0129ccccc0366140524d77f7510e2364.doc Page 1 of 21
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT WORKSHEET for PROPOSED Evidence-Based GUIDELINE RECOMMENDATIONS NOTE: Save worksheet using the following filename format: Taskforce.Topic.Author.Date.Doc where Taskforce is a=ACLS, b=BLS, p=Pediatric, n=neonatal and i=Interdisciplinary. Use 2 or 3 letter abbreviation for author’s name and 30Jul03 as sample date format. Worksheet Author: Taskforce/Subcommittee: __BLS __ACLS _X_PEDS __ID _PROAD Ricardo Samson __Other: Author’s Home Resuscitation Council: _X_AHA __ANZCOR __CLAR __ERC __HSFC Date Submitted to Subcommittee: August 16, 2004; revised November 23, 2004 __HSFC __RCSA ___IAHF ___Other:
STEP 1: STATE THE PROPOSAL. State if this is a proposed new guideline; revision to current guideline; or deletion of current guideline. Existing guideline, practice or training activity, or new guideline: Update of existing guideline
From Guidelines 2000, pp I-316-319
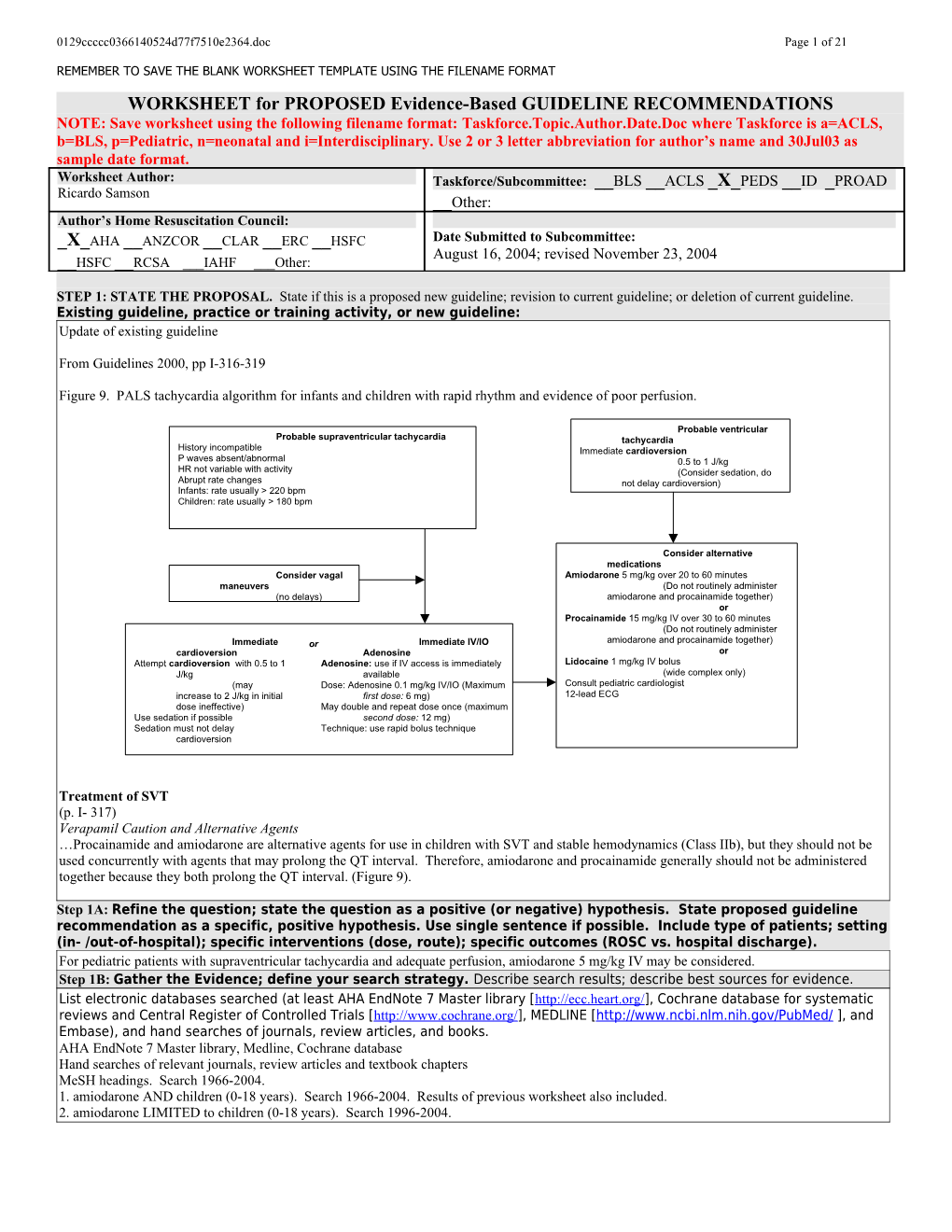
Figure 9. PALS tachycardia algorithm for infants and children with rapid rhythm and evidence of poor perfusion.
Probable ventricular Probable supraventricular tachycardia tachycardia History incompatible Immediate cardioversion P waves absent/abnormal 0.5 to 1 J/kg HR not variable with activity (Consider sedation, do Abrupt rate changes not delay cardioversion) Infants: rate usually > 220 bpm Children: rate usually > 180 bpm
Consider alternative medications Consider vagal Amiodarone 5 mg/kg over 20 to 60 minutes maneuvers (Do not routinely administer (no delays) amiodarone and procainamide together) or Procainamide 15 mg/kg IV over 30 to 60 minutes (Do not routinely administer Immediate or Immediate IV/IO amiodarone and procainamide together) cardioversion Adenosine or Attempt cardioversion with 0.5 to 1 Adenosine: use if IV access is immediately Lidocaine 1 mg/kg IV bolus J/kg available (wide complex only) (may Dose: Adenosine 0.1 mg/kg IV/IO (Maximum Consult pediatric cardiologist increase to 2 J/kg in initial first dose: 6 mg) 12-lead ECG dose ineffective) May double and repeat dose once (maximum Use sedation if possible second dose: 12 mg) Sedation must not delay Technique: use rapid bolus technique cardioversion
Treatment of SVT (p. I- 317) Verapamil Caution and Alternative Agents …Procainamide and amiodarone are alternative agents for use in children with SVT and stable hemodynamics (Class IIb), but they should not be used concurrently with agents that may prolong the QT interval. Therefore, amiodarone and procainamide generally should not be administered together because they both prolong the QT interval. (Figure 9).
