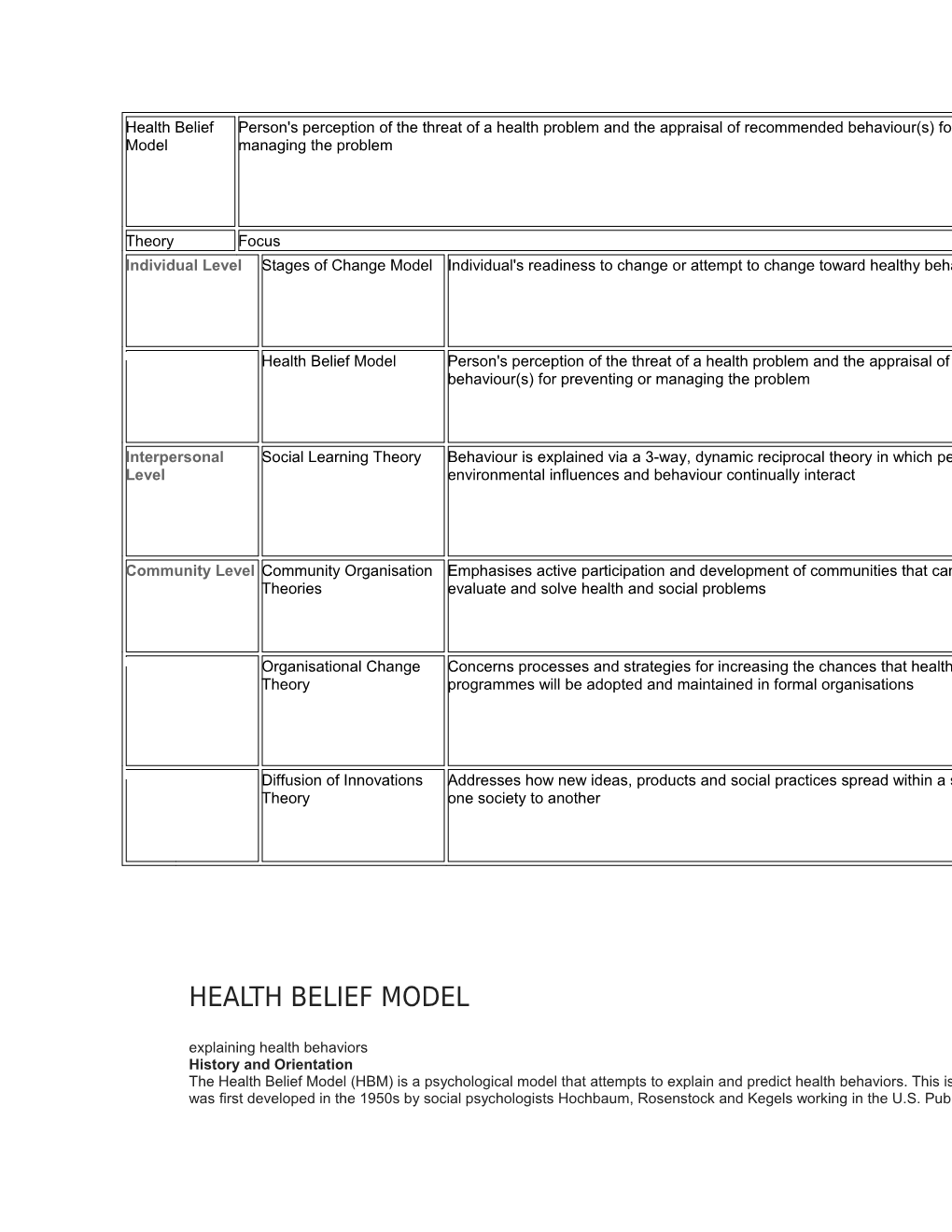
Health Belief Person's perception of the threat of a health problem and the appraisal of recommended behaviour(s) for preventing or Model managing the problem
Theory Focus Individual Level Stages of Change Model Individual's readiness to change or attempt to change toward healthy behaviours
Health Belief Model Person's perception of the threat of a health problem and the appraisal of recommended behaviour(s) for preventing or managing the problem
Interpersonal Social Learning Theory Behaviour is explained via a 3-way, dynamic reciprocal theory in which personal factors, Level environmental influences and behaviour continually interact
Community Level Community Organisation Emphasises active participation and development of communities that can better Theories evaluate and solve health and social problems
Organisational Change Concerns processes and strategies for increasing the chances that healthy policies and Theory programmes will be adopted and maintained in formal organisations
Diffusion of Innovations Addresses how new ideas, products and social practices spread within a society or from Theory one society to another
HEALTH BELIEF MODEL
explaining health behaviors History and Orientation The Health Belief Model (HBM) is a psychological model that attempts to explain and predict health behaviors. This is done by focusing on the attitudes and beliefs of individuals was first developed in the 1950s by social psychologists Hochbaum, Rosenstock and Kegels working in the U.S. Public Health Services. The model was developed in response to the failure of a free tuberculosis (TB) health screening program. Since then, the HBM has been adapted to explore a variety of long- and short-term health behaviors, including sexual risk behaviors and the transmission of HIV/AIDS. Core Assumptions and Statements The HBM is based on the understanding that a person will take a health-related action (i.e., use condoms) if that person: 1. feels that a negative health condition (i.e., HIV) can be avoided, 2. has a positive expectation that by taking a recommended action, he/she will avoid a negative health condition (i.e., using condoms will be effective at preventing HIV), and 3. believes that he/she can successfully take a recommended health action (i.e., he/she can use condoms comfortably and with confidence). The HBM was spelled out in terms of four constructs representing the perceived threat and net benefits: perceived susceptibility, barriers. These concepts were proposed as accounting for people's "readiness to act." An added concept, cues to action, addition to the HBM is the concept of self-efficacy, or one's confidence in the ability to successfully perform an action. This concept was added by Rosenstock and others in 1988 to help the HBM better fit the challenges of changing habitual unhealthy behaviors, such as being sedentary, smoking, or overeating. Table from “Theory at a Glance: A Guide for Health Promotion Practice" (1997) Concept Definition Perceived Susceptibility One's opinion of chances of getting a condition
Perceived Severity One's opinion of how serious a condition and its consequences are Perceived Benefits One's belief in the efficacy of the advised action to reduce risk or seriousness of impact Perceived Barriers One's opinion of the tangible and psychological costs of the advised action Cues to Action Strategies to activate "readiness"
Self-Efficacy Confidence in one's ability to take action Conceptual Model Source: Glanz et al, 2002, p. 52 Favorite Methods Surveys. Scope and Application The Health Belief Model has been applied to a broad range of health behaviors and subject populations. Three broad areas can be identified (Conner & Norman, 1996): 1) Preventive health behaviors, which include health-promoting (e.g. diet, exercise) and health-risk (e.g. smoking) behaviors as well as vaccination and contraceptive practices. 2) Sick role behaviors, which refer to compliance with recommended medical regimens, usually following professional diagnosis of illness. 3) Clinic use, which includes physician visits for a variety of reasons. Example This is an example from two sexual health actions. (http://www.etr.org/recapp/theories/hbm/Resources.htm) Concept Condom Use Education Example 1. Perceived Susceptibility Youth believe they can get STIs or HIV or create a Youth believe they may have been exposed to STIs or pregnancy. HIV. 2. Perceived Severity Youth believe that the consequences of getting STIs Youth believe the consequences of having STIs or HIV or HIV or creating a pregnancy are significant enoughwithout knowledge or treatment are significant enough to to try to avoid. try to avoid. 3. Perceived Benefits Youth believe that the recommended action of using Youth believe that the recommended action of getting condoms would protect them from getting STIs or tested for STIs and HIV would benefit them — possibly by HIV or creating a pregnancy. allowing them to get early treatment or preventing them from infecting others. 