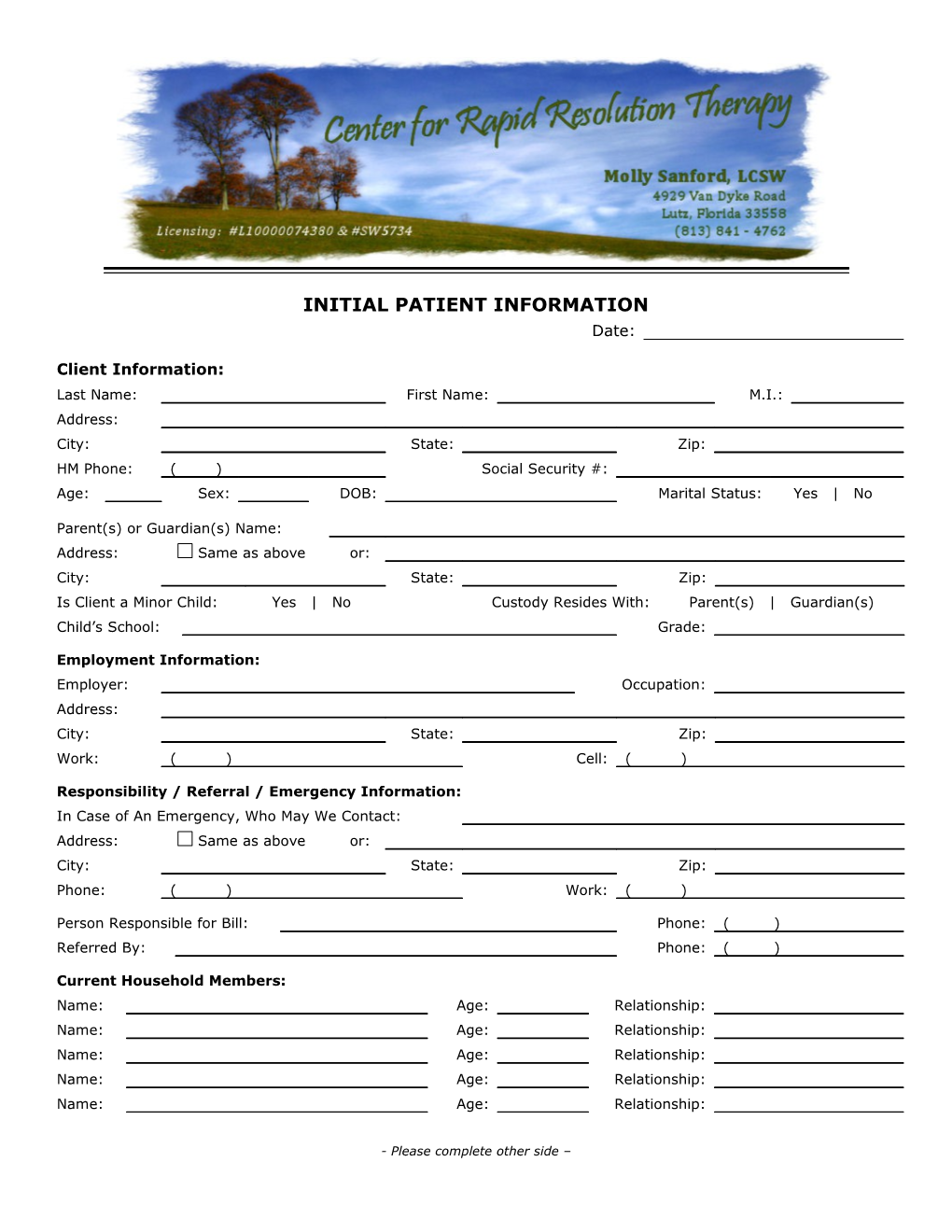
INITIAL PATIENT INFORMATION Date:
Client Information: Last Name: First Name: M.I.: Address: City: State: Zip: HM Phone: ( ) Social Security #: Age: Sex: DOB: Marital Status: Yes | No
Parent(s) or Guardian(s) Name: Address: Same as above or: City: State: Zip: Is Client a Minor Child: Yes | No Custody Resides With: Parent(s) | Guardian(s) Child’s School: Grade:
Employment Information: Employer: Occupation: Address: City: State: Zip: Work: ( ) Cell: ( )
Responsibility / Referral / Emergency Information: In Case of An Emergency, Who May We Contact: Address: Same as above or: City: State: Zip: Phone: ( ) Work: ( )
Person Responsible for Bill: Phone: ( ) Referred By: Phone: ( )
Current Household Members: Name: Age: Relationship: Name: Age: Relationship: Name: Age: Relationship: Name: Age: Relationship: Name: Age: Relationship:
- Please complete other side – Medical Information: Doctor Name: Phone :
State Briefly The Reason You Are Seeking Counseling At This Time:
Please List Any Known Allergies To Medications: None or:
Current Medications: None or:
Physical/Medical Conditions Pertinent To Counseling: None or:
Do You Currently Smoke: Yes | No
Previous Psychiatric Hospitalizations and/or Outpatient Counseling Dates: List: Date: List: Date:
Insurance/EAP Information: Primary Insurance Company Or EAP: Address: Contract #: Group #: Subscriber #: Name of Insured: Relationship to Client:
Insured’s DOB: Insured’s SSN#: Employer of Insured: Same as Above or:
Secondary Insurance (if any): Address: Contract #: Group #: Subscriber #:
Assignment Of Insurance Benefits: The undersigned hereby authorizes the release of any information relating to all claims for benefits submitted on behalf of myself and/or dependents. I further expressly agree and acknowledge that my signature on this document authorizes my physician/therapist to submit claims for benefits, for services rendered or for services to be rendered, without obtaining my signature on each and every claim to be submitted for myself and/or my dependents, and that I will be bound by this signature as though the undersigned had personally signed the particular claim.
I, , hereby authorize (Name of Insured) (Name of Insurance Company) to pay and hereby assign directly to Molly Sanford, LCSW, all benefits, if any, otherwise payable to me for her services as described on the attached forms. I understand that I am financially responsible for all charges incurred. I further acknowledge that any insurance benefits, when received by and paid to Molly Sanford, LCSW, will be credited to my account, in accordance with above said assignment.
(Authorized Signature of Subscriber) (Date) Patient Name: Date:
Symptom Checklist: Please check any of the statements you believe may be true of yourself
I have had feelings of depression: At times Constantly, for about how long? Periodically, for about how long?
I am having difficulty remembering: Short Term Long Term
Please check any of the statements you believe may be true of yourself: My sleeping habits have changed I am having difficulty concentrating I have less energy than I did before I am having trouble sleeping I am having difficulty making decisions I feel restless I sleep too much I have little or no appetite I think about dying I want to eat more than usual I don’t enjoy many of the things I used to I am more talkative than usual I feel great about myself I am easily distracted
Sometimes my thoughts are racing Sometimes I sweat too much Sometimes I feel like I am choking Sometimes I have chest pain or discomfort Sometimes I am afraid I am dying I am driven to meet my goals Sometimes I have chills or hot flashes Sometimes I am restless I am easily fatigued Sometimes I tremble Some behaviors I do over and over again
Sometimes I have feelings of being detached from myself I am irritable or others have indicated that they think I am irritable I don’t need much sleep; I feel rested with only a little sleep Sometimes my heart pounds or beats very rapidly Sometimes I have sensations of shortness of breath or smothering Sometimes I feel dizzy, unsteady, lightheaded, or faint Sometimes I have nausea or abdominal distress Sometimes I think my thoughts or actions are crazy Sometimes I have numbness or tingling sensations
