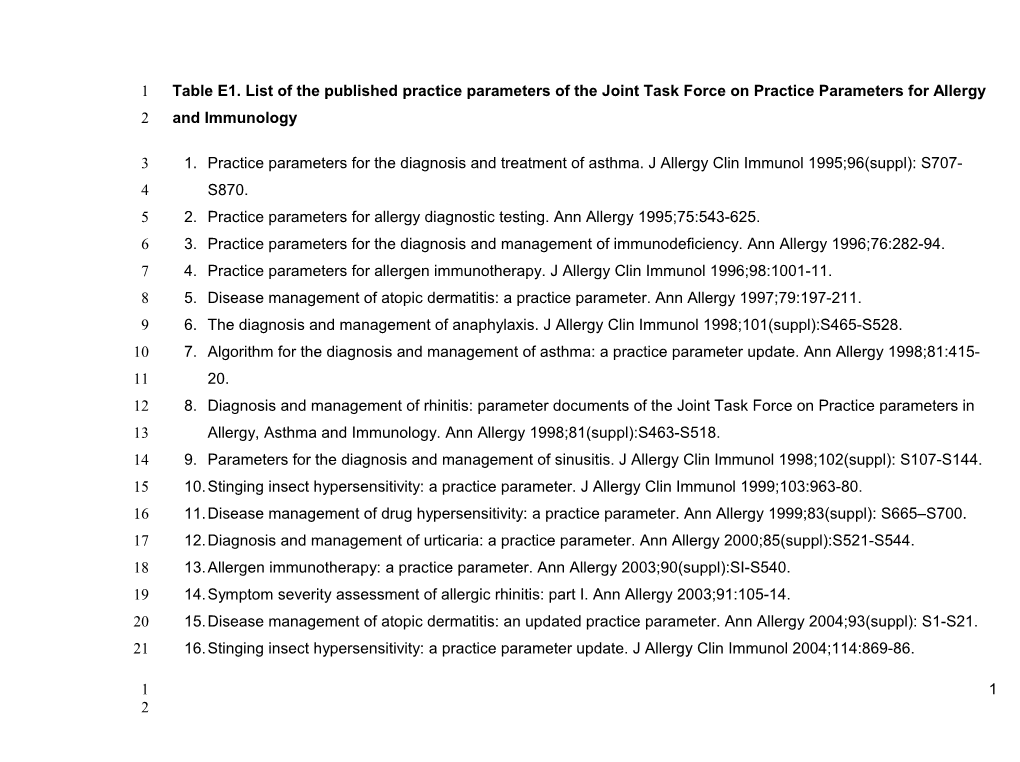
1 Table E1. List of the published practice parameters of the Joint Task Force on Practice Parameters for Allergy 2 and Immunology
3 1. Practice parameters for the diagnosis and treatment of asthma. J Allergy Clin Immunol 1995;96(suppl): S707- 4 S870. 5 2. Practice parameters for allergy diagnostic testing. Ann Allergy 1995;75:543-625. 6 3. Practice parameters for the diagnosis and management of immunodeficiency. Ann Allergy 1996;76:282-94. 7 4. Practice parameters for allergen immunotherapy. J Allergy Clin Immunol 1996;98:1001-11. 8 5. Disease management of atopic dermatitis: a practice parameter. Ann Allergy 1997;79:197-211. 9 6. The diagnosis and management of anaphylaxis. J Allergy Clin Immunol 1998;101(suppl):S465-S528. 10 7. Algorithm for the diagnosis and management of asthma: a practice parameter update. Ann Allergy 1998;81:415- 11 20. 12 8. Diagnosis and management of rhinitis: parameter documents of the Joint Task Force on Practice parameters in 13 Allergy, Asthma and Immunology. Ann Allergy 1998;81(suppl):S463-S518. 14 9. Parameters for the diagnosis and management of sinusitis. J Allergy Clin Immunol 1998;102(suppl): S107-S144. 15 10.Stinging insect hypersensitivity: a practice parameter. J Allergy Clin Immunol 1999;103:963-80. 16 11.Disease management of drug hypersensitivity: a practice parameter. Ann Allergy 1999;83(suppl): S665–S700. 17 12.Diagnosis and management of urticaria: a practice parameter. Ann Allergy 2000;85(suppl):S521-S544. 18 13.Allergen immunotherapy: a practice parameter. Ann Allergy 2003;90(suppl):SI-S540. 19 14.Symptom severity assessment of allergic rhinitis: part I. Ann Allergy 2003;91:105-14. 20 15.Disease management of atopic dermatitis: an updated practice parameter. Ann Allergy 2004;93(suppl): S1-S21. 21 16.Stinging insect hypersensitivity: a practice parameter update. J Allergy Clin Immunol 2004;114:869-86.