4. Perceived Barriers Youth identify their personal barriers to using Youth identify their personal barriers to getting tested (i.e., condoms (i.e., condoms limit the feeling or they are getting to the clinic or being seen at the clinic by someone too embarrassed to talk to their partner about it) and they know) and explore ways to eliminate or reduce these explore ways to eliminate or reduce these barriers barriers (i.e., brainstorm transportation and disguise (i.e., teach them to put lubricant inside the condom to options). increase sensation for the male and have them practice condom communication skills to decrease their embarrassment level). 5. Cues to Action Youth receive reminder cues for action in the form of Youth receive reminder cues for action in the form of incentives (such as pencils with the printed message incentives (such as a key chain that says, "Got sex? Get "no glove, no love") or reminder messages (such as tested!") or reminder messages (such as posters that say, messages in the school newsletter). "25% of sexually active teens contract an STI. one of them? Find out now"). 6. Self-Efficacy Youth confident in using a condom correctly in all Youth receive guidance (such as information on where to circumstances. get tested) or training (such as practice in making an appointment). References Key publications Conner, M. & Norman, P. (1996). Predicting Health Behavior. Search and Practice with Social Cognition Models. Open University Press: Ballmore: Buckingham. Glanz, K., Rimer, B.K. & Lewis, F.M. (2002). Health Behavior and Health Education. Theory, Research and Practice. San Fransisco: Wiley & Sons. Glanz, K., Marcus Lewis, F. & Rimer, B.K. (1997). Theory at a Glance: A Guide for Health Promotion Practice. National Institute of Health. Eisen, M et.al. (1992). A Health Belief Model — Social Learning Theory Approach to Adolescents' Fertility Control: Findings from a Controlled Field Trial. Rosenstock, I. (1974). Historical Origins of the Health Belief Model. Health Education Monographs. Vol. 2 No. 4. Becker, M.H. The Health Belief Model and Personal Health Behavior. Health Education Monographs. Vol. 2 No. 4. Champion, V.L. (1984). Instrument development for health belief model constructs, Advances in Nursing Science, 6, 73-85. Becker, M.H.,Radius, S.M., & Rosenstock, I.M. (1978). Compliance with a medical regimen for asthma: a test of the health belief model, See also: http://www.comminit.com/ctheories/sld-2929.html http://www.etr.org/recapp/theories/hbm/ See also: Theory of Planned Behavior/ Reasoned Action, Protection Motivation Theory See also Health Communication Using a Health Belief Model In Teaching Preventive Health Care Principles To Israeli RNs A Paper for Presentation at the CITA Conference University of Massachusetts Lowell November 7, 8, 9, 2002 nn K. Mackey EdD, RN Introduction The health of individuals and aggregate populations within a given community is dependent on their ability to identify their risk for specific health problem(s). In addition, these individuals and groups must be willing to adhere to life style changes in order to maintain health and wellness. Therefore, the role of nurses and other health care practitioners is to assess an individual’s health risk and his/her belief that engaging in specific risk reduction interventions could lead to healthier outcomes. The purpose of this paper is to explore instructional methods that can be utilized by faculty to teach nurses about the application of a Health Belief Model (HBM) in any health care setting. The application of teaching methods will be based upon how Israeli registered nursing students were taught HBM models or principles for implementation in their clinical practice. Before presenting specific teaching methods, the health care system in Israel, the role of nursing, and the future for nursing practice in Israel will be discussed. Overview of the Israeli Health Care System and Cultural Background The current Health Care System in Israel is a result of the National Health Insurance Law, which was enacted in 1995 and is based on principles of socialized medicine. The health care system is support by an individual health tax and funding from general tax revenues. Each citizen has a choice to belong to one of four Health Maintenance-like Organization (HMOs) or “sick funds.” These HMOs are similar to American HMOs and all citizens of Israel are required to join a sick fund. Israel’s national health law determines the types of health services or “basket of services” provided by the HMOs, the various payments the insured must pay, and how governmental appropriations will be divided among the HMOs. According to the health care law ll Israeli