posted: March, 2014 Effective: July 1, 2014 ANNEX A2
g. In cases where consumers are programmatically eligible for FFS initiatives for which funding is unavailable at the time of admission, contractee may then utilize RRI funding (if eligibility criteria is met). Contractee is required to include a copy of the NJSAMS New Client Limits screen indicating no new client admissions are available to other initiatives with the DASIE in the treatment file to support the use of RRI funds;
h. Contractee must implement internal controls that result in assurances that all RRI funds are properly authorized, and that program expenditures are reasonable, allowable and correct;
i. Per the Governor’s Executive Order No. 125, contractors are subject to penalties, including suspension of funds, return of funds, and other actions as determined for non- compliance or illegitimate use of RRI funding.
6. Transportation:
a. Transportation is a reimbursable service under the RRI only when necessary to transfer a consumer from a hospital emergency department and/or psychiatric emergency screening center for admission to the RRI participating facility;
b. Approval to provide transportation services in the RRI initiative is based on the Program Manager’s favorable review of the contractee transportation policy/s addressing driver/staff ratio, response timeframes, monitoring of driver’s license status, safety and safe driver competencies, use of subcontract services, etc. as applicable; c. A contractee approved to provide RRI transportation shall establish affiliation agreements with community-based hospital emergency departments and/or psychiatric emergency screening centers, through which they agree to accept referrals of RRI consumers; d. A signed, dated copy of the written affiliation agreements must be on file at the agency as well as with the DMHAS Office of Care Management. At a minimum, the affiliation agreement must: i. Include the contractee’s policies and procedures for screening and approving admission to the facility; ii. Based upon bed availability at the time of screening, the contractee will transport approved consumer from a hospital emergency department and/or psychiatric emergency screening center to the treatment facility. e. Transportation reimbursement is calculated based on the round-trip mileage provided for an individual consumer admitted to a network provider directly from an affiliated emergency room or screening center;
DMHAS Initiative Specific Annex A2 – SFY 2015-2016 Page 17 Department of Human Services Division of Mental Health and Addiction Services
Revised: March, 2014 Posted: March, 2014 Effective: July 1, 2014 ANNEX A2
f. Contractee may not submit duplicate billing for multiple consumers transported during the same service period;
g. RRI contractee is required to maintain a HIPAA compliant transportation log documenting the date, destination, departure and arrival times, consumer NJSAMS number, and agency staff (driver and passenger aide) for each trip claimed under the RRI. The provider shall transmit the transportation logs electronically to the RRI Program Manager within five business days of the end of each month.
7. Rosters:
a. RRI contractee is required to submit a HIPAA-compliant roster of all individuals receiving RRI funded Medically Monitored Inpatient Detoxification Enhanced Level III.DE care to the DMHAS RRI Program Manager within 5 business days of the end of each month.
i. Roster is to include: agency address and license number, consumer NJSAMS ID#, LOC, admission date, dates of service;
ii. An additional notation should document which of the following criteria was met to justify admission into this level of care: 1) co-occurring disorder (include diagnosis); 2) pregnancy (provide approximate due date); 3) poly-addicted persons, including those addicted to benzodiazepines; (provide diagnoses) 4) may or may not be on opiate replacement therapy; 5) non–life-threatening medical condition(s) that do not require the services of an acute care hospital (provide diagnosis).
8. Coordination and collaboration with DMHAS and other Recovery and Rebuilding partners: RRI treatment contractee shall participate in meetings, trainings, community events, and other activities as requested by DMHAS as needed to support adherence to program accountability and integrity, to promote awareness of services available under the RRI, and to improve coordination of efforts among other service providers.
9. Co-occurring Network: The contractee shall meet agency criteria to participate in the co-occurring network and have demonstrated readiness to provide integrated care for dually diagnosed client. New contractees must submit a co-occurring application no later than 60 days following the execution of their new FFS contract.