Step 1A: Refine the question; state the question as a positive (or negative) hypothesis. State proposed guideline recommendation as a specific, positive hypothesis. Use single sentence if possible. Include type of patients; setting (in- /out-of-hospital); specific interventions (dose, route); specific outcomes (ROSC vs. hospital discharge). For pediatric patients with supraventricular tachycardia and adequate perfusion, amiodarone 5 mg/kg IV may be considered. Step 1B: Gather the Evidence; define your search strategy. Describe search results; describe best sources for evidence. List electronic databases searched (at least AHA EndNote 7 Master library [http://ecc.heart.org/], Cochrane database for systematic reviews and Central Register of Controlled Trials [http://www.cochrane.org/], MEDLINE [http://www.ncbi.nlm.nih.gov/PubMed/ ], and Embase), and hand searches of journals, review articles, and books. AHA EndNote 7 Master library, Medline, Cochrane database Hand searches of relevant journals, review articles and textbook chapters MeSH headings. Search 1966-2004. 1. amiodarone AND children (0-18 years). Search 1966-2004. Results of previous worksheet also included. 2. amiodarone LIMITED to children (0-18 years). Search 1996-2004. 0129ccccc0366140524d77f7510e2364.doc Page 2 of 21
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
• State major criteria you used to limit your search; state inclusion or exclusion criteria (e.g., only human studies with control group? no animal studies? N subjects > minimal number? type of methodology? peer-reviewed manuscripts only? no abstract-only studies?) Peer-reviewed manuscripts only, no abstract-only studies Inclusion criteria: intravenous amiodarone, arrhythmias Exclusion criteria: oral amiodarone, non-relevant case reports, treatment of ventricular arrhythmias, non-arrhythmia references • Number of articles/sources meeting criteria for further review: Create a citation marker for each study (use the author initials and date or Arabic numeral, e.g., “Cummins-1”). . If possible, please supply file of best references; EndNote 6+ required as reference manager using the ECC reference library. Amiodarone: number of articles found: 94; number meeting inclusion and exclusion criteria: 21
STEP 2: ASSESS THE QUALITY OF EACH STUDY Step 2A: Determine the Level of Evidence. For each article/source from step 1, assign a level of evidence—based on study design and methodology. Level of Definitions Evidence (See manuscript for full details) Level 1 Randomized clinical trials or meta-analyses of multiple clinical trials with substantial treatment effects Level 2 Randomized clinical trials with smaller or less significant treatment effects Level 3 Prospective, controlled, non-randomized, cohort studies Level 4 Historic, non-randomized, cohort or case-control studies Level 5 Case series: patients compiled in serial fashion, lacking a control group Level 6 Animal studies or mechanical model studies Level 7 Extrapolations from existing data collected for other purposes, theoretical analyses Level 8 Rational conjecture (common sense); common practices accepted before evidence-based guidelines
Step 2B: Critically assess each article/source in terms of research design and methods. Was the study well executed? Suggested criteria appear in the table below. Assess design and methods and provide an overall rating. Ratings apply within each Level; a Level 1 study can be excellent or poor as a clinical trial, just as a Level 6 study could be excellent or poor as an animal study. Where applicable, please use a superscripted code (shown below) to categorize the primary endpoint of each study. For more detailed explanations please see attached assessment form.
Component of Study and Rating Excellent Good Fair Poor Unsatisfactory Design & Highly appropriate Highly appropriate Adequate, Small or clearly Anecdotal, no sample or model, sample or model, design, but biased population controls, off randomized, proper randomized, proper possibly biased or model target end-points controls controls Methods AND OR OR OR OR Outstanding Outstanding accuracy, Adequate under Weakly defensible Not defensible in accuracy, precision, and data the in its class, limited its class, precision, and data collection in its class circumstances data or measures insufficient data collection in its or measures class A = Return of spontaneous circulation C = Survival to hospital discharge E = Other endpoint B = Survival of event D = Intact neurological survival Step 2C: Determine the direction of the results and the statistics: supportive? neutral? opposed?