citizens must be provided basic health care. However, for improved access and choice, any individual who can afford it may obtain private supplemental hospitalization and health care. In each major city there are large medical centers that have the same departments that one would see in any hospital or medical center in the United States. Hadassah Hospital located in Jerusalem, an important research institution, is one of the most well known medical centers in Israel that provides health care. Israel has many cultural groups, which have led, the country in becoming a pluralistic society. The major cultural groups are Arabs and Jews, as well as Russian and Ethiopian immigrates. Within the Jewish culture are the Ultra-Orthodox Jews who have a very strong religious faith and rely on governmental support in order to live. Before any Ultra-Orthodox Jewish member can receive health care treatment, his/her spiritual leader will provide consultation and approval. Arabic and Hebrew are the principle languages, while English is an emerging language for many Israelis. Many of the medical and nursing journals are written in English so the health care practitioner must have some command of English. Role of Nursing Basic nursing education is completed through hospital based nursing programs, similar to that seen in the early development of nursing education in the United States. There are baccalaureate-nursing programs at some of the Israeli universities but enrollment is limited to students who do not have a nursing background. Nurses who are currently registered nurses (RNs) have little opportunity in obtaining a baccalaureate in nursing through Israeli universities. Therefore, nurses must obtain their nursing degrees through a United States based program that has been contracted by a private Israeli educational brokering institution. In addition, the Israeli Counsel on Higher Education must approve of the American nursing program before it can be 3 offered to Israeli RNs. Lack of approval by this counsel would result in non-recognition of the nursing degree by Israel. Currently, Israeli nurses view their role as providing treatment (nursing care) to patients in a variety of practice settings, engaging in patient health education programs, assisting physicians in carrying out medical treatment regimes, and collaborating with multi-disciplinary staff. Nurses who work in various sick funds (HMOs) help carry out physicians’ instructions and supervise patients’ progress. Hospital nurses engage in complex functions based upon patient acuity and supervise care provided by para- professional workers. Based upon student comments, within the next 5-10 years nurses in Israel would like to see nursing develop as a profession with greater respect, and that the bachelors degree will be required for entry into nursing practice. In addition, they want to become active decision makers in the health care system by having more input into the policies and strategies that relate to the delivery of health care. One student summed up her future vision of nursing by saying “nurses must become independent in initiating nursing interventions and assist patients and families to assume more responsibility for self care.” Nurses would also like to see higher salaries but recognize that the continuing violence in the country is draining to the financial resources. Nevertheless these nurses believe that a solid nursing education at the baccalaureate level will enhance the image of nursing and increase the quality of health care for all Israeli citizens. Thus, nurses become enrolled in the approved American nursing program to help actualize their vision for nursing. Instructional Preparations A required course in the American nursing program is Health Education in the Community where part of the course content is the application of a health belief model. The 4 HBM framework is presented as one of the theoretical approaches to promote and maintain a life style change that encourages health promotion, health maintenance, and assist in decreasing complications due to chronic illness. The implementation of an American based nursing program in a foreign country requires the nursing faculty to have: (a) a solid back ground in teaching and learning principles, (b) an extensive experience in academic settings, (c) expertise in the content area, (d) flexibility in presenting course content that does not compromise academic integrity, and (e) an understanding of the host country’s culture, health care system, role of nursing, and strategies used by students to engage in the process of learning. At the beginning of the Health Education course, a student questionnaire was completed by the Israeli RNs. The purpose of this questionnaire was to assist the nursing faculty in understanding the Israeli health care system and the nursing experience of each