DMHAS Initiative Specific Annex A2 – SFY 2015-2016 Page 18 Department of Human Services Division of Mental Health and Addiction Services
Revised: March, 2014 Posted: March, 2014 Effective: July 1, 2014 ANNEX A2
SCREENING, BRIEF INTERVENTION & REFERRAL TO TREATMENT (SBIRT)
NJ SBIRT SPECIALTY TREATMENT NETWORK
NJ SBIRT Program Summary
Implemented in February 2013, the NJ Screening, Brief Intervention and Referral to Treatment (NJ- SBIRT) Project is a federal Substance Abuse and Mental Health Services Administration (SAMHSA- funded initiative to expand the existing substance use services continuum of care by making evidence-based, risk identification and early intervention services available to reduce harmful substance use and its associated negative health consequences.
The NJ SBIRT Project is a partnership between DMHAS, the Henry J. Austin Federally Qualified Health Center (HJA), Trenton Health Team member organizations, and Rutgers University. As the lead service partner, the HJA will implement SBIRT services in a mix of several primary care and community health project sites located throughout the city of Trenton. SBIRT services will be fully integrated into existing primary care and/or emergency care services at all project sites, affording universal screening for substance use risk among all adult patients seeking medical care. All NJ SBIRT Project sites will serve as treatment referral sources for those patients identified as needing substance use assessment and/or treatment services.
DMHAS Initiative Specific Annex A2 – SFY 2015-2016 Page 19 Department of Human Services Division of Mental Health and Addiction Services
Revised: March, 2014 Posted: March, 2014 Effective: July 1, 2014 ANNEX A2
Participating NJ SBIRT Specialty Treatment Network contractee must be licensed to provide services in Mercer County by the NJ Department of Human Services, Office of Licensure, under the Standards for Licensure of Outpatient Substance Abuse Treatment Facilities at NJAC 10:161 B, and agree to cooperate with the monitoring requirements of DMHAS, including site visits, on-site review of case files, review of billing/fiscal records, and interviews of staff and consumers to ensure compliance with initiative-specific procedures.
Contract Specific Requirements
In addition to the General Service Requirements stated in the DMHAS Standard FFS Network Annex A, the NJ SBIRT Specialty Treatment Network contractee shall comply with the following NJ SBIRT specific requirements:
1. Network and Affiliation requirements:
a. All participating treatment contractee shall be affiliated with the Henry J. Austin Health Center (HJA) through which they agree to accept referral of NJ SBIRT consumers from any of the NJ SBIRT project sites located in the city of Trenton.
b. A signed, dated copy of the written affiliation agreement must be on file at the DMHAS, Office of Care Management. At a minimum, the affiliation agreement must include the specialty treatment provider agency’s policy and procedures for accepting a “warm handoff” from the NJ SBIRT project sites.
c. All participating treatment contractee shall offer NJ SBIRT referred consumers: income and program eligibility determinations; assessments; appropriate ASAM levels of outpatient care; and enhancement packages to include clinical review services; and co- occurring services.
d. If a NJ SBIRT referred consumer is assessed as needing a level of care other than outpatient or intensive outpatient, all participating treatment contractee shall offer NJ SBIRT assessed consumers a secondary referral to another licensed substance use provider for a more appropriate level of care, with notification of same to HJA through NJSAMS.
DMHAS Initiative Specific Annex A2 – SFY 2015-2016 Page 20 Department of Human Services Division of Mental Health and Addiction Services
Revised: March, 2014 Posted: March, 2014 Effective: July 1, 2014 ANNEX A2
e. It is recommended that participating treatment contractee schedule initial appointments within 2 business days of the NJ SBIRT referral.