1 1 2 22 17.The diagnosis and management of anaphylaxis: an updated practice parameter. J Allergy Clin Immunol 23 2005;115(suppl):S483-S523. 24 18.Practice parameter for the diagnosis and management of primary immunodeficiency. Ann Allergy 2005; 25 94(suppl):S1-S63. 26 19.Attaining optimal asthma control: a practice parameter. J Allergy Clin Immunol 2005;116(suppl):S3-S11. 27 20.The diagnosis and management of sinusitis: a practice parameter update. J Allergy Clin Immunol 2005; 28 116(suppl):S13-S47. 29 21.Food allergy: a practice parameter. Ann Allergy Asthma Immunol 2006;96(suppl 2):S1-S68. 30 22.Contact dermatitis: a practice parameter. Ann Allergy Asthma Immunol 2006;97(suppl 2):S1-S38. 31 23.Cox L, Li JT, Nelson H, Lockey R. Allergen immunotherapy: A practice parameter second update. J Allergy Clin 32 Immunol 2007; 120:S25-85. 33 24.Bernstein IL, Li JT, Bernstein DI, et al. Allergy Diagnostic Testing-An Updated Practice Parameter. Ann Allergy 34 100; March 2008:S1-S148 35 25.Wallace D, Dykewicz M, Bernstein D, et al. The diagnosis and management of rhinitis: An updated practice 36 parameter. The Journal of Allergy and Clinical Immunology 2008;122:S1-S84. 37 26.Kelso JM, Li JT, Nicklas RA, et al. Adverse Reactions to Vaccines. Ann Allergy 2009; 103(4)S1-S16. 38 27.Lieberman P, Nicklas RA, Oppenheimer J, et al. The diagnosis and management of anaphylaxis practice 39 parameter: 2010 update. J Allergy Clin Immunol 2010;126:477-80 e1-42. 40 28.Drug allergy: an updated practice parameter. Ann Allergy Asthma Immunol 2010;105:259-73. 41
42
3 2 4 43
44 Table E2. List of summary statements without accompanying explanations
45Summary Statement 1: The immunologic response to subcutaneous immunotherapy is characterized by 46decreases in the sensitivity of end organs and changes in the humeral and cellular responses to the administered 47allergens. A
48Summary Statement 2: Reduction in end organ response with immunotherapy includes decreased early and late 49response of the skin, conjunctiva, nasal mucosa and bronchi to allergen challenge, decrease in allergen induced 50eosinophil, basophil and mast cell infiltration, blunting of mucosal priming, and reduction of non-specific 51bronchial sensitivity to histamine. A
52Summary Statement 3: Shortly after initiation of immunotherapy there is an increase in CD4+CD25+ regulatory T- 53lymphocytes secreting IL-10 and TGF-B associated with immunologic tolerance, defined as a long-lived decrease 54in allergen-specific T-cell responsiveness. With continued immunotherapy there is some waning of this response
55and immune deviation from Th2 to Th1 cytokine response to the administered allergen predominates. A
56Summary Statement 4: Specific- IgE levels initially rise, then gradually fall. Levels of specific IgG1 IgG4 and IgA 57rise. None of these changes in antibody levels have been shown to correlate strongly with clinical improvement. 58A
59Summary Statement 5: Increases in allergen-specific IgG are not predictive of the degree or duration of efficacy of 60immunotherapy. However, functional alterations in allergen-specific IgG such as changes in avidity and/or affinity 61for allergen might play a role in determining clinical efficacy. LB
5 3 6 62Summary Statement 6: Immunotherapy is effective for treatment of allergic rhinitis, allergic conjunctivitis, allergic 63asthma, and stinging insect hypersensitivity. Therefore, immunotherapy merits consideration in patients with 64these disorders as a possible treatment option. A
65 Summary Statement 7: Allergen immunotherapy should be considered for patients who have demonstrable 66 evidence of specific-IgE antibodies to clinically relevant allergens. The decision to begin allergen 67 immunotherapy may depend on a number of factors, including but not limited to: patient 68 preference/acceptability, adherence, medication requirements, response to avoidance measures, and the 69 adverse effects of medications. D
70Summary Statement 8: There are some data indicating that immunotherapy can be effective for atopic dermatitis 71when this condition is associated with aeroallergen sensitivity. B
72Summary Statement 9: The potential for benefit in symptoms related to oral allergy syndrome with inhalant 73immunotherapy directed at the cross-reacting pollens has been observed in some studies but not in others. For 74this reason, more investigation is required to substantiate that a benefit in oral allergy symptoms will occur with 75allergen immunotherapy. C
76Summary Statement 10a: Immunotherapy should be considered if the patient has had a systemic reaction to a 77Hymenoptera sting, especially if such a reaction was associated with respiratory symptoms, cardiovascular 78symptoms, or both and if the patient has demonstrable evidence of specific-IgE. A
79 Summary Statement 10b: Measurement of baseline serum tryptase level is recommended in patients with 80 moderate or severe anaphylactic reactions to stings because its predictive value is useful regardless of the 81 decision about VIT. Elevated tryptase is associated with more frequent and more severe anaphylactic 82 reactions to stings, as well as greater failure rates with VIT and greater relapse rates after stopping VIT.B
7 4 8 83Summary Statement 11: Large local reactions (LLR) to insect stings may cause significant morbidity and impair 84quality of life. VIT may significantly reduce the size and duration of large local reactions and may be considered in 85patients who have frequent and disabling LLR, particularly those with occupational exposure. B
86Summary Statement 12: Clinical trials do not support the use of subcutaneous immunotherapy for food 87hypersensitivity. A
88Summary Statement 13: The safety and efficacy of oral and sublingual immunotherapy for food hypersensitivity 89is currently investigational.NR
90 Summary Statement 14: Clinical studies do not support the use of allergen immunotherapy for chronic 91 urticaria, angioedema or both. Therefore, allergen immunotherapy for patients with chronic urticaria or 92 angioedema, or both is not recommended. D
93 Summary Statement 15: Clinical parameters, such as symptoms and medication use, might be useful 94 measures of the efficacy of immunotherapy in a clinical setting; however, repetitive skin testing of patients 95 receiving immunotherapy is not recommended. A
96Summary Statement 16: Allergen immunotherapy in asthmatic patients should not be initiated unless the patient’s 97asthma is stable with pharmacotherapy. C
98Summary Statement 17: Immunotherapy for children is effective and well tolerated. It has been shown to prevent 99the new onset of allergen sensitivities in monosensitized patients as well as progression from allergic rhinitis to 100asthma. Therefore immunotherapy should be considered (along with pharmacotherapy and allergen avoidance) in 101the management of children with allergic rhinitis/ rhinoconjunctivitis, allergic asthma, and stinging insect 102hypersensitivity. B
9 5 10 103 Summary Statement 18: Immunotherapy may be initiated in young children. Indications are similar to those of 104 other age groups. D
105 Summary Statement 19: In patients, who otherwise have the indication for specific immunotherapy, there is no 106 absolute upper age limit for initiation of immunotherapy. D
107Summary Statement 20a: Allergen immunotherapy may be continued but is usually not initiated in the pregnant 108patient. C
109Summary Statement 20b: If pregnancy occurs during the build-up phase and the patient is on a dose unlikely to 110be therapeutic, discontinuation of immunotherapy should be considered. D
111Summary Statement 21: Immunotherapy can be considered in patients with immunodeficiency and autoimmune 112disorders. C