student. Results of the questionnaire identified where students worked and how long they had been nurses; their understanding of the Israeli health care system; identification of at risk populations and the five major health care problems in Israel today. Because the Health Education course was taught in English, another outcome of the questionnaire was to identify the level of student proficiency with the English language. Most of the students in the nursing course were proficient in a second, third, or even a fourth language. To ensure that students understood the course content from a language perspective several strategies were used. Before each class the instructor developed a list of vocabulary words that were essential for class content and students were required to look up the definitions in English. During the first few minutes of class, feedback was elicited from students regarding their understanding of these vocabulary words. When discussing the class content the instructor 5 used a set of questioning strategies to help ensure the English comprehension. For example, student were asked to define certain words such as “motivation and compliance” and then related the concept or definition to health education and expected health outcomes.. If students were still confused due to the comprehension of the English, a student who was proficient in tge English language presented the concepts to students in Hebrew. Literature Review Before developing the lecture material and learning activities, the course instructor conducted a review of the literature to find current research studies related to health belief models. The purpose for this review was to encourage evidence-based practice in understanding what may work or not work in using health belief modules in practice settings. One such study was a meta-analysis conducted by Bennet and Bozionelous (2000) related to the use of condoms and health belief concepts. The researchers reviewed 20 studies and found that attitudes were more powerful than social norms in the use of condoms and self-efficacy judgments were more influential than other perceived control factors. Another study conducted by Bish, Sutton, and Golombok (2000) focused on the use of Becker’s Health Belief Model and Ajzen and Fishbien’s Theory of Planned Behavior in identifying factors that influenced women to complete routine cervical pap smears. Findings from this study indicated that a positive attitude toward the procedure it self was more important in having it done than the perceived threat of disease or social pressure. Mclntosh and Kubena (1996), conducted a study by applying health belief model components to determine if changes in dietary habits could result in a reduction of fat and cholesterol intake. Findings from this found that the HBM components help people make changes in their dietary habits and that the beliefs were subject to influences by others in particular health care personnel who provided health teaching. An additional finding from 6 McIntosh and Kubena’s study was the influence of dietary cost in reducing fat and cholesterol. Although these three studies were only a partial representation of the literature review completed by the faculty member, the process helped the instructor to direct students to recent research studies that might be influential in finding the right combination of assessment factors and interventions to help individuals achieve desired health outcomes Health Education and a Health Belief Model The health care provider drives health education in Israel. Clients and families are referred to a guidance nurse or social worker where health information is provided. Community health education classes are offered on specific health issues such as smoking cessation, effects of diet on cardiac disease, how to control blood pressure, and the importance of mammography. Age specific health education in the schools focuses on nutrition, good dental care, protection from the sun, and safe sexual practices. Many health education classes also have a specific population focus, such as first time mothers who want to breast feed their infants. An over-riding theme from Israeli RNs in the health education course was that patients and families did not always follow the guidance offered by nurses, physicians, or social workers. Because of the lack of follow through by patients and families an increase in health care cost was seen through readmissions, proliferation of chronic illness, a rise in morbidly and mortality rates for specific diseases as well as injures caused by accidents in particular road accidents. Based upon the referral system, clients were sent to the guidance nurse for instruction. The philosophical under-pinning here was “we tell patients what they need to know and expect them to follow through”. To help Israeli nurses understand that information