I have cycling thoughts, pictures or fears in my head that I find it difficult to stop I am doing things I enjoy, but it has gotten me in trouble or has the potential to get me in trouble Some things I feel I must do or I just don’t feel right or comfortable or I can’t relax Sometimes I have feelings that I am dying, losing control, or going crazy Sometimes I have excessive fears of
I never drink beer, wine or liquor drinks I sometimes drink beer, wine, or liquor drinks I drink some type of alcoholic drink at least three times a week I drink some type of alcoholic drink more than three times a week I think I have a drinking problem Someone has told me that they think I have a problem with drinking I used to drink alcoholic drinks, but I no longer do I used to drink “too much” alcohol I used to have a problem with alcohol but I no longer do
I smoke cigarettes. How many packs/day? I used to smoke cigarettes. How many packs/day? I quit smoking (when?):
I have the following medical conditions:
I take the following medications (please include dosage): Informed Consent for Treatment
Client Name: Social Security #: Date of Birth:
I, , am voluntarily seeking treatment for Responsible Party From Patient Name Therapist
1. I understand that it is my responsibility to understand my mental health insurance benefits and to notify Molly Sanford, LCSW, of any changes as soon as I am aware of such changes. It is the responsibility of Molly Sanford, LCSW, to bill for services provided. It is my responsibility to pay for services not covered by my insurance company unless restricted by contract. Co- payments are required by insurance companies to be collected at the time the service is rendered. 2. I understand that if I have a scheduled appointment and I need to cancel it, I will do so at least 24 hours in advance or more if possible. If I do not provide 24 hours notice, I may be charged for the appointment. 3. My therapist will recommend a specific type of treatment for me and will explain the advantages and risks. It is my responsibility to ask questions if I am not clear about my treatment plan. 4. I understand that what I talk about in sessions with my therapist is considered confidential and that my therapist will not disclose that information to anyone without a release of information except for the following as required by law: physical or sexual abuse of a minor child or an elderly adult, clear intent to harm oneself or someone else, court order from a judge. 5. I also understand that my therapist, in keeping with generally accepted standards of practice, may seek confidential clinical supervision regarding my treatment plan. The purpose of such consultation is to assure quality care. Every effort is made to protect my identity. 6. I understand that an on-call therapist (who may or may not be my regular therapist) is available for emergency situations only. (Immediate consultation needed to avert harm to self or others.) If a situation is urgent, I will leave a message with the office and can expect a call within 12 hours. I also understand that if needed, I will call 911 first. 7. A copy of my clinical records will be maintained for seven years. Should I require a copy, I will submit a written request to release records to a person specified in the request. 8. I understand that I and my therapist alone are responsible for my treatment and that no other therapist sharing office space or in affiliation with my therapist will be responsible for any aspect of my on-going treatment. 9. I understand that mental health providers are required to submit psychiatric diagnosis and a “treatment plan” including diagnosis, description of the problem, personal background information, treatment goals, and therapy methods to my mental health managed care company. I permit the therapy staff to submit any information required to use my benefits. 10. I have read a copy of the “Notice of Information Practices” and I understand that I may request a hard copy of this document for my personal records.
Signature of Patient Date