113Summary Statement 22: Clinical and physiological improvement can be demonstrated very shortly after the 114patient reaches a maintenance dose. A
115Summary Statement 23: Patients should be evaluated at least every 6 to 12 months while they receive 116immunotherapy. D
117Summary Statement 24: The patient’s response to immunotherapy should be evaluated on a regular basis. A 118decision about continuation of effective immunotherapy should generally be made after the initial period of 3 to 5 119years of treatment. Some patients may experience sustained clinical remission of their allergic disease after 120discontinuing immunotherapy, but others may relapse. The severity of disease, benefits sustained from
11 6 12 121treatment, and convenience of treatment are all factors that should be considered in determining whether to 122continue or stop immunotherapy for any individual patient. D
123Summary Statement 25: Although there are no specific tests to distinguish, which patients will relapse after 124discontinuing VIT, there are clinical features that are associated with a higher chance of relapse, notably a history 125of a very severe reaction to a sting, elevated baseline serum tryptase level, a systemic reaction during VIT (to a 126sting or a venom injection), honeybee venom allergy, and treatment duration of less than 5 years. C
127Summary Statement 26: At present, there are no specific tests or clinical markers that will distinguish between 128patients who will relapse and those who will remain in long-term clinical remission after discontinuing effective 129inhalant allergen immunotherapy, and the duration of treatment should be determined by the physician and 130patient after considering the risks and benefits associated with discontinuing or continuing immunotherapy. D
131Summary Statement 27: Published studies indicate that individual local reactions do not appear to be predictive 132of subsequent systemic reactions. However, some patients with greater frequency of large local reactions might 133be at an increased risk for future systemic reactions. C
134Summary Statement 28: Local reactions were found to not predict local reactions at the next injection in one 135retrospective study. C
136Summary Statement 29: Glycerin concentrations up to 50% were not associated with significantly higher local 137reaction rates. Higher glycerin concentrations are associated with injection pain, which correlates with the total 138amount of glycerin injected. C
13 7 14 139Summary Statement 30: Antihistamines have been demonstrated to be beneficial in decreasing local reactions 140during cluster and rush protocols, while leukotriene antagonists were shown effective in a rush protocol. Though 141commonly utilized, the effect of these medications in reducing local reactions during conventional build-up and 142maintenance immunotherapy injections has not been extensively reported. A
143Summary Statement 31: Although there is a low risk of severe systemic reactions with appropriately administered 144allergen immunotherapy, life-threatening and fatal reactions do occur. A
145Summary Statement 32: An assessment of the patient’s current health status should be made before 146administration of the allergy immunotherapy injection to determine whether there were any health changes that 147might require modifying or withholding that patient’s immunotherapy treatment. Poorly controlled asthma has 148been identified as a risk factor for a severe immunotherapy reaction. Before the administration of the allergy 149injection, the patient should be evaluated for the presence of asthma symptoms. One might also consider an 150objective measure of airway function (eg, peak flow) for the asthmatic patient before allergy injections. B
151Summary Statement 33: The majority of safety data on allergen immunotherapy reactions is in the context of 30 152minutes. Because most serious systemic reactions from allergen immunotherapy occur within 30 minutes after 153an injection, patients should remain in the physician’s office /medical clinic for at least 30 minutes after the 154immunotherapy injection. C
155Summary Statement 34: Delayed systemic reactions, defined as occurring after the 30 minute wait period, may 156occur and, in general, are not severe. B
15 8 16 157Summary Statement 35: Biphasic immunotherapy reactions, defined as resolution of the initial reaction with 158recurrence 2 to 24 hours, were reported in up to 23% of patients, who experienced a systemic reaction after 159allergen immunotherapy in one study. Biphasic reactions were typically less severe than the initial reaction. C
160Summary Statement 36: Several large studies demonstrate that life- threatening anaphylactic reactions after the 161first 30 minutes are rare. Delayed and biphasic immunotherapy systemic reactions may occur outside of a 162supervised medical facility. Thus, patients should be educated regarding the possible signs and symptoms of 163systemic reactions and to contact their health care professional or seek emergency medical attention, as 164indicated. The decision to prescribe epinephrine autoinjectors to patients receiving allergen immunotherapy is 165up to the physician’s discretion and is based on a number of considerations. C
166Summary Statement 37: Exposure to β-adrenergic blocking agents is a risk factor for more serious and treatment- 167resistant anaphylaxis. Concomitant use of β-blockers and allergen immunotherapy should be carefully 168considered from an individualized risk/benefit standpoint, and incorporate patient preferences in the medical 169decision-making process. C
170Summary Statement 38: The balance of possible risks and benefits is not the same for patients with the potential 171for life-threatening stinging insect reaction who are also taking a β-blocker. In patients who are unable to replace 172a β-blocker with an equally efficacious alternative, concomitant administration of venom immunotherapy and a β- 173blocker is warranted. C
174Summary Statement 39: Glucagon may be efficacious for the treatment of refractory β-blocker associated 175anaphylaxis. C
176Summary Statement 40: ACE inhibitors have been associated with greater risk for more severe reaction from 177venom immunotherapy as well as field stings. ACE inhibitor discontinuation should be considered for patients 17 9 18 178receiving venom immunotherapy. Concurrent administration of venom immunotherapy and an ACE inhibitor is 179warranted in selected cases in which no equally efficacious alternative for an ACE inhibitor exists, and this is 180judged to be favorable from an individualized risk/benefit standpoint and consideration of patient preferences. No 181evidence exists that angiotensin receptor blockers are associated with greater risk for anaphylaxis from allergen 182immunotherapy. C
183Summary Statement 41: β-blocker and ACE Inhibitors are frequently prescribed in combination. Concomitant 184administration of both of these medications in a patient who requires venom immunotherapy may be warranted, if 185favorable, from an individualized assessment of potential risks and benefits and patient preferences. D
186Summary Statement 42: Patients selected for immunotherapy should be cooperative and compliant. D
187 Summary Statement 43: Allergen immunotherapy in asthmatic patients should not be initiated unless the 188 patient’s asthma is stable. C
189 Summary Statement 44: Medical conditions that reduce the patient’s ability to survive the systemic allergic 190 reaction or the resultant treatment are relative contraindications for allergen immunotherapy. Examples 191 include severe asthma uncontrolled by pharmacotherapy and significant cardiovascular disease. C