alone does not lead to client motivation, compliance, or the desired health care outcome, a six-hour block of instruction about health belief models was provided. The basic model that was introduced to students was 7 Becker’s health belief model. This model provided the framework in teaching nurses the importance of putting the focus on the client and not the guidance nurse/nurse educator. Becker’s Health Belief Model Becker (1974) developed the concepts of a health belief model by expanding upon the works of Reoenstock who studied individuals’ reasons for not participating in health- screening programs. Health belief from Becker’s point of view is based upon the idea that an individual must have the willingness to participate in health interventions and believe that being healthy is a highly valued outcome. Therefore, it was possible to predict if an individual would engage in positive health behaviors by determining the individuals’ perception of the disease, illness or accident, identification of modifying factors, and the likelihood that the individual will take some action. The most influential factor within Becker’s model that might prevent an individual from engaging in healthy behaviors was the perceived barriers (Barnstable, 1997). Becker’s model can be found in Table 1 Table 1 Becker’s The Health Belief Model ______Individuals Perceptions Modifying Factors Likelihood of Action Perceived Susceptibility Demographic, Socio-psychological Perceived Benefits Perceived Seriousness and Structural Variables Perceived Barriers Cues to Action: Advice from others Reminders form Primary Care Articles or TV information Illness of friend or family member Perceived Threat of Disease Likelihood of Taking Recommended Preventive Health Action
(Copied and modified from Bastable p.135) 8 Instructional Steps Using concepts of the health belief model developed by Becker the following steps were used to help students understand the basic components and the application of a health belief models. Step 1. Students were broken down into small discussion groups and asked to define health, illness, and health promotion from their own health perspective. Then they were to discuss how they envisioned or defined the health of their clients. At the end of the group discussions, each group presented their findings to the entire class. Step 2: An interactive teaching approach, utilizing power-point materials as a guide, basic concepts and principles related to health belief model developed by Becker was presented. Included in the presentation were Pender’s Health Promotion Model, Ajzen and Fishbien’s Theory of Reasoned Action, and Bandura’s Self-efficacy Model. Step 3: After the presentation of the basic concepts related to health belief, the students were ask to break down into their groups and each student was to identify a behavior tat they would like to see changed in themselves. Students were asked to look at their current behavior, which intellectually they know need to be changed; then using the health belief model to guide the assessment, ask themselves the following questions: To what extent did the RN students believe being over weight, smoking, lack of exercise, or not completing a mammogram would lead to the development of disease? If a problem were to develop how serious would it be? Who would support them in their quest to change behavior? What are their barriers to change? Students who smoked were asked the following questions: why do you smoke, what prevents you from stopping, and how 9 important is smoking to you? The purpose for this part of the class was to help students view the health issue as if they were the clients. Step 4: After completing the exercise in Step 3, each student was then asked to identify a client situation where a change in client behavior was a desired outcome. One student presented the problem of diabetic patients who live on a Kabutz and had difficulty managing their blood sugars and preventing foot ulcers. In this particular Kabutz meals were prepared and eaten in a central location. The cost for the care and treatment of diabetic patients was stressing the financial resources of the Kabutz. Although previous health teaching was conducted on foot care, the importance of a good diet, exercise, and other principles of diabetic care, patients continued to have problems. When the nurse was able to assess the client using health belief model principles, the following was a partial list of concerns that were discovered from the clients’ perspective: 1 a. Felt embarrassed because he/she was different from the other members in the Kabutz. 2 b. Express difficulty in talking with the individual who cooked the communal meal. 3 c. Wanted to be able to participate more fully in the activities of the Kabutz 4 d. Wanted to feel valued as a member who could contribute to the operations of the Kubutz.