Signature of Witness Date THIS NOTICE DESCRIBES HOW MEDICAL INFORMATION ABOUT YOU MAY BE USED AND DISCLOSED AND HOW YOU CAN GET ACCESS TO THIS INFORMAITON. PLEASE REVIEW IT CAREFULLY.
Understanding your Personal Mental Health Record Information Each time you visit a hospital, physician or other healthcare provider the provider makes a record of your visit. Typically this record contains your health history current symptoms, examination and test results, diagnoses, treatment and a plan for future care or treatment. This information, often referred to as your medical record, serves as a: Basis for planning your care and treatment Means of communication among the many health professionals who contribute to your care Legal document describing the care you received Means by which you or a third-party payer can verify that you actually received the services billed for A tool in medical education A source of information for public health officials charged with improving the health of the regions they serve A tool to assess the appropriateness and quality of care you received A tool to improve the quality of healthcare and achieve better patient outcomes
Understanding what is in your health records and how your health information is used helps you to: Ensure its accuracy and completeness Understand who, what, where, why, and how others may access your health information Make informed decision about authorizing disclosure to others Better understand the health information rights detailed below
Your Rights Under the Federal Privacy Standard Although your health records are the physical property of the healthcare provider who completed it, you have certain rights with regard to the information contained therein. You have the right to: Request restriction on uses and disclosures of your health information for treatment, payment, and health care operations. Health care operations consist of activities that are necessary to carry out the operations of the provider, such as quality assurance and peer review. The right to request restriction does not extend to uses or disclosures permitted or required under ‘ ‘ 164.502(a)(2)(I) (disclosures to you), 164.510 (for facility directories, but note that you have the right to object to such uses), or 164.512 (uses and disclosures not requiring a consent or an authorization). The latter uses and disclosures include, for example, those required by law, like mandatory communicable disease reporting. In those cases, you do not have a right to request restriction. Even in those cases in which you do have the right to request restriction, we do not have to agree to the restriction. If we do, however, we will adhere to it unless you request otherwise or we give you advance notice. You may also ask us to communicate with you by alternate means and, if the method of communication is reasonable, we must grant the alternate communication request. Receive and keep a copy of this notice of information practices. Although we have posted a copy in prominent locations throughout the facility, if you access those copies, you nonetheless have a right to a hard copy on request. The law requires us to ask you to acknowledge receipt of your copy. Inspect and copy your health information upon request. Again, this right is not absolute. In certain situations, such as if access would cause harm, we can deny access. You do not have a right of access to the following: o Psychotherapy notes. Such notes comprise those that are recorded in any medium by a healthcare provider who is a mental health professional documenting or analyzing a conversation during a private counseling session or a group, joint, or family counseling session and that are separated from the rest of your medical record. Information compiled in reasonable anticipation of or for use in civil, criminal, or administrative actions or proceedings. Any of your health information that is subject to the Clinical Laboratory Improvement Amendments of 1988 (CLIA), 42 U.S.C. ‘ 263a, to the extent that the provision of access to the individual would be prohibited by law. Information was obtained from someone other than a healthcare provider under a promise of confidentiality and the access requested would be reasonable likely to reveal the source of the information.