DIRECTION of study by results & statistics: SUPPORT the proposal NEUTRAL OPPOSE the proposal Outcome of proposed guideline Outcome of proposed guideline Outcome of proposed guideline Results superior, to a clinically important no different from current inferior to current approach degree, to current approaches approach 0129ccccc0366140524d77f7510e2364.doc Page 3 of 21
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
Step 2D: Cross-tabulate assessed studies by a) level, b) quality and c) direction (ie, supporting or neutral/ opposing); combine and summarize. Exclude the Poor and Unsatisfactory studies. Sort the Excellent, Good, and Fair quality studies by both Level and Quality of evidence, and Direction of support in the summary grids below. Use citation marker (e.g. author/ date/source). In the Neutral or Opposing grid use bold font for Opposing studies to distinguish them from merely neutral studies. Where applicable, please use a superscripted code (shown below) to categorize the primary endpoint of each study. 0129ccccc0366140524d77f7510e2364.doc Page 4 of 21
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT Supporting Evidence For pediatric patients with supraventricular tachycardia and adequate perfusion, amiodarone 5 mg/kg IV may be considered e c n e
d Excellent i v E
f o
y t i l
a Good u Q
Burri, 2003 E Valsangiacomo, 2002 E Laird, 2003 E Fair Hoffman, 2002 E Juneja, 2002 E Cabrera, 2002 E Dodge, 2002 E Kuga, 1999 E Michael, 1999 E Celiker, 1998 E Drago, 1998 E or F Perry, 1996 E Soult, 1995 E Figa, 1994 E or F Perry, 1993 E or F 1 2 3 4 5 6 7 8 Level of Evidence A = Return of spontaneous circulation D = Intact neurological survival G = non-inducibility on EP testing B = Survival of event E = Restoration of sinus rhythm H = other endpoint C = Survival to hospital discharge F = Decrease in tachycardia rate * adult studies Neutral or Opposing Evidence For pediatric patients with supraventricular tachycardia and adequate perfusion, amiodarone 5 mg/kg IV may be considered e c n e
d Excellent i v E
f o
y t i l
a Good u Q
Fair Yap, 2000 H Daniels, 1998 H McKee, 2003 H Gandy, 1998 H
1 2 3 4 5 6 7 8 Level of Evidence A = Return of spontaneous circulation D = Intact neurological survival G = Non-inducibility on EP testing B = Survival of event E = Restoration of sinus rhythm H = Other endpoint C = Survival to hospital discharge F = Decrease in tachycardia rate * adult studies 0129ccccc0366140524d77f7510e2364.doc Page 5 of 21
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
STEP 3. DETERMINE THE CLASS OF RECOMMENDATION. Select from these summary definitions. CLASS CLINICAL DEFINITION REQUIRED LEVEL OF EVIDENCE Class I • Always acceptable, safe • One or more Level 1 studies are present (with rare Definitely recommended. Definitive, • Definitely useful exceptions) excellent evidence provides support. • Proven in both efficacy & effectiveness • Study results consistently positive and compelling • Must be used in the intended manner for proper clinical indications. Class II: • Safe, acceptable • Most evidence is positive Acceptable and useful • Clinically useful • Level 1 studies are absent, or inconsistent, or lack • Not yet confirmed definitively power • No evidence of harm • Class IIa : Acceptable and useful • Safe, acceptable • Generally higher levels of evidence Good evidence provides support • Clinically useful • Results are consistently positive • Considered treatments of choice • Class IIb: Acceptable and useful • Safe, acceptable • Generally lower or intermediate levels of evidence Fair evidence provides support • Clinically useful • Generally, but not consistently, positive results • Considered optional or alternative treatments Class III: • Unacceptable • No positive high level data Not acceptable, not useful, may be • Not useful clinically • Some studies suggest or confirm harm. harmful • May be harmful. • Research just getting started. • Minimal evidence is available Indeterminate • Continuing area of research • Higher studies in progress • No recommendations until • Results inconsistent, contradictory further research • Results not compelling
STEP 3: DETERMINE THE CLASS OF RECOMMENDATION. State a Class of Recommendation for the Guideline Proposal. State either a) the intervention, and then the conditions under which the intervention is either Class I, Class IIA, IIB, etc.; or b) the condition, and then whether the intervention is Class I, Class IIA, IIB, etc. Indicate if this is a __Condition or _X_Intervention Final Class of recommendation: __Class I-Definitely Recommended __Class IIa-Acceptable & Useful; good evidence _X_Class IIb-Acceptable & Useful; fair evidence __Class III – Not Useful; may be harmful __Indeterminate-minimal evidence or inconsistent
REVIEWER’S PERSPECTIVE AND POTENTIAL CONFLICTS OF INTEREST: Briefly summarize your professional background, clinical specialty, research training, AHA experience, or other relevant personal background that define your perspective on the guideline proposal. List any potential conflicts of interest involving consulting, compensation, or equity positions related to drugs, devices, or entities impacted by the guideline proposal. Disclose any research funding from involved companies or interest groups. State any relevant philosophical, religious, or cultural beliefs or longstanding disagreements with an individual. Background: Pediatrics/Pediatric Cardiology/Pediatric Electrophysiology Experience: Member – Pediatric Resuscitation Sub-Committee, ECC, AHA, 2002-present Panel Member- Anti-arrhythmic therapy. ECC Guidelines 2000 Conflicts of interest – none No philosophical, religious or cultural disagreements.
REVIEWER’S FINAL COMMENTS AND ASSESSMENT OF BENEFIT / RISK: Summarize your final evidence integration and the rationale for the class of recommendation. Describe any mismatches between the evidence and your final Class of Recommendation. “Mismatches” refer to selection of a class of recommendation that is heavily influenced by other factors than just the evidence. For example, the evidence is strong, but implementation is difficult or expensive; evidence weak, but future definitive evidence is unlikely to be obtained. Comment on contribution of animal or mechanical model studies to your final recommendation. Are results within animal studies homogeneous? Are animal results consistent with results from human studies? What is the frequency of adverse events? What is the possibility of harm? Describe any value or utility judgments you may have made, separate from the evidence. For example, you believe evidence-supported interventions should be limited to in-hospital use because you think proper use is too difficult for pre-hospital providers. Please include relevant key figures or tables to support your assessment. 0129ccccc0366140524d77f7510e2364.doc Page 6 of 21
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
1. There have been 14 published reports of the use of intravenous amiodarone in children < 18 years of age. The results of these articles are summarized in the table below. Because supraventricular tachycardia encompasses a wide variety of electrophysiologic mechanisms, results of individual arrhythmia substrates must be examined individually:
2. Junctional ectopic tachycardia (JET) is the single most common substrate for which amiodarone was used, comprising nearly half of the total number of patients in the published experience. Nearly all of these patients’ arrhythmias occurred in the immediate post-operative setting following congenital heart disease repair or palliation. Historically, post-operative JET was a malignant tachyarrhythmia, often refractory to conventional antiarrhythmic therapy, and often leading to cardiovascular compromise and ultimately significant post-operative morbidity and mortality. Intravenous amiodarone was shown to be effective in the treatment of JET, with an overall success rate of 87%. Success in these cases is defined as restoration to sinus rhythm in most reports, or partial success defined as a decrease in tachycardia rate so as to achieve hemodynamic stability. However, one must keep in mind that the patients experiencing this arrhythmia represent a very narrow, highly selected patient profile and most often occur in a pediatric cardiac ICU setting
3. Atrial ectopic tachycardia (AET) is another SVT mechanism for which intravenous amiodarone has been used. This is another supraventricular arrhythmia substrate that is typically difficult to control. Although there is far less experience with amiodarone in this setting than with other forms of SVT, results with amiodarone for AET are generally similar, with restoration of sinus rhythm in approximately 80% of cases.