Step 5. Evidence-based principles have become an integral part of baccalaureate nursing education and nursing practice. Therefore, the next steps in the learning process, students were asked to find primary research articles related to health belief models and 10 present their findings when completing course assignments. The application of research findings was evident in the final course papers, through class discussions, and during their microteaching activities. Step 6. The final step in the students’ learning process was for them to attend a health education class and determine if a health belief model or components from a health belief model were evident in helping clients achieve better health outcomes. If the presenter did not use a health belief model, and in most cases this was true, students were then asked to indicate which health belief model they would use, how would they use it, and why. The learning outcomes for this assignment were mixed. For example, some of the students identified principles of Bandura’s Self-efficacy. However, the students did not look at self- efficacy from the client’s perspective. Instead identified during the teaching session that the guidance nurse explained to the class participates that their efforts were essential in achieving positive health outcomes. It was clear in the students write up that the participants in the health education were passive learners without the opportunity to discuss their feelings and abilities toward meeting a health goal. Although the idea of self-efficacy has merit, more work was needed with the students to understand the difficulties, challenges, and possibilities from the client’s point of view. Other students were able to describe the difficulties and possibilities from the client’s perspectives. In guidance class for diabetic patients stated “ the intensity of the illness, side effects of the medication, and the length of time needed to be on a therapeutic mediation” impacted on how well the medication follow-up was continued. In addition, the same patients felt the lack of family support was a barrier to continued follow-through in taking medications for diabetes. Some students addressed a health belief model from a theoretical perspective by 11 explaining how to use the model to help adolescence engage in safe sexual practices. The model used in this context was Ajzen’s Theory of Planned Behavior. Using the concepts of attitude, subjective norms, and perceived control, the RNs were able to take these principles and help the guidance nurse (school nurse) prepare for a lecture on reducing at risk sexual behavior. An example of how the school nurse approached the young person’s attitude toward sex was to give students a questionnaire a week before the class. In this questionnaire the students were to tell how they felt about engaging in sexual activity and how important was it for them to use or not use a condom. The questionnaire also addressed social support regarding condoms use. Was it cool to use condoms or not from the peer group perspective? As students gained an understanding of health belief model principles, two ideas were generated. The first idea was related to how to use health belief principles in situations where illness was not the overriding concern. An example would be to encourage mothers to breast-feed and couples to participation in childbirth classes. A second idea presented by the RN students was how to use health belief principles as a change model for nursing staff. Through class discussions the students were asked to discuss principles related to health belief and self-efficacy in a non-illness context. Some of the RN students in the class were managers and supervisors wanted to know if the health belief module could be used to change behavior in other staff members. One situation identified by these nurse managers was how to help nursing assistants recognize a change in a client’s condition and then report findings to the staff nurse. Thus, a discussion was generated to identify how the nursing assistants might perceive the importance of their role as care gives and did they feel they could make a difference in the health outcomes for clients. Questions generated from this discussion were: 12 1 a. Does the nursing assistant feel that they can make a difference in client care? 2 b. Do other members of the health team value their input? 3 c. Do they feel valued as a member of the team? 4 d. Did the assistants find that the staff nurses listen to them? 5 e. Does the staff nurse provide cues to the nursing assistants? 6 f. Does the nursing assistant feel that they have the knowledge and resources to make a difference (self-efficacy)? 7 g. Who supports or recognizes the nursing assistant during their care of patients? 8 h. What are the barriers to working with elderly clients as perceived by nursing assistance?