192 Summary Statement 45: Allergen immunotherapy should be administered in a setting where procedures that 193 can reduce the risk of anaphylaxis are in place and where the prompt recognition and treatment of anaphylaxis 194 is ensured. C
195 Summary Statement 46: Epinephrine is the treatment of choice for immunotherapy systemic reactions. Risk 196 factors for fatal immunotherapy reactions include delayed administration of epinephrine. B
19 10 20 197 Summary Statement 47: The starting dose for build-up is usually a 1000-fold or 10,000-fold dilution of the 198 maintenance concentrate, although a lower starting dose might be advisable for highly sensitive patients. D
199 Summary Statement 48: The frequency of allergen immunotherapy administration during a conventional build- 200 up phase is generally 1 to 3 injections per week. D
201 Summary Statement 49: The dose of allergen immunotherapy extract should be appropriately reduced after a 202 systemic reaction if immunotherapy is continued. D
203 Summary Statement 50: Immunotherapy given during periods when the patient is exposed to increased levels 204 of allergen(s) to which they are highly sensitive may be associated with an increased risk of a systemic 205 reaction. However, while survey data have noted this to be a risk factor for severe reactions, several published 206 studies have not found an association between pollen seasons and systemic reactions. C
207 Summary Statement 51: There is no retrospective or prospective published evidence to support modification 208 of doses of allergen immunotherapy because of treatment gaps during the build-up or maintenance 209 immunotherapy phase. However, it is customary to reduce the dose of allergen immunotherapy extract when 210 the interval between injections is prolonged. D
211 Summary Statement 52: With cluster immunotherapy, 2 or more injections are administered per visit to 212 achieve a maintenance dose more rapidly than with conventional schedules. C
213 Summary Statement 53: Studies with single allergens utilizing a cluster schedule demonstrated a similar or 214 increased frequency of systemic reactions compared with immunotherapy with conventional schedules. A 21 11 22 215 Summary Statement 54: Rush schedules can achieve a maintenance dose more quickly than weekly 216 schedules. A
217 Summary Statement 55: Rush schedules with inhalant allergens are associated with an increased risk of 218 systemic reactions. However, rush protocols for administration of stinging Hymenoptera have not been 219 associated with a similarly high incidence of systemic reactions. A
220 Summary Statement 56: Premedication may reduce the frequency of systemic reactions caused by 221 conventional immunotherapy. A
222 Summary Statement 57: Premedication before cluster and rush immunotherapy with aeroallergens may reduce 223 the rate of systemic reactions. Combination therapy is effective in reducing systemic and local reactions 224 during accelerated immunotherapy build-up protocols. A
225 Summary Statement 58: Omalizumab pretreatment has been shown to improve the safety and tolerability of 226 cluster and rush immunotherapy schedules in patients with moderate-persistent asthma and allergic rhinitis, 227 respectively. Additionally, omalizumab used in combination with immunotherapy has been shown to be 228 effective in improving symptom scores compared to immunotherapy alone. A
229 Summary Statement 59: Once a patient reaches a maintenance dose, the interval between injections often can 230 be progressively increased as tolerated up to an interval of 4 weeks for inhalant allergens and up to 8 weeks 231 for venom. Some individuals might tolerate longer intervals between maintenance dose injections. A
23 12 24 232 Summary Statement 60: Allergen immunotherapy extract injections should be given using a calibrated small 233 volume syringe with a 26-to 27-gauge 1/2 or 3/8 inch non-removable needle. C
234 Summary Statement 61: The injection should be given subcutaneously in the lateral or posterior portion of the 235 arm. D
236 Summary Statement 62: Regardless of the location, allergen immunotherapy should be administered under the 237 direct supervision of an appropriately trained physician and/ or qualified physician extender in a facility with 238 the appropriate equipment, medications and personnel to treat anaphylaxis. D
239 Summary Statement 63: The preferred location for administration of allergen immunotherapy is in the office of 240 the physician who prepared the patient’s allergen immunotherapy extract. D
241Summary Statement 64: Patients at high risk of systemic reactions, where possible, should receive 242immunotherapy in the office of the physician who prepared the patient’s allergen immunotherapy extract. D
243Summary Statement 65: In rare and exceptional cases, when allergen immunotherapy cannot be administered in a 244medical facility and withholding this therapy would result in a serious detriment to the patients’ health (eg, VIT for 245a patient living in a remote area), careful consideration of potential benefits and risks of at-home administration of 246allergen immunotherapy should be made on an individual patient basis. If this approach is used, informed 247consent should be obtained from the patient, and the person administering the injection to the patient must be 248educated about how to administer immunotherapy and recognize and treat anaphylaxis. D
25 13 26 249Summary Statement 66: If a patient on immunotherapy transfers from one physician to another, a decision must 250be made by the physician to whom the patient has transferred as to whether to continue immunotherapy. D
251Summary Statement 67: If immunotherapy is continued, a decision must then be made about whether to continue 252unchanged the immunotherapy program initiated by the previous physician or to start a new immunotherapy 253program. Patients may continue to receive the immunotherapy extract prepared by the patient’s previous 254physician if this is acceptable to the transferring and accepting physicians. D
255Summary Statement 68: A detailed documentation of the patient’s schedule and allergen extract content must 256accompany a patient when he or she transfers responsibility for their immunotherapy care from one physician to 257another. In addition, a record of previous response to and compliance with this program should be communicated 258to the patient’s new physician. D
259Summary Statement 69: An allergen immunotherapy extract must be considered different if there is any change. 260There is potentially an increased risk of a systemic reaction if the immunotherapy extract is changed because of 261the possible variability in composition and potency of allergen extracts. If the allergen immunotherapy extract is 262changed, the patient may need to be retested for specific-IgE sensitivity and started on an immunotherapy 263formulation and schedule that is based on this reevaluation.D
264Summary Statement 70: Immunotherapy is effective for pollen, animal allergens, dust mite, mold/ fungi and 265Hymenoptera hypersensitivity. Therefore, immunotherapy should be considered as part of the management 266program in patients who have symptoms related to exposure to these allergens, as supported by the presence of 267specific IgE antibodies. A
268Summary Statement 71: There is limited data on the efficacy of cockroach immunotherapy. B 27 14 28 269Summary Statement 72: There are few studies that have investigated the efficacy of multiallergen subcutaneous 270immunotherapy. These studies have produced conflicting results, with some demonstrating significant clinical 271improvement compared with placebo and others showing no benefit over optimal pharmacotherapy and 272environmental control measures. Thus, it is important to treat the patients only with relevant allergens. B