4. Non-JET SVT comprises the remainder of cases (of which AET is a part). Included in this category are atrial reentrant tachycardias (atrial flutter and atrial fibrillation) as well as the most common forms of SVT (bypass-tract mediated and AV nodal reentrant tachycardia). Once again, success rates for amiodarone in this setting approaches 90%. non SVT JET JET SVT cases succ % AET JET succ % SVT succ % Burri, 2003 17 16 94% 2 - - NA 17 16 94% Cabrera, 15 11 73% - 15 11 73% - - NA Celiker 10 9 90% 4 4 3 75% 6 5 83% Dodge 22 19 86% - 22 19 86% - - NA Figa 18 12 67% 6 4 4 100% 14 8 57% Hoffman 10 10 100% - 10 10 100% - - NA Juneja 7 6 86% - - - NA 7 6 86% Kuga 13 12 92% - - - NA 13 12 92% Laird 11 9 82% - 11 9 82% - - NA Michael 1 1 100% - 1 1 100% - - NA Perry 93 2 1 50% - 1 1 100% 1 0 0% Perry 96 28 24 86% 4 14 13 93% 14 11 79% Soult 23 20 87% - - - NA 23 20 87% Valsangiacomo 7 6 86% 1 3 3 100% 4 3 75% OVERALL 184 159 86% 17 85 74 87% 99 81 88% Abbreviations: SVT, supraventricular tachycardia, AET, atrial ectopic tachycardia; JET, junctional ectopic tachycardia; succ, success.
5. Three references cite complications related to intravenous amiodarone therapy. Yap, et al, describe proarrhythmia of polymorphic ventricular tachycardia, while Daniels and Gandy report complications of hypothyroidism and pulmonary toxicity related to acute administration of IV amiodarone.
6. Overall, amiodarone appears to be effective in the treatment of supraventricular tachycardia, keeping in mind that most of the reported experience in the literature involves junctional ectopic tachycardia. The overall success rate reported for amiodarone in the treatment of a number of supraventricular arrhythmia substrates is 86%. Thus, amiodarone appears to be an acceptable alternative agent for the treatment of SVT.
Preliminary draft/outline/bullet points of Guidelines revision: Include points you think are important for inclusion by the person assigned to write this section. Use extra pages if necessary.
(RECOMMEND NO SIGNIFICANT CHANGE IN THE CURRENT GUIDELINES) Publication: Chapter: Pages: I-317 0129ccccc0366140524d77f7510e2364.doc Page 7 of 21
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
Consensus on Science: Based on one LOE 3 and a number of LOE 5 case series, amiodarone is effective in the treatment of surpraventricular tachycardias with an overall success rate of 86%, but many of the studies were conducted in infants with junctional ectopic tachycardia rather than the more common bypass-tract mediated and AV nodal reentrant tachycardia seen most commonly in the outpatient setting.
Treatment of SVT (p. I- 317) Verapamil Caution and Alternative Agents …Procainamide and amiodarone are alternative agents for use in children with SVT and stable hemodynamics (Class IIb), but they should not be used concurrently with agents that may prolong the QT interval. Therefore, amiodarone and procainamide generally should not be administered together because they both prolong the QT interval. (Figure 9).
Attachments: . Bibliography in electronic form using the Endnote Master Library. It is recommended that the bibliography be provided in annotated format. This will include the article abstract (if available) and any notes you would like to make providing specific comments on the quality, methodology and/or conclusions of the study.
Citation List
Citation Marker Full Citation* Burri, 2003 Burri S, Hug MI, Bauersfeld U. Efficacy and safety of intravenous amiodarone for incessant tachycardias in infants. Eur J Pediatr 2003;162(12):880-4.
Amiodarone is an effective anti-arrhythmic agent for the treatment of supraventricular and ventricular tachycardias. The safety and efficacy of intravenous amiodarone has been described in adults and children but only to a limited extent in infants. The purpose of this study was to evaluate the safety and efficacy of intravenous amiodarone in infants. Between February 1994 and June 2001, 23 infants with a median age of 8 days (range 1-300 days) with life-threatening incessant tachycardias (17 supraventricular, 6 ventricular) were treated with intravenous amiodarone as single anti-arrhythmic agent. At presentation, 22 infants were haemodynamically unstable. Amiodarone was given as an intravenous loading dose of 5 mg/kg over 1 h followed by an intravenous maintenance dose of 5 micro g/kg per min with stepwise increase up to 25 micro g/kg per min until arrhythmia control or side-effects occurred. Amiodarone was effective in 19 infants, partially effective in three and ineffective in one infant. The median time until arrhythmia control was 24 h (range 1-96 h) and the median maintenance dosage 15 micro g/kg per min (range 5-26 micro g/kg per min). Electrophysiological side-effects necessitating dose reduction comprised of sinus bradycardia in two patients. Hypotension in one patient resolved after dose diminution. Neurological side-effects consisted of choreatic movements in one infant, which resolved over time. Amiodarone administration was stopped in one patient with elevated liver enzymes. CONCLUSION: intravenous amiodarone is a safe and effective therapy for life-threatening incessant tachycardias in infants.
Comment: This is the largest series of infants receiving amiodarone in the literature. All of these patients had life-threatening arrhythmias and all but one were hemodynamically unstable at the time of amiodarone administration. Amiodarone was generally well-tolerated and effective in these patients. (LOE 5, quality FAIR, supportive) Cabrera, 2002 Cabrera Duro A. Rodrigo Carbonero D. Galdeano Miranda JM. Martinez Corrales P. Pastor Menchaca E. Macua Biurrun P. Pilar Orive J. [The treatment of postoperative junctional ectopic tachycardia]. [Spanish] Anales Espanoles de Pediatria. 56(6):505-9, 2002 Jun.