At the end of the discussion nurses were able to begin to develop realistic approaches, which involved the nursing assistants that would improve early recognition of signs and symptoms indicating an elder client may be experiencing a change in health status. Before any in-service classes an idea that was generated was for the guidance nurse to talk with the nursing assistants to find out how they felt regarding early recognition of patient problems requiring immediate attention. It is also important to point out that understanding the problem from the individual’s perspective whether it is the client, staff member, or family member may help insure some successes in meeting expected outcomes. In the case of mothers who desire to breastfeed, asking the following questions to determine from the mothers perspective thoughts, experiences, and feelings regarding the art of breast-feeding, another class discussion was pursued. 1 a. How important is breast-feeding is to the mother (i.e. breast feeding can be used as a method of birth control, to have a healthy baby; attitude toward breast-feeding)? 13 1 b. Does the mother believe that she has the ability and resources to start and continue with breast-feeding (i.e. enough milk, prevent sore nipples, able to eat properly)? 2 c. Who offers support for breast-feeding (social support)? 3 d. What barriers have the mother identified that might become an issue related to breast- feeding (i.e. not able to breast-feed before, seeing friends who had a difficult time, working, other children to take care of, etc)? 4 e. What is the mother’s desired outcome (i.e. healthy baby, bonding with the infant, feeling good about herself as a mother, meeting a cultural and or religious requirement, etc.)?
Mothers, especially first time mothers, come to breast-feeding classes to learn how to breast-feed and to feel comfortable with the decision to breat-feed. Assessing a mother from a health belief perspective will enable nurses gain a more complete insight into the new mothers’ specific concerns. This assessment information can lead in the development of a teaching and intervention plan that meets the learning needs of breast- feeding mothers. Conclusion Using health belief models can assist nurses in seeing the health concerns from the client’s perspective. In many cases clients and families are referred or given health education programs without an assessment of their learning needs and are expected to follow the treatment plan. Nurses can empower clients to become active participants by including them in the decision making process through adequate collection of information from the client’s perspective. Faculty can facilitate the learning process by teaching in an interactive format that provides an opportunity for students to engage in learning about the application of health belief principles in clinical practice. Part of the teaching and learning process is to demonstrate how 14 course content can be applied realistically to clinical practice. Without a realistic application of course content that can be supported by research outcomes, improvement in clients’ health may not come to fruition. Clinical research is the next logical step in determining whether nurses who have been taught about health belief models actually apply the principles in clinical practice overtime and if so, do they effect change in the client’s willingness to change behaviors that result in healthier life styles. In addition, educational research should be conducted to determine which teaching methodologies best help students learn health belief principles and concepts. . Therefore, outcome research becomes an important goal whether it is conducted in the clinical or educational setting. 15 Bibliography Aaronld, J. (1998). Health Promotion: Handbook. Boston, MA: Mosby. Ajzen, I. & Fishbein, M. (1974). Understanding Attitudes and Predicting Social Behavior. Englewood Cliffs, NJ: Prentice-Hall, Inc. Bandura, A. (1997). Self-Efficacy: The Exercise of Control. New York, NY: W. H. Freeman and Company Bastable, S. (1997). Nurse as Educator: Principles of Teaching and Learning. Boston, MA: Jones and Bartlett Publishers. Becker, M. (1974). The health belief model and personal health behavior. Thorofare, NJ: Slack. Bennett, P., & Bozionelos, G. (2000, April). The theory of planned behavior as predictor of condom use: A narrative review. Psychology, Health, & Medicine 5 (3), 307-329. Bish, A., Sutton, S., & Golombok, S. ( 2000, February). Predicting uptake of a routine cervical smear test: A comparison of the health belief model and the theory of planned behavior. Psychology and Health, 15 (1), 35-352. McIntosh, W. & Kubena, K. (1996). An application of the health belief model to reductions in fat and cholesterol intake. Journal of wellness Perspectives, 12 (2), 98-108. O’connor, B. & Cappelli, M. (1999, May). Health Beliefs and the intent to use predictive genetic testing for cystic fibrosis carries status. Psychology, Health & Medicine, 4 (2), 157-169. Pender, N., Murdaugh, C., & Parsons, M. (2002). Health Promotion in Nursing. Upper Saddle River, NJ: Prentice Hall. 16