273Summary Statement 73: The selection of the components of an allergen immunotherapy extract should be based 274on a careful history in correlation with positive allergy skin tests or serum specific- IgE antibodies. The allergen 275immunotherapy extract should contain only clinically relevant allergens. In choosing the components for a 276clinically relevant allergen immunotherapy extract, the physician should be familiar with local and regional 277aerobiology and indoor and outdoor allergens, paying special attention to potential allergens in the patient’s own 278environment D
279Summary Statement 74: Skin testing has been the primary diagnostic tool in clinical studies of allergen 280immunotherapy. Therefore, in most patients, skin testing should be used to determine whether the patient has 281serum specific- IgE antibodies. Appropriately interpreted serum specific-IgE antibodies can also be used. C
282Summary Statement 75: Nonstandardized extracts can vary widely in biologic activity and composition, 283regardless of a particular wt/vol or PNU potency and should not be considered equipotent. B
284Summary Statement 76: When possible, standardized extracts should be used to prepare the allergen 285immunotherapy extract treatment sets. A
286Summary Statement 77: Allergen immunotherapy extract preparation should be performed by individuals 287experienced and trained in handling allergenic products. A customized individual allergen immunotherapy extract 288should be prepared from a manufacturer’s extract or extracts in accordance to the patient’s clinical history and 289allergy test results and may contain single or multiple allergens. D
29 15 30 290Summary Statement 78: Consideration of the following principles is necessary when mixing allergen extract: (1) 291cross-reactivity of allergens, (2) optimization of the dose of each constituent, and (3) enzymatic degradation of 292allergens. B
293Summary Statement 79: The selection of allergens for immunotherapy should be based (in part) on the cross- 294reactivity of clinically relevant allergens. Knowledge of allergen cross-reactivity is important in the selection of 295allergens for immunotherapy because limiting the number of allergens in a treatment vial may be necessary to 296attain optimal therapeutic doses of each of the components. Many botanically related pollens contain allergens 297that are cross-reactive. When pollens are substantially cross-reactive, selection of a single pollen within the 298cross-reactive genus or subfamily may suffice. When pollen allergens are not substantially cross-reactive, testing 299for and treatment with multiple locally prevalent pollens might be necessary. B
300Summary Statement 80: The efficacy of immunotherapy depends on achieving an optimal therapeutic dose of 301each of the constituents in the allergen immunotherapy extract. A
302Summary Statement 81: The maintenance concentrate should be formulated to deliver a dose considered to be 303therapeutically effective for each of its constituent components. The maintenance concentrate vial is the highest- 304concentration allergy immunotherapy vial (eg, 1:1 vol/vol vial). The projected effective dose is called the 305maintenance goal. Some individuals unable to tolerate the projected effective dose will experience clinical 306benefits at a lower dose. The maintenance dose is the dose that provides therapeutic efficacy without significant 307adverse local or systemic reactions and might not always reach the initially calculated projected effective dose. 308This reinforces that allergy immunotherapy must be individualized. A
31 16 32 309Summary Statement 82: Studies designed to investigate the effect of combining extracts with high proteolytic 310activity, such as cockroach and mold/fungi, with extracts such as pollen, dander and dust mite extracts, have 311demonstrated a significant loss of potency with some of these extracts. Separation of extracts with high 312proteolytic enzyme activities, from other extracts is recommended. It may be necessary to prepare two or more 313vials to provide allergen immunotherapy containing an optimal dose of each component, while avoiding allergen 314extract combinations that may result in degradation of some or all of the components. B
315Summary Statement 83: Allergen immunotherapy extracts should be stored at 4 to 8ºC to reduce the rate of 316potency loss. B
317Summary Statement 84: Extract manufacturers conduct stability studies with standardized extracts that expose 318them to various shipping conditions. It is the responsibility of each supplier or manufacturer to ship extracts 319under validated conditions that are shown not to adversely affect the product’s potency or safety. C
320Summary Statement 85: In determining the allergen immunotherapy extract expiration date, consideration must 321be given to the fact that the rate of potency loss over time is influenced by several separately and collectively, 322including (1) storage temperature, (2) presence of stabilizers and bactericidal agents, (3) concentration, (4) 323presence of proteolytic enzymes, and (5) volume of the storage vial. D
324Summary Statement 86: Administration of an incorrect injection is a potential risk of allergen immunotherapy. An 325incorrect injection is an injection given to the wrong patient or a correct patient receiving an injection of an 326incorrect dose. A customized individual maintenance concentrate of the allergen immunotherapy extract and 327serial dilutions, whether a single extract or a mixture of extracts, prepared and labeled with the patient’s name 328and birth date might reduce the risk of incorrect (i.e., wrong patient) injection. D
329Summary Statement 87: The mixing of antigens in a syringe is not recommended because of the potential for 330treatment errors and cross-contamination of extracts. C
33 17 34 331Summary Statement 88: Serial dilutions of the maintenance concentrate should be made in preparation for the 332build-up phase of immunotherapy. D
333Summary Statement 89: Dilution limits the number of antigens that can be added to a maintenance concentrate if 334a therapeutic dose is to be delivered. A
335Summary Statement 90: A consistent uniform labeling system for dilutions from the maintenance concentrate 336might reduce errors in administration and therefore is recommended. D
337Summary Statement 91: The allergen immunotherapy extract contents, informed consent for immunotherapy, and 338administration of extracts should be documented. D
339Summary Statement 92: Allergen extracts can be administered by several routes in addition to the subcutaneous 340route. Currently, there are no FDA-approved formulations for a noninjection immunotherapy extract. A
341Summary Statement 93: Randomized, controlled clinical trials with dust mite and pollen sublingual 342immunotherapy have demonstrated significant improvement in symptoms and medication use in patients with 343allergic rhinitis and asthma. A
344Summary Statement 94: Local reactions, primarily oral-mucosal, are common with sublingual immunotherapy. 345Systemic reactions may occur and a few have been reported in individuals, who were unable to tolerate 346subcutaneous immunotherapy. A few reported cases have been of a severity to be categorized as anaphylaxis A
347Summary Statement 95: Clinical trials evaluating the safety and efficacy of sublingual immunotherapy for 348ragweed and grass-pollen allergic rhinitis. Currently, there are no FDA-approved formulation for sublingual 349immunotherapy. A