OBJECTIVE: To evaluate treatment of junctional ectopic tachycardia after cardiac surgery. MATERIAL AND METHODS: Twenty-seven patients (5.5 % of 488 patients who underwent surgery) were treated for junctional ectopic tachycardia between 1994 and 1998. There were 14 boys and 13 girls with a mean age of 11 11 months. Seven suffered from tetralogy of Fallot, seven 0129ccccc0366140524d77f7510e2364.doc Page 8 of 21
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
from ventricular septal defect, six from atrioventricular septal defect, three from transposition of the great vessels and the remaining four had other complex heart diseases. The mean initial frequency was 186 27 beats/min. Crystalloid cardioplegia was applied in 274 patients (1994-1996) and 20 patients (7.4 %) showed junctional ectopic tachycardia. Hematic cardioplegia was performed in 214 patients (1997-1998) and seven patients (3.2 %) developed junctional ectopic tachycardia. Of the 33 patients who were treated during the surgical procedure with high mean doses of sympathomimetic catecholamine agents, 27 (81 %) developed tachycardia. Tachycardia developed 8.24 7 hours after surgery (range: 1-24 hours) in 25 patients and after 4 and 5 days in the remaining two patients. The mean duration of tachycardia was 4 days. RESULTS: In all patients rectal temperature was reduced to 32-34 C. Nineteen patients (70 %) showed a quick response (1-2 hours), although the technique was effective as an isolated procedure in only one patient. Sympathomimetic catecholamine level was reduced to 2-5 g/kg/min in 20 patients but this was effective in 14 (70 %). In 15 patients intravenous amiodarone was also administered and was effective in 11 patients (73 %). Finally, intravenous propafenone was administered to 5 patients. The most effective treatments were hypothermia with reduction of sympathomimetic catecholamine levels in 7 patients (100 %) or intravenous amiodarone in 4 (80 %). Tachycardia led to low cardiac output in 10 patients and only four recovered normal sinus rhythm. Eight patients died. Of these, hemorrhage in the junction area was confirmed in six patients. CONCLUSIONS: Junctional ectopic tachycardia is favored by high levels of sympathomimetic catecholamines after surgery. On the other hand, myocardial protection with hematic cardioplegia reduces tachycardia. Moderate hypothermia with reduction of sympathomimetic agents or intravenous amiodarone reverses ectopic tachycardia.
Comment: This report deals mostly with JET in the post-operative setting and its treatment in infants. Amiodarone was effective in 11 of 15 patients without major side effects. (LOE 5, quality FAIR, supportive) Celiker, 1998 Celiker A. Ceviz N. Ozme S. Effectiveness and safety of intravenous amiodarone in drug- resistant tachyarrhythmias of children. Acta Paediatrica Japonica. 40(6):567-72, 1998 Dec.
BACKGROUND: Experience with pediatric use of intravenous amiodarone is limited. In this study, our experiences with intravenous amiodarone in children with acute life-threatening or chronic tachyarrhythmias are reviewed. METHODS AND RESULTS: Twelve patients, with a mean age of 3.4 +/- 3.1 years, range 9 months-10 years (two with incessant ventricular tachycardia, one with ectopic atrial tachycardia, two with atrioventricular re-entrant tachycardia (three episodes), four with postoperative or congenital junctional ectopic tachycardia, two with bradycardia-tachycardia syndrome, one with atrial tachycardia) were treated with intravenous amiodarone during 13 tachycardia episodes. Left ventricular systolic functions were depressed in six patients. In 11 patients, a median of two drugs (range one-four), including adenosine infusion and in five cases direct current cardioversion were tried without success prior to intravenous amiodarone. The loading dose of amiodarone was 5 mg/kg in all episodes, infused over 1 h. Maintenance infusion was required in 12 episodes. In 10 episodes (77%), amiodarone was considered effective, in one (7.6%) partially effective (junctional ectopic tachycardia) and in two (15.4%) ineffective (sick sinus syndrome, atrial tachycardia). Therapeutic effect was obtained in a median period of 30 h (range 1-103 h). The mean effective maintenance dose was 10 +/- 4.7 micrograms/kg per min (range 5-15 micrograms/kg per min). In one patient, mild hypotension, and in three patients cellulitis occurred, but none of them necessitated termination of treatment. CONCLUSIONS: Intravenous amiodarone is found to be an effective and safe antiarrhythmic agent for children with acute life-threatening and chronic tachyarrhythmias and depressed left ventricular systolic functions.
Comments: Describes use of IV amiodarone in patients with refractory arrhythmias. Similar to Perry et al, 1993, although arrhythmic substrates are supraventricular in origin rather than ventricular. Long term F/U shows mortality rate of 30%, felt NOT to be related to amiodarone, but emphasizes the seriousness of the underlying conditions causing refractory arrhythmias in children. (LOE 5, quality FAIR, supportive) Daniels, 1998 Daniels CJ, Schutte DA, Hammond S, Franklin WH. Acute pulmonary toxicity in an infant from intravenous amiodarone.[see comment]. Comment in Am J Cardiol. 1998 May 1;81(9):1171; 0129ccccc0366140524d77f7510e2364.doc Page 9 of 21
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
American Journal of Cardiology. 80(8):1113-6, 1997 Oct 15.
Intravenous amiodarone is an effective treatment for supraventricular and ventricular tachyarrhythmias. We report a case of acute pulmonary toxicity in an infant from intravenous amiodarone and describe the clinical evaluation and laboratory studies leading to the diagnosis.
Comments: This patient became ill and deteriorated clinically prior to starting amiodarone. There is no direct evidence to suggest amiodarone was the cause of the patient’s pulmonary problems, other than the temporal development of worsening of respiratory status after starting IV amio. Amiodarone levels were not obtained, (LOE 5, quality FAIR, opposing) Dodge, 2002 Dodge-Khatami A. Miller OI. Anderson RH. Gil-Jaurena JM. Goldman AP. de Leval MR. Impact of junctional ectopic tachycardia on postoperative morbidity following repair of congenital heart defects. European Journal of Cardio-Thoracic Surgery. 21(2):255-9, 2002 Feb.