In other situations, the provider may deny you access but, it if does, the provider must provide you with a review of the decision denying access. These reviewable grounds for denial include: When a licensed healthcare professional has determined, in the exercise of professional judgment, that the access is reasonable likely to endanger the life or physical safety of the individual or another person. When the PHI (Personal Health Information) makes reference to another person (other than a healthcare provider) and a licensed healthcare provider has determined, in the exercise of professional judgment, that the access is reasonably likely to cause substantial harm to such other person. The request is made by the individual’s personal representative and a licensed healthcare professional has determined, in the exercise of professional judgment that the provision of access to such personal representative is reasonably likely to cause substantial harm to the individual or another person.
For these reviewable grounds, another licensed professional must review the decision of the provider denying access within 60 days. If we deny you access, we will explain why and what your rights are, including how to seek review.
If we grant access, we will tell you what, if anything, you have to do to get access. We reserve the right to charge a reasonable, cost-based fee for making copies. Request amendment/correction of your health information. We do not have to grant the request if: o We did not create the record. If, as in the case of a consultation report from another provider, we did not create the record, we cannot know whether it is accurate or not. Thus, in such cases, you must seek amendment/correction from the party creating the record. If they amend or correct the record, we will put the corrected record in our records. The records are not available to you as discussed immediately above. The record is accurate and complete.
If we deny your request for amendment/correction, we will notify you why, how you can attach a statement of disagreement to your records (which we may rebut), and how you can complain to our complaint official or to the Department of Health and Human Services. If we grant the request, we will make the correction and distribute the correction to those who need it and those you identify to us that you want to receive the corrected information.
Obtain an accounting of non-routine uses and disclosures, those other than for treatment, payment, and health care operations, or of protected health information about them. We do not need to provide an accounting for: For disclosures to you For disclosures authorized by you For disclosures of limited data sets (partially de-identified data used for research, public health, or health care operations). For the facility directory or to persons involved in your care or for other notification purposes as provided in ‘ 164.510 (uses and disclosures requiring an opportunity for the individual to agree or to object, including notification to family members, personal representatives, or other persons responsible for the care of the individual, of the individual’s location, general condition, or death). For national security or intelligence purposes under ‘ 164.512(k)(2)(disclosures not requiring consent, authorization, or an opportunity to object). For information disclosed as required by law (harm to self or others or physical/sexual abuse). That occurred before April 14, 2003.
We must provide the accounting within 60 days. The accounting must include: Date of each disclosure Name and address of the organization or person who received the protected health information Brief description of the information disclosed Brief statement of the purpose of the disclosure that reasonably informs you of the basis for the disclosure or, in lieu of such statement, a copy of your written authorization or a copy of the written request for disclosure.
The first accounting in any 12-month period is free. Thereafter, we reserve the right to charge a reasonable, cost-based fee. Revoke your [consent or] authorization to use or disclose health information except to the extent that we have already taken action in reliance on the consent or authorization.
Our Responsibilities Under the Federal Privacy Standard In addition to providing you your rights, as detailed above, the federal privacy standard requires us to: Maintain the privacy of your health information, including implementing reasonable and appropriate physical, administrative, and technical safeguards to protect the information. Provide you with this notice as to our legal duties and privacy practices with respect to individually identifiable health information we collect and maintain about you. Abide by the terms of this notice Train our personnel concerning privacy and confidentiality Implement a sanction policy to discipline those who breach privacy/confidentiality or our policies with regard thereto. Mitigate (lessen the harm of) any breach of privacy/confidentially.
WE RESERVE THE RIGHT TO CHANGE OUR PRACTICES AND TO MAKE THE NEW PROVISIONS EFFECTIVE FOR ALL INDIVIDUALLY IDENTIFIABLE HEALTH INFORMATION WE MAINTAIN. SHOULD WE CHANGE OUR INFORMATION PRACTICES, WE WILL MAIL A REVISED NOTICE TO THE ADDRESS YOU HAVE SUPPLIED US.
We will not use or disclose your health information without your consent or authorization except as described in this notice or otherwise required by law.
