1
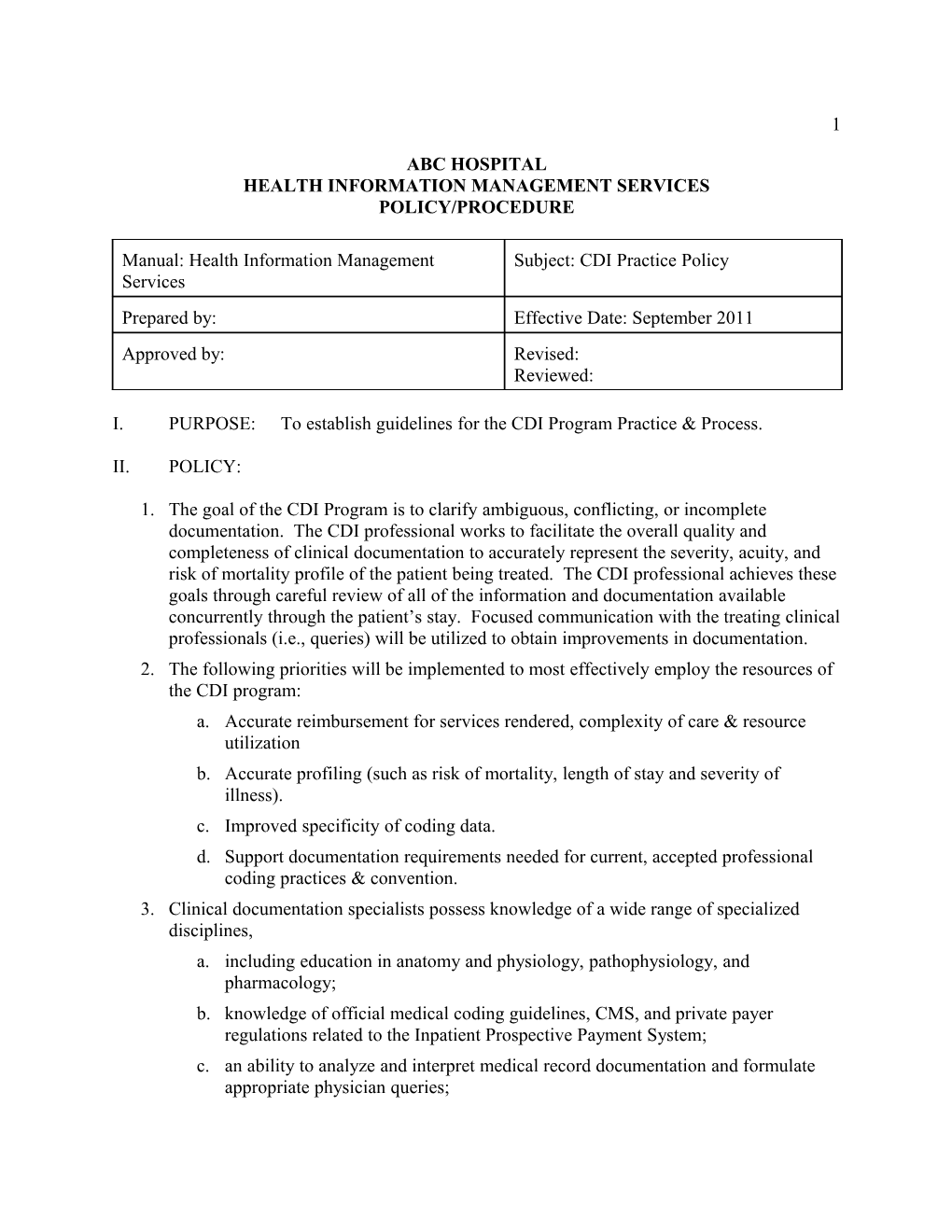
ABC HOSPITAL HEALTH INFORMATION MANAGEMENT SERVICES POLICY/PROCEDURE
Manual: Health Information Management Subject: CDI Practice Policy Services Prepared by: Effective Date: September 2011 Approved by: Revised: Reviewed:
I. PURPOSE: To establish guidelines for the CDI Program Practice & Process.
II. POLICY:
1. The goal of the CDI Program is to clarify ambiguous, conflicting, or incomplete documentation. The CDI professional works to facilitate the overall quality and completeness of clinical documentation to accurately represent the severity, acuity, and risk of mortality profile of the patient being treated. The CDI professional achieves these goals through careful review of all of the information and documentation available concurrently through the patient’s stay. Focused communication with the treating clinical professionals (i.e., queries) will be utilized to obtain improvements in documentation. 2. The following priorities will be implemented to most effectively employ the resources of the CDI program: a. Accurate reimbursement for services rendered, complexity of care & resource utilization b. Accurate profiling (such as risk of mortality, length of stay and severity of illness). c. Improved specificity of coding data. d. Support documentation requirements needed for current, accepted professional coding practices & convention. 3. Clinical documentation specialists possess knowledge of a wide range of specialized disciplines, a. including education in anatomy and physiology, pathophysiology, and pharmacology; b. knowledge of official medical coding guidelines, CMS, and private payer regulations related to the Inpatient Prospective Payment System; c. an ability to analyze and interpret medical record documentation and formulate appropriate physician queries; 2
d. and an ability to benchmark and analyze clinical documentation program performance. 4. Records will be reviewed within 48 hours of admission. Re-reviews will be conducted with a frequency as determined by the existent documentation and clinical status. Generally, each case will be reviewed at least every 3 days with variation from daily to weekly. 5. Outcomes data will be entered into the appropriate database on a weekly basis. Data will generally be entered within 4 weeks of discharge (or within one week of final coding if later). 6. Educational programs will be periodically offered and developed on clinical and coding topics for the development of expertise among the CDI staff. a. This program will be managed by identified members the CDI team. b. Resources will be drawn from a variety of sources including knowledgeable subject matter experts within the organization, commercial sources, consultants and directly from CDI and coding staff. 7. When there is a difference of opinion about post-discharge coding between the CDS and Coding Professional, the following process will be followed: a. The CDS & Coder discuss and attempt to resolve. b. If unable to resolve the difference of opinion, the conversation is referred to a designee of the Coding Manager for review. A summary of the opinions will be provided. c. Finally, the case may be referred to the Coding and CDI Managers. An external reviewer may be involved at their discretion. d. The final decision regarding coding practice rests solely with the Coding Manager. Reference: AHIMA. “Managing an Effective Query Process” Journal of AHIMA 79, No. 10 (October 2008): 83-88. AHIMA. “Guidance for Clinical Documentation Improvement Programs” Journal of AHIMA 81, No. 5 (May 2010): 45-50.