OBJECTIVE: To determine the incidence of postoperative junctional ectopic tachycardia (JET), we reviewed 343 consecutive patients undergoing surgery between 1997 and 1999. The impact of this arrhythmia on in-hospital morbidity and our protocol for treatment were assessed. METHODS: We reviewed the postoperative course of patients undergoing surgery for ventricular septal defect (VSD; n=161), tetralogy of Fallot (TOF; n=114), atrioventricular septal defect (AVSD; n=58) and common arterial trunk (n=10). All patients with JET received treatment, in a stepwise manner, beginning with surface cooling, continuous intravenous amiodarone, and/or atrial pacing if the haemodynamics proved unstable. A linear regression model assessed the effect of these treatments upon hours of mechanical ventilation, and stay on the cardiac intensive care unit (CICU). RESULTS: Overall mortality was 2.9% (n=10), with three of these patients having JET and TOF. JET occurred in 37 patients (10.8%), most frequently after TOF repair (21.9%), followed by AVSD (10.3%), VSD (3.7%), and with no occurrence after repair of common arterial trunk. Mean ventilation time increased from 83 to 187 h amongst patients without and with JET patients (P<0.0001). Accordingly, CICU stay increased from 107 to 210 h when JET occurred (P<0.0001). Surface cooling was associated with a prolongation of ventilation and CICU stay, by 74 and 81 h, respectively (P<0.02; P<0.02). Amiodarone prolonged ventilation and CICU stay, respectively, by 274 and 275 h (P<0.05; P<0.06). CONCLUSIONS: Postoperative JET adds considerably to morbidity after congenital cardiac surgery, and is particularly frequent after TOF repair. Aggressive treatment with cooling and/or amiodarone is mandatory, but correlates with increased mechanical ventilation time and CICU stay. Better understanding of the mechanism underlying JET is required to achieve prevention, faster arrhythmic conversion, and reduction of associated in-hospital morbidity.
Comment: Another study examining factors associated with post-operative JET; hence, the focus was not so much on efficacy of amiodarone. Specific dosing protocols were not given and side effects, other than mortality were not listed. (LOE 5, quality FAIR, supportive) Drago, 1998 Drago F, Mazza A, Guccione P, Mafrici A, Di Liso G, Ragonese P. Amiodarone used alone or in combination with propranolol: a very effective therapy for tachyarrhythmias in infants and children. Pediatr Cardiol 1998 Nov-Dec;19(6):445-9
The aim of the study was to evaluate the efficacy of amiodarone used alone or in combination with propranolol in infants and children affected by life-threatening or drug-resistant tachyarrhythmias. The study included 27 children (median age 3 months), affected by life-threatening and/or drug- resistant supraventricular or ventricular tachyarrhythmias. The loading dose of amiodarone was 10- 20 mg/kg/day and the maintenance dose ranged between 3 and 20 mg/kg/day. When amiodarone was ineffective, propranolol was added at a dosage of 2-4 mg/kg/day. The study population was divided into two groups: group A was composed of patients <1 year and group B of patients >1 year. The effectiveness of the therapy was assessed by clinical evaluation, Holter monitoring, exercise testing, and, in patients with reentry tachycardias, electrophysiological testing. Amiodarone used alone was effective or partially effective in 4/14 (28%) patients in group A and in 11/13 (85%) patients in group B (p < 0.006). Among amiodarone-resistant patients, the combined therapy with propranolol was effective in 8/10 patients in group A and 2/2 patients in group B. Therefore, amiodarone used alone or in combination with propranolol was effective in 25/27 (93%) patients. During the follow-up (20.5 +/- 13 months) there were no arrhythmic effects but side 0129ccccc0366140524d77f7510e2364.doc Page 10 of 21
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
effects were noted in 5/27 (18.5%) patients. Amiodarone seems to be an effective drug in the control of the life-threatening and/or drug-resistant supraventricular and ventricular tachyarrhythmias in children. The addition of propranolol can significantly enhance the success rate of this class III drug, especially in the treatment of reentry tachycardias due to accessory pathways.
Comments: It is not specified whether these patients received oral or intravenous amiodarone. The patient population included children with supraventricular (n=20) and ventricular (n=7) tachycardias that were previously refractory to other drugs or was life- threatening. Side effects were not proarrhythmic and consisted of hypothyroidism, skin color changes, corneal deposits and thyroiditis/hepatitis. (LOE 5, quality FAIR, supportive) Figa, 1994 Figa FH, Gow RM, Hamilton RM, Freedom RM. (1994). Clinical efficacy and safety of intravenous Amiodarone in infants and children. Am J Cardiol 74(6): 573-577. The effectiveness and safety of intravenous amiodarone in children are not well stablished. This study reviewed its use in 30 infants and children for life-threatening tachyarrhythmias: 18 patients (19 episodes) with supraventricular tachycardia, and 12 with ventricular tachycardia. Eighteen patients had structural heart defects with arrhythmias that occurred after surgery. The mean loading dose was 5 mg/kg infused over 1 hour, with a starting maintenance dose of 5 micrograms/kg/min. In 18 treatment episodes, amiodarone was used alone or in combination with digoxin. Thirteen patients received amiodarone combined with other antiarrhythmic agents. Intravenous amiodarone was effective or partially effective in 94% of patients, achieving a therapeutic effect in a median time of 1 day (range 1 hour to 5 days). The mean effective maintenance dose was 9.5 micrograms/kg/min (13.7 mg/kg/day), and median treatment duration was 5 days (range 1 to 30). Adverse effects occurred in 18 patients (58%), however none necessitated termination of amiodarone therapy. Potentially significant electrocardiographic abnormalities occurred in 5 patients during combination antiarrhythmic therapy with propafenone. Sinus bradycardia requiring temporary postoperative pacing occurred in 3 patients treated with amiodarone alone. Intravenous amiodarone used alone or in combination therapy is an effective treatment for resistant, life- threatening arrhythmias in infants and children. Combination drug therapy with propafenone must be used cautiously. Potential bradycardia pacing may be necessary during administration of amiodarone after surgery.