35 18 36 350Summary Statement 96: Randomized, controlled studies have demonstrated that nasal immunotherapy with dust 351mite and pollen extracts is effective in reducing symptom and medication use. Local adverse reactions are 352common with this approach and are the most frequently cited reason for discontinuation of treatment in one large 353prospective study. The use of this approach has decreased considerably since the introduction of SLIT. C
354Summary Statement 97: A 3-injection course of intralymphatic immunotherapy is as effective as a 3-year course 355of conventional subcutaneous immunotherapy in one non-controlled study. NR
356Summary Statement 98: Epicutaneous immunotherapy resulted in significantly higher treatment success in one 357placebo-controlled study. However, there were no significant differences in the primary outcome and nasal 358provocation test scores between the groups. NR
359Summary Statement 99: Several clinical trials with oral and sublingual immunotherapy demonstrate an increased 360tolerance to oral food challenge in individual with food hypersensitivity while on therapy. Oral and sublingual 361food immunotherapy is investigational. NR
362Summary Statement 100: Allergoids are modified allergen extracts processed in a way that reduces the extract's 363allergenicity while preserving its antigenicity. B
364Summary Statement 101: Adjuvants may enhance the effectiveness of allergen immunotherapy by shifting the
365immune response toward Th1 production. Two adjuvants most extensively studied with allergen immunotherapy 366are an immunostimulatory oligonucleotide sequence of DNA containing a CpG motif (CpG) and 3-deacylated 367monophospholipid A (MPL). Clinical trials with these adjuvants, in combination with ragweed (CPG and MPL) and 368grasses (MPL), demonstrate significant improvement in allergic rhinitis symptoms with 4 to 6 injections 369administered pre-seasonally. Neither of these adjuvants are available as FDA-approved allergen extracts. NR
37 19 38 370
371 Table E3. Systemic reactions reported with subcutaneous immunotherapy and skin testing with aeroallergens 372 and venom in some publications from 1995 to 2009E1
P/R* Author (year) Location Duration Schedule Nº patients / Systemic reaction rate Time, observation Nº of injections Patients Injections minutes period Allergen (%) (%) (range)
R PhillipsE2 (2009) USA 6 months Conventional 883/ 17 (1.9) 18 (0.13) 20 average(1- Inhalant & 14,000 60min) Venom R DaVeigaE3 USA Jul/02- 830/ 15 (1.8) 36 (0.37) 50% (2008) Mar/07 <30min, 8% Conventional 9659 > 1 hour
Inhalant All severe reactions < 30min
R RankE4 USA 2004-2006 Conventional 338/10497 25 (7.4) 29 (0.28) 50% > (2008) 30min, all Inhalant more severe SR >30min R RoyE 5 USA, 2 years Conventional 12,963/ 258 (2) 283(0.026) ND (2007) multicenter 1,108,621 Inhalant 39 20 40 R HarveyE6 USA Jan /97-7/02 Rush Inhalant 65 25/65 (38) Does not 5 Moderate (2004) apply 20-45min 1 severe started mild at 55min P TinkelmanE7 USA Jan-Dec Conventional 4,512/ 96 (2.1) 98 (0.06) All severe 1991 156,800 reactions (1995) Inhalant < 30min R BrehlerE8 (2000) Germany 2-day 9 Rush 403/ 43 (10.7) ND ND injections venom 3,627 R SerranoE9 (2009) Spain, 1996-2006 Cluster 1,147/6,982 39** (3.4) 42** (0.6) 23% multicenter <30min Depot (10-360)***
Inhalants P SchiappoliE10 (2009) 1 Italy, multi- Up to 2006 Depot 1,738/60,785 57 (3.28) 95 (0.156) 44% center <30min (one grade 4), 56% >30min (span 45min- 24h) P WintherE11 (2006) 2 Denmark 3 years Depot, 1038/23,047 341 582 (2.5) 50%<30m modified (32.8) in (all cluster grade 4 were <30min),
41 21 42 50% >30min P MorenoE12 Spain, 1996-97 Conventional 423/17,526 18 (3.7) 53(0.3) All <30min, multicenter except 2 AD (2004) Inhalant flares R RagusaE13 E14 Italy 1981-90 Conventional 4000/435,854 115 (5.2) 115 (0.06) Almost all SR within (1997, 2004) 1991-2000 Inhalant 26 (1.1) 26 (0.01) 30min R GastaminzaE15 (2003) Spain 5 years Conventional 1212/29,762 60 (5) 79 (0.27) 73% < 30min Inhalant & Venom R AkcakayaE16 Turkey 1989-97 Depot 88/5760 12 (13.6) 12 (0.2) Most (2000) <30min Dust mite P BaggE17 US 2007-08 SPT 1456 6 (0.4) Does not apply (2009) ID testing 46 (3.2) R ValyaseviE18 (1999) US Jan/92- SPT 16505 5 (0.03) Does not 4 < 25min, Jun/97 apply 1 at 75min ID testing 269 373 * P/R = prospective or retrospective, ID = intradermal skin testing, ND = no data, SPT = skin puncture/prick test, SR = systemic reaction, US 374 = United States of America
375 ** Including 7 grade 0 reactions (=non-specific reactions).
376 *** The patient with the only grade 3 reaction was the only patient with an onset at 10min. All others started later.
377Reprinted with permission from Elsevier Publishers
378
43 22 44 379
380Table E4. Example of a build-up schedule for weekly immunotherapy
Dilution (vol/vol) Volume (mL) 1:1000 0.05 0.10 0.20 0.40 1:100 0.05 0.10 0.20 0.30 0.40 0.50 1:10 0.05 0.07 0.10 0.15 0.25 0.35 0.40 0.45 0.50 Maintenance concentrate 0.05 0.07 0.10 0.15 0.20 0.25 0.30 45 23 46 0.35 0.40 0.45 0.50 381Dilutions are expressed as vol/vol from the maintenance concentrate.
47 24 48 382
383Table E5. Example of immunotherapy dose adjustment schedule for unscheduled gaps in allergen 384immunotherapy injection intervals (modification of the AAAAI skin testing and immunotherapy consent and 385instruction forms: immunotherapy administration instruction form, which can be found at http://www.aaaai.org)
386Build-up phase for weekly or biweekly injections (time intervals from missed injection)
387 Up to 7 days, continue as scheduled (ie, if on weekly build-up, then it would be up to 14 days after administered 388 injection or 7 days after the missed scheduled injection).
49 25 50 389 Eight to 13 days after missed scheduled injection; repeat previous dose. 390 Fourteen to 21 days after missed scheduled injection; reduce dose 25%. 391 Twenty-one to 28 days after missed scheduled injection; reduce previous dose 392 50%. 393 Then increase dose each injection visit as directed on the immunotherapy 394 schedule until therapeutic maintenance dose is reached. 395 This suggested approach to modification of doses of allergen immunotherapy 396 because of gaps between treatment during the build-up phase is not based on 397 retrospective or prospective published evidence, but it is presented as a 398 sample for your consideration. The individual physician should use this or a 399 similar protocol as a standard operating procedure for the specific clinical 400 setting. A similar dose-reduction protocol should be developed for gaps in 401 maintenance immunotherapy
51 26 52 402Table E6. Example of a cluster immunotherapy schedule
Concentration as Visit Dose (mL) dilution of maintenance vial 1 0.10 1:1000 vol/vol 0.40 1:1000 vol/vol 0.10 1:100 vol/vol 2 0.20 1:100 vol/vol 0.40 1:100 vol/vol 0.07 1:10 vol/vol 3 0.10 1:10 vol/vol 0.15 1:10 vol/vol 0.25 1:10 vol/vol 4 0.35 1:10 vol/vol 0.50 1:10 vol/vol 5 0.07 1:1 vol/vol 0.10 1:1 vol/vol 6 0.15 1:1 vol/vol 0.20 1:1 vol/vol 7 0.30 1:1 vol/vol 0.40 1:1 vol/vol 8 0.50 1:1 vol/vol 403
404
53 27 54 405
406Table E7. Recommended documentation for allergen immunotherapy 407prescription forms
408The purpose of the allergen immunotherapy prescription form is to define the contents 409of the allergen immunotherapy extract in enough detail that it could be precisely 410duplicated. The following information should be on an immunotherapy prescription 411form:
412Patient information:
413Patient name, patient number (if applicable), birth date, telephone number, and 414picture (if available) should be included.