How to Get More Information or to Report a Problem If you have questions and/or would like additional information, you may contact Molly Sanford, LCSW at Bridgewater Professional Park, 4929 Van Dyke Rd., Lutz, Florida 33558.
Disclosures for Treatment, Payment, and Health Operations Treatment: When you give us consent, with the regulatory consent granted by the Department of Health and Human Services, we may use or disclose your health information for treatment.
Example: Your therapist will record information in your record to diagnose your condition and determine the best course of treatment for you. The primary caregiver will give treatment orders and document what he or she expects other members of the healthcare team to do to treat you. Those other members will then document the actions they took and their observations. In that way the primary caregiver will know how you are responding to treatment.
We will also provide your physician, other healthcare professionals, or a subsequent therapist with copies of your records to assist them in treating you once we are no longer treating you.
Payment: When you give us consent, with the regulatory consent granted by the Department of Health and Human Services, we may use or disclose your health information for payment.
Example: We may send a bill to you or to a third-party payer, such as a health insurer. The information on or accompanying the bill may include information that identifies you, your diagnosis, treatment received, and supplies used.
Health Operations: When you give us consent, with the regulator consent granted by the Department of Health and Human Services, we may use or disclose your health information for health operations.
Members of our staff, the risk or quality improvement manager, or members of a quality assurance team may use information in your health record to assess the care and outcomes in your cases and the competence of your therapist. We will use this information in an effort to continually improve the quality and effectiveness of the healthcare and services we provide. Uses and Disclosures Other than for Treatment, Payment, or Health Care Operations Business Associates: We provide some services through contracts with business associates. Examples include certain diagnostic tests, a copy service to copy your records, computer technician, attorney, and the like. When we use these services, we may disclose your health information to the business associate so that they can perform the function(s) we have contracted with them to do and bill you or your third-party payer for services rendered. To protect your health information, however, we require the business associate to appropriately safeguard your information.
Notification: We may use or disclose information to notify or assist in notifying a family member, personal representative, or another person responsible for your care, you location, and general condition.
Communication with Family: Unless you object, health professionals using their best judgment, may disclose to a family member, other relative, close personal friend, or any other person you identify, health information relevant to that person’s involvement in your care or payment related to your care.
Research: We may disclose information to researchers when their research has been approved by an institutional review board that has reviewed the research proposal and established protocols to ensure the privacy of your health information.
Continuity of Care: We may contact you to provide appointment reminders or information about treatment alternatives or other health-related benefits and services that may be of interest to you.
Food and Drug Administration (FDA): We may disclose to the FDA health information relative to adverse effects/events with respect to food, drugs, supplements, product or product defects, or post marketing surveillance information to enable product recalls, repairs, or replacement.
Workers Compensation: We may disclose health information to the extent authorized by and the to the extent necessary to comply with laws relating to workers compensation or other similar programs established by law. In these cases, you will be notified and asked to sign a release of information.
Law Enforcement: We may disclose health information purposes as required by law or in response to a court order. If subpoenaed, you will be notified and asked to sign a release of information.
Health Oversight agencies an public health authorities: If a member of our work force or a business associate believes in good faith that we have engaged in unlawful conduct or otherwise violated professional or clinical standards and are potentially endangering one or more patients, workers or the public, they may disclose your health information to health oversight agencies and/or public health authorities, such as the department of health.
The federal Department of Health and Human Services (DHHS): Under the privacy standards, we must disclose your health information to DHHS as necessary for them to determine our compliance with those standards.
State law: Under the laws of the State of Florida, certain information must be disclosed. This information includes knowledge of physical or sexual abuse of a minor, senior, or other person considered protected under state law. It also includes the duty to protect a person from harm from themselves and the duty to warn anyone who the therapist determines in his/her clinical judgment may be at risk for harm from someone else.
Release of Information: You may request, in writing, that information be released to another party. We will at that time release the information requested to the person or persons requested.
Effective Date:
| Signature of Patient Signature of Witness
Acknowledgement of Information Practices
Patient Name Date
Address FL DR LIC #
City State Zip
I, have read the Statement of information Patient Name Practices of Molly Sanford, LCSW, and agree to the information contained therein. I understand that this Statement meets HIPAA requirements to protect my privacy.
Signature of Patient Date
Signature of Witness Date
A personal copy of this acknowledgement and a copy of the Statement of Information Practices of Molly Sanford, LCSW, will be made available to you. Please Choose One: NO, I do not require a copy YES, I received a copy on Date
Signature of Patient Date
Signature of Witness Date