Comments: One of the larger pediatric studies involving IV amiodarone (30 pts). Shows high rate of clinical improvement (94% - 71% effective, defined as elimination of arrhythmia, and 23% partially effective, defined as slowing of ventricular rate and improvement in clinical symptoms) . Adverse effects of sinus bradycardia requiring temporary cardiac pacing are especially noteworthy. (LOE 5, quality FAIR, supportive). Gandy, 1998 Gandy J, Wonko N, Kantoch MJ. Risks of intravenous amiodarone in neonates. Canadian Journal of Cardiology. 14(6):855-8, 1998 Jun.
The courses of two neonates treated with intravenous amiodarone for supraventricular tachyarrhythmia, both of whom developed significant adverse effects, are reported. A 13-day-old term newborn developed hypothyroidism after 27 days of mostly intravenous amiodarone for atrioventricular reciprocating tachycardia and severe heart failure. A one-day-old, 36 weeks' gestation newborn developed electromechanical dissociation after receiving an intravenous bolus of amiodarone for rapid atrial flutter. Judicious use of amiodarone is recommended.
Comments: Both infants received large initial boluses of IV amiodarone (15 mg/kg for both). The authors acknowledge this but point out that perhaps there is something about newborns predisposes them to amiodarone side effects, compared with older children. (LOE 5, quality FAIR, opposing) Hoffman, 2002 Hoffman TM. Bush DM. Wernovsky G. Cohen MI. Wieand TS. Gaynor JW. Spray TL. Rhodes LA. Postoperative junctional ectopic tachycardia in children: incidence,risk factors, and treatment. Annals of Thoracic Surgery. 74(5):1607-11, 2002 Nov.
BACKGROUND: Junctional ectopic tachycardia (JET) occurs commonly after pediatric cardiac operation. The cause of JET is thought to be the result of an injury to the conduction system during the procedure and may be perpetuated by hemodynamic disturbances or postoperative electrolyte 0129ccccc0366140524d77f7510e2364.doc Page 11 of 21
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
disturbances, namely hypomagnesemia. The purpose of this study was to determine perioperative risk factors for the development of JET. METHODS: Telemetry for each patient admitted to the cardiac intensive care unit from December 1997 through November 1998 for postoperative cardiac surgical care was examined daily for postoperative JET. A nested case-cohort analysis of 33 patients who experienced JET from 594 consecutively monitored patients who underwent cardiac operation was performed. Univariate and multivariate analyses were conducted to determine factors associated with the occurrence of JET. RESULTS: The age range of patients with JET was 1 day to 10.5 years (median, 1.8 months). Univariate analysis revealed that dopamine or milrinone use postoperatively, longer cardiopulmonary bypass times, and younger age were associated with JET. Multivariate modeling elicited that dopamine use postoperatively (odds ratio, 6.2; p = 0.01) and age less than 6 months (odds ratio, 4.0; p = 0.02) were associated with JET. Only 13 (39%) of the patients with JET received therapeutic interventions. CONCLUSIONS: Junctional ectopic tachycardia occurred in 33 (5.6%) of 594 patients who underwent cardiac operation during the study period. Postoperative dopamine use and younger age were associated with JET. It may be speculated that dopamine should be discontinued in the presence of postoperative JET.
Comments: Still another study examining factors associated with the development and treatment of JET in the post-operative cardiac setting for children. Dosing strategies and side effects of amiodarone were not discussed. (LOE 5, quality FAIR at best, supportive) Juneja, 2002 Juneja R. Shah S. Naik N. Kothari SS. Saxena A. Talwar KK. Management of cardiomyopathy resulting from incessant supraventricular tachycardia in infants and children. Indian Heart Journal. 54(2):176-80, 2002 Mar-Apr.
BACKGROUND: Radiofrequency ablation is considered to be the treatment of choice in patients with ventricular dysfunction related to incessant supraventricular tachycardia. However, reservations regarding its use in infants and children prompted us to try alternative strategies for this group. METHODS AND RESULTS: Eight children (age range: 1 day to 10 years) were diagnosed to have tachycardia-related ventricular dysfunction in the past 6 years. They presented with symptoms of palpitation, dyspnea and/or generalized swelling over the body of 3 months to 2 years'duration. The cardiothoracic ratio at presentation was 64% (52%-70%) and ejection fraction was 22.2% (15%-45%). In 7 patients tachycardia was diagnosed to be ectopic atrial and in 1 it was permanent junctional reciprocating tachycardia. Six of these children were managed with intravenous/oral amiodarone in combination with digoxin (3) and/or propranolol (2). In one child addition of amiodarone to digoxin and propranolol > l led to polymorphic ventricular tachycardia, and amiodarone was withdrawn. Only one child underwent radiofrequency ablation as the first choice because regular follow-up was not possible due to logistic reasons. Sinus rhythm with normalization of ventricular function was achieved in 6 of the 7 children treated medically. One child continued to have frequent episodes of tachycardia and underwent successful radiofrequency ablation of a high right atrial ectopic focus. Two out of the 6 patients on amiodarone could be managed with only digoxin and propranolol after their ventricular function had returned to normal. A third patient relapsed on stopping amiodarone and underwent successful radiofrequency ablation of a left atrial ectopic tachycardia. CONCLUSIONS: Short-term amiodarone in combination with digoxin/propranolol is a safe and effective treatment strategy for infants/children with tachycardiomyopathy. Control of tachycardia is achieved in the majority, leading to recovery of ventricular function. This approach may avoid unnecessary ablations in children or at least postpone it till the procedure would be safer.
Comments: Authors state that patients were treated with “intravenous/oral amiodarone” but no further details as to dosing. One child had proarrhythmia (polymorphous VT) attributable to amiodarone, leading to withdrawal of the drug. (LOE 5, quality FAIR at best, supportive) Kuga, 1999 Kuga K. Yamaguchi I. Sugishita Y. Effect of intravenous amiodarone on electrophysiologic variables and on the modes of termination of atrioventricular reciprocating tachycardia in Wolff- Parkinson-White syndrome. Japanese Circulation Journal. 63(3):189-95, 1999 Mar.