415Preparation information:
416Name of person and signature preparing the allergen immunotherapy extract should 417be included.
418Date of preparation should be recorded.
419Bottle name should be included (eg, trees and grass). If abbreviations are used, a 420legend should be included to describe the meaning of the abbreviations.
421Allergen immunotherapy extract content information:
422The following information for each allergen should be included on the form in a 423separate column:
424 Content of the allergen immunotherapy extract, including common name or 425 genus and species of individual antigens and detail of all mixes, should be 426 included.. 427 Concentration of available manufacturer’s extract. 428 Volume of manufacturer’s extract addadded to achieve the projected effective 429 concentration. This can be calculated by dividing the projected effective
55 28 56 430 concentration by the concentration of available manufacturer’s extract times the 431 total volume. 432 The type of diluent (if used). 433 Extract manufacturer. 434 Lot number should be included. 435 Expiration date should be recorded and not exceed the expiration date of any 436 of the individual components.
437
57 29 58 438
439 Figure E8a. Allergen immunotherapy extract blank and E8b completed 440 prescription form
441 59 30 60 442
443
61 31 62 444
445Table E9. Labels for allergen immunotherapy extracts
446Each vial of allergen immunotherapy extract should be labeled in a way that permits 447easy identification. Each label should include the following information (example in 448Figs 2 and 3):
449 Appropriate patient identifiers might include the patient’s name, patient’s 450 number, patient’s picture, and birth date. 451 The contents of the allergen immunotherapy extract in a general way should be 452 included. The detail with which this can be identified depends on the size of the 453 label and the number of allergens in the vial. Ideally, allergens should be 454 identified as trees, grasses, weeds, mold, dust mite, cockroach, cat, and dog. 455 Because of space limitations, it might be necessary to abbreviate the antigens 456 (eg, T, G, W, M, DM, Cr, C, and D respectively [see Appendix 1). A full and 457 detailed description of vial contents should be recorded on the prescription/ 458 content form. 459 The dilution from the maintenance concentrate (vol/vol) should be recorded. If 460 colors, numbers, or letters are used to identify the dilution, they also should be 461 included. 462 The expiration date should be included.
463
464
63 32 64 465
466Table E10. Examples of possible abbreviations for allergen immunotherapy 467extract components
Tree T Grass G Bermuda B Weeds W Ragweed R Mold M Alternaria Alt Cladosporium Cla Penicillium Pcn Cat C Dog D Cockroach Cr Dust mite DM D farinae Df D pteronyssinus Dp Mixture Mx 468
469
65 33 66 470
471Table E11 Allergen immunotherapy administration form recommended 472documentation
473The purpose of the allergen immunotherapy administration form is to document the 474administration of the allergen immunotherapy extract to a patient. Its design should be 475clear enough so that the person administering an injection is unlikely to make an error 476in administration. It also should provide documentation in enough detail to determine 477what was done on each visit. The following recommendations on allergen 478immunotherapy are taken from The Joint Task Force on Practice Parameters.
479Patient information:
480 Patient’s name, date of birth, telephone number, and patient’s picture (optional 481 but helpful). 482 Allergen immunotherapy extract information: 483 Allergen immunotherapy extract name and dilution from maintenance in vol/vol 484 bottle letter (eg, A and B), bottle color, or number, if used. 485 Expiration date of all dilutions.
486Administration information in separate columns:
487Date of injection.
488Arm administered injection, which might facilitate determination of exact cause of local 489reaction.
490Projected build-up schedule.
491Delivered volume reported in milliliters.
492Description of any reactions. The details of any treatment given in response to a 493reaction would be documented elsewhere in the medical record and referenced on the 494administration form.
67 34 68 495Patient’s health before injection. This can be performed through a verbal or written 496interview of the patient before administering the immunotherapy injection. The patient 497should be questioned about increased asthma symptoms, b-blocker use, change in 498health status (including pregnancy and recent infections), or an adverse reaction to a 499previous injection (including delayed large local reactions persisting through the next 500day). Patients with significant systemic illness generally should not receive an 501injection.
502Antihistamine use. Antihistamines are frequently a component of an allergy 503medication regimen, and it would be important to note whether a patient is taking an 504antihistamine on the day he or she receives his or her immunotherapy injection. For 505consistency in interpretation of reactions, it might be desirable for a patient to either 506take or avoid antihistamines on a regular basis on the days he or she receives 507immunotherapy. The physician should note on the form whether he or she 508recommends the patient consistently take an antihistamine on immunotherapy 509treatment days.
510Peak flow reading. Consider obtaining a peak expiratory flow rate measurement 511before administering an immunotherapy injection to asthmatic patients. Poorly 512controlled asthma is considered a risk factor for immunotherapy. Obtaining a peak 513expiratory flow rate measurement before the immunotherapy injection might help 514identify patients with symptomatic asthma. The patient’s baseline peak expiratory flow 515rate should be provided on the form as a reference. Health care professionals 516administering immunotherapy injections should be provided with specific guidelines 517about the peak expiratory flow rate measurement for when an immunotherapy 518injection should be withheld and the patient referred for clinical evaluation.
519Baseline blood pressure. It might be useful to record the patient’s blood pressure as a 520baseline for future reference.
69 35 70 521Figure E12. Allergen immunotherapy administration form for single extract
522
523Figure E13. Allergen immunotherapy administration form for two extracts
524
71 36 72 525
73 37 74 526
527Figure E14. Health screen record
528
75 38 76 529
530
531
532Figure E15. Allergen immunotherapy systemic reaction treatment record
77 39 78 533
534
535
79 40 80 536Figure E16. Patterns of allergen cross-reactivity
Patterns of Allergen Cross-Reactivity
Allergen Cross-Reactivity (
Allergen groups (species within the genus) listed below show strong cross-reactivity within the associated group. Using one member of the group for the allergy immunotherapy extract may be adequate to protect the patient against the entire group.