f. Under signed, patient consent, the participating treatment provider shall document the disposition of all NJ SBIRT referred consumers in NJSAMS to facilitate follow-up by HJA, including:
i. Consumers who do not attend scheduled assessment appointments;
ii. Consumers who are assessed and admitted to treatment at the participating treatment provider agency; and
2. Consumers who are assessed and require a level of care not available at the participating provider agency, and for whom the treatment provider makes a secondary referral.NJ SBIRT Initiative consumer eligibility guidelines:
a. Consumers must:
i. Be referred from one of the NJ SBIRT Project sites in the city of Trenton operated under the HJA administrative authority ii. Be 18 years of age or older iii. Meet ASAM criteria for Level I or Level II.1 outpatient care
b. Federal funding for treatment services provided to NJ SBIRT Project consumers may be accessed as the payer of last resort. Participating treatment contractee must document the income and program eligibility status of all referred NJ SBIRT consumers using the NJSAMS DASIE Plus module. Authorization or payment for services should be obtained from other payers when another payer is available.
c. NJ SBIRT Specialty Treatment Network contractee may only request authorization for services provided to eligible consumers through the NJ SBIRT FFS Initiative when no other payer is available. Payment for services authorized through the NJ SBIRT Initiative shall be accepted as payment in full.
DMHAS Initiative Specific Annex A2 – SFY 2015-2016 Page 21 Department of Human Services Division of Mental Health and Addiction Services
Revised: March, 2014 Posted: March, 2014 Effective: July 1, 2014 ANNEX A2
3. Participating treatment contractee shall participate in meetings/trainings as requested by DMHAS.
SOUTH JERSEY INITIATIVE (SJI)
South Jersey Initiative Program Summary Funded by DMHAS, the SJI began in 2001 to serve residents age 13-24 of Atlantic, Burlington, Cape May, Camden, Cumberland, Gloucester, Ocean and Salem Counties. The program was initially created to serve adolescent and young adults in the aforementioned counties until a residential treatment facility could be built. The project evolved to a full continuum of care for residents of eight southern counties between the ages of 13-24. On January 1, 2014 the initiative ceased serving the 13-17.99 year old population and is now solely dedicated to serving the 18-24 young adult population in the eight southern counties.
Contract Specific Requirements In addition to the General Service Requirements stated in the Division of Mental Health and Addiction Services (DMHAS) Standard FFS Network Annex A, the South Jersey Initiative (SJI) contractee shall comply with the following SJI specific requirements:
1. The contractee shall provide treatment services for young adults aged 18 to 24 from Atlantic, Burlington, Camden, Cape May, Cumberland, Gloucester, Ocean and Salem Counties.
2. The contractee shall complete appropriate assessments on each client specific to their age group: DMHAS Initiative Specific Annex A2 – SFY 2015-2016 Page 22 Department of Human Services Division of Mental Health and Addiction Services
Revised: March, 2014 Posted: March, 2014 Effective: July 1, 2014 ANNEX A2
a. Addiction Severity Index (ASI) for ages 18 to 24 b. All clients shall have an appropriate Level of Care Index (LOCI).
3. Urine Drug Screens: a. SJI contractee shall ensure that all clients will be screened weekly and randomly for alcohol and other drug use. b. SJI contractee shall ensure that young adults will be screened upon return from off grounds visits. c. SJI contractee shall ensure that young adults with positive urine drug screens shall receive additional individual counseling, with the focus on addressing the circumstances behind the positive urine drug screens. d. SJI contractee shall ensure that the adults treatment plan must be reviewed by the multidisciplinary team with the treatment plan revised documenting targeted interventions. 4. Clinical Services: a. The SJI contractee shall ensure that progress notes include when applicable but are not limited to: Referral(s) for other services case management related activities
5. The contractee shall meet agency criteria to participate in the co-occurring network and have demonstrated readiness to provide integrated care for dually diagnosed client. New contractees must submit a co-occurring application no later than 60 days following the execution of their new FFS contract.
DMHAS Initiative Specific Annex A2 – SFY 2015-2016 Page 23 Department of Human Services Division of Mental Health and Addiction Services
Revised: March, 2014 Posted: March, 2014 Effective: July 1, 2014