Strong cross-reactivity Weeds: Grasses: between members of the (Ambrosia) Subfamily Festucoideae, Festucoidea subfamily Short ragweed Southern and Slender Meadow fescue but unique allergenicity Giant ragweed ragweed do not cross- Timothy of Eragrostoideae False ragweed react as well as other Rye (Bermuda) & Western ragweed ragweed species. Kentucky blue Panicoideae subfamilies (Artemisia) Orchard (Bahia & Johnson ) Sages Strong cross-reactivity Red top Wormwood between Artemisia Mugworts species Trees: Chenopod and Amaranth families (Cupressaceae) Juniper Cupressaceae family: (Salsola) Russian thistle Skin testing Cedar strong evidence for (Chenopodium) Lambs quarter suggests strong Cypress cross-reactivity (Kochia) Burning bush pollen cross- (Betulaceae) between members of reactivity Birch this family. One across chenopod and Alder member of this family amaranth family Hazel should be adequate. (Amaranthus) boundaries. Hornbeam Pigweed Predominant weed Hophornbeam Red root pigweed species n in (Fagaceae) Betulaceae and Fagales Amaranth geographic region Beech families have extensive should be used. Oak cross-reactivity. Chestnut The use of one of the (Oleaceae) locally prevalent (Atriplex) Ash members should be Saltbush Strong cross- European olive adequate. Wingscale reactivity between Privet Atriplex species (Populus) Oleacea family: Cottonwood Strong cross-reactivity Dust Mites: D. pteronyssinus Poplar between the Fraxinus D. farinae Aspen (ash) and Olea (olive) Cockroach: species D. pteronyssinus and D. farinae have allergens German cockroach with extensive interspecific cross-reacting American cockroach epitopes as well as unique allergens. Generally, considered individually, dosage modifications Although, German cockroaches are most likely may be made if used in combination to account to occur in American homes, an equal mixture for this cross-reactivity of German and American cockroach is appropriate
537
81 41 82 538
539
540
541Table E17. Allergen immunotherapy informed consent
Documentation that Informed consent is a process by which a patient and informed consent has physician discuss various aspects of a proposed treatment. been obtained. Although many allergists use a written consent form before starting immunotherapy, a reasonable alternative is simply to document the consent process in the medical record. The consent process usually consists of the following:
what the treatment is and alternatives to the treatment;
potential benefits to be expected from the treatment;
potential risks, including a fair description of how frequently they are likely to occur, if known, including the possibility of death;
Since the informed costs associated with immunotherapy and who pays for them; consent process is the anticipated duration of treatment; and complex and details might vary from state any specific office policies that affect treatment. to state, each allergist/immunologist should decide how they should document informed consent. Legal advice might be
83 42 84 useful.
542
543
544References for On-line Repository
545E1 Cox L, Larenas-Linnemann D, Lockey RF, Passalacqua G. Speaking the same 546language: The World Allergy Organization Subcutaneous Immunotherapy Systemic 547Reaction Grading System. J Allergy Clin Immunol 2010;125:569-74, 74 e1-74 e7. IV
548E2. Phillips J, Bag A, Lockey R. Systemic Reactions to Subcutaneous Allergen 549Immunotherapy and the response to epinephrine. J Allergy Clin Immunol 2009; 550123:S60.III
551E3. DaVeiga S, Caruso K, Golubski S, Lang D. A Retrospective Survey of Systemic 552Reaction from Allergen Immunotherapy. J Allergy Clin Immunol 2008:S124.III
553E4. Rank MA, Oslie CL, Krogman JL, Park MA, Li JT. Allergen immunotherapy 554safety: characterizing systemic reactions and identifying risk factors. Allergy Asthma 555Proc 2008; 29:400-5.III
556E5. Roy SR, Sigmon JR, Olivier J, Moffitt JE, Brown DA, Marshall GD. Increased 557frequency of large local reactions among systemic reactors during subcutaneous 558allergen immunotherapy. Ann Allergy Asthma Immunol 2007; 99:82-6.III
559E6. Harvey SM, Laurie S, Hilton K, Khan DA. Safety of rush immunotherapy to 560multiple aeroallergens in an adult population. Ann Allergy Asthma Immunol 2004; 56192:414-9. III
85 43 86 562E7. Tinkelman DG, Cole WQ, 3rd, Tunno J. Immunotherapy: a one-year prospective 563study to evaluate risk factors of systemic reactions. J Allergy Clin Immunol 1995; 95:8- 56414. III
565E8. Brehler R, Wolf H, Kutting B, Schnitker J, Luger T. Safety of a two-day ultrarush 566insect venom immunotherapy protocol in comparison with protocols of longer duration 567and involving a larger number of injections. J Allergy Clin Immunol 2000; 105:1231-5.III
568E9. Serrano P, Justicia J, Sanchez C, Cimarra M, Fernandez-Tavora L, Orovitg A, et 569al. Systemic tolerability of specific subcutaneous immunotherapy with index-of- 570reactivity–standardized allergen extracts administered using clustered regimens: a 571retrospective, observational, multicenter study. Ann Allergy Asthma Immunol 2009; 572102:247–52. III
573E10. Schiappoli M, Ridolo E, Senna G, et al. A prospective Italian survey on the safety 574of subcutaneous immunotherapy for respiratory allergy. Clin Exp Allergy 2009.
575E11. Winther L, Arnved J, Malling HJ, Nolte H, Mosbech H. Side-effects of allergen- 576specific immunotherapy: a prospective multi-centre study. Clin Exp Allergy 2006;36:254- 57760. III
578E12. Moreno C, Cuesta-Herranz J, Fernandez-Tavora L, Alvarez-Cuesta E. 579Immunotherapy safety: a prospective multi-centric monitoring study of biologically 580standardized therapeutic vaccines for allergic diseases. Clin Exp Allergy 2004; 34:527- 58131.III
582E13. Ragusa FV, Passalacqua G, Gambardella R, Campanari S, Barbieri MM, 583Scordamaglia A, et al. Nonfatal systemic reactions to subcutaneous immunotherapy: a 58410-year experience. J Investig Allergol Clin Immunol 1997; 7:151-4.III
585E14. Ragusa VF, Massolo A. Non-fatal systemic reactions to subcutaneous 586immunotherapy: a 20-year experience comparison of two 10-year periods. Allerg 587Immunol (Paris) 2004; 36:52-5.
87 44 88 588E15. Gastaminza G, Algorta J, Audicana M, Etxenagusia M, Fernandez E, Munoz D. 589Systemic reactions to immunotherapy: influence of composition and manufacturer. Clin 590Exp Allergy 2003; 33:470-4.
591E16. Akcakaya N, Hassanzadeh A, Camcioglu Y, Cokugras H. Local and systemic 592reactions during immunotherapy with adsorbed extracts of house dust mite in children. 593Ann Allergy Asthma Immunol 2000; 85:317-21.
594E17. Bagg AS, Chacko T, Lockey RF. Systemic Reactions to Prick and Intradermal 595Skin Tests. J Allergy Clin Immunol 2009; 123.
596E18. Valyasevi MA, Maddox DE, Li JT. Systemic reactions to allergy skin tests. Ann 597Allergy Asthma Immunol 1999; 83:132-6.
598
599
600
89 45 90