Atrioventricular reciprocating tachycardia (AVRT) associated with the Wolff-Parkinson-White (WPW) syndrome, sometimes terminates spontaneously, generally sustains and eventually becomes drug resistant. Amiodarone is a potent antiarrhythmic drug that is sometimes effective in patients with AVRT which is resistant to conventional antiarrhythmic drugs. However, systematic studies 0129ccccc0366140524d77f7510e2364.doc Page 12 of 21
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
concerning the effects of amiodarone on AVRT have not been reported. This study evaluated the effects of intravenous amiodarone on electrophysiologic variables, and on the sites and the modes of termination of AVRT. Fifteen WPW patients were studied. Nine had overt, and 6 had concealed WPW syndrome. Measurements of electrophysiologic variables and the induction of AVRT were performed by atrial and/or ventricular programmed stimulations. Amiodarone was then administered at a dose of 5 mg/kg over 5 min. The effective refractory periods (ERP) of the atrial, atrioventricular node, ventricular and accessory pathway were increased significantly by amiodarone. The conduction times of all the components were significantly lengthened by amiodarone, except for the His-ventricular (HV) interval in concealed WPW patients. AVRT was induced in all patients, and was terminated by amiodarone in 12 of 13 patients with sustained AVRT. After amiodarone, AVRT was induced in 9 patients. Spontaneous termination was observed 11 times in 3 of the 9 patients in whom AVRT was still induced. In these cases, the modes and sites of termination were the same as during the baseline state. The ERPs and conduction times of all components of AVRT, except the HV interval, were significantly lengthened by amiodarone. Amiodarone is efficacious for terminating AVRT wherever weak links exist. However, sites of spontaneous termination are not significantly affected by amiodarone.
Comments: Predominantly adult patient population, although some patients were as young as 15 years old. Patients with stable SVT induced in EP lab and sustained for > 8 minutes. IV amiodarone was effective in 80%. No adverse effects were reported, although the side effects profile of IV amiodarone was not the subject of this study. (LOE 3. quality of study FAIR, because of the highly specific clinical scenario (EP lab), adult patient population with the inclusion of at least one patient < 18 yo, supportive) Laird, 2003 Laird WP. Snyder CS. Kertesz NJ. Friedman RA. Miller D. Fenrich AL. Use of intravenous amiodarone for postoperative junctional ectopic tachycardia in children. Pediatric Cardiology. 24(2):133-7, 2003 Mar-Apr
To assess the efficacy and safety of intravenous (IV) amiodarone for the treatment of postoperative junctional ectopic tachycardia (JET) in children, we retrospectively reviewed 11 patients treated with IV amiodarone for JET between 1/92 and 2/00. Data included heart rate and hemodynamics pre- and post-amiodarone, drug dosage, duration of therapy, and effect. Success was defined as reversion to sinus rhythm or slowing to a hemodynamically stable rate. The mean heart rate prior to amiodarone was 203 bpm, and the mean systolic blood pressure was 64 mmHg. Mean IV amiodarone loading dose was 8.2 +/- 4.0 mg/kg, followed by an infusion in 7 patients at a dose of 12.9 +/- 3.9 mg/kg/day for a duration of 74.3 +/- 46.9 hours. At 1 hour post-load, mean heart rate was 147 bpm and mean systolic blood pressure was 88 mmHg for the group. Three patients were in sinus rhythm, 4 in intermittent sinus rhythm with accelerated junctional rhythm, and 4 patients solely accelerated junctional rhythm. Control of JET persisted in 9 patients. Of the two patients requiring additional treatment, both had received a 5 mg/kg load and neither was on an infusion. Five patients were paced at some point following amiodarone: four to improve hemodynamics and one for late sinus bradycardia. Side effects included hypotension with loading (1) and late sinus bradycardia (1). One patient was discharged on oral amiodarone. Intravenous amiodarone given in doses of 10 mg/kg in two 5 mg/kg increments, followed by an infusion of 10-15 mg/kg/day for 48- 72 hours, appears to be safe and effective for postoperative JET in patients who fail conventional therapy or who are hemodynamically unstable. Long-term oral therapy is usually not necessary.
Comments: Another study that examines JET in the post-op setting. Excellent efficacy but note that 5 patients required cardiac pacing, including one for sinus bradycardia. (LOE 5, quality FAIR, supportive) McKee, 2003 McKee MR. Amiodarone-an “old” drug with new recommendations. Curr Opin Pediatr 2003;15(2):193-9.
Amiodarone has gained recognition as an antiarrhythmic medication after recent publication of the newly revised American Heart Association guidelines for pediatric resuscitation. Although support for the widespread use of amiodarone in adults has been supported by research, the few pediatric studies demonstrate limited efficacy and highlight the need for additional data. Because of the nature of the need for this type of resuscitation medication, controlled prospective studies will be difficult to obtain if not morally contraindicated. This article reviews the properties of amiodarone 0129ccccc0366140524d77f7510e2364.doc Page 13 of 21
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
and the pertinent pediatric studies to provide healthcare providers supplemental information regarding amiodarone when choosing antiarrhythmics for acute resuscitation. Individual providers need to discern whether the pediatric data available supports widespread acceptance into current treatment regimens.
Comment: This is an editorial rather than a study; however, it suggests that the evidence in pediatric patients at that time did not support the treatment recommendations (LOE7, quality FAIR, opposing). Michael, 1999 Michael JG. Wilson WR Jr. Tobias JD. Amiodarone in the treatment of junctional ectopic tachycardia after cardiac surgery in children: report of two cases and review of the literature. American Journal of Therapeutics. 6(4):223-7, 1999 Jul.
Junctional ectopic tachycardia (JET) occurs most frequently after operative repair of congenital heart defects. The mechanism is thought to involve direct trauma to the atrioventricular node and His bundle resulting in an ectopic focus. Several therapeutic methods have been described in the pediatric literature with varying degrees of success and complication rates. Because heart rates may exceed 200 to 300 beats per minute, there may be inadequate time for ventricular filling. Ventricular filling can be further compromised because of the asynchrony between the atria and the ventricles. These factors can lead to significant compromise of cardiovascular function in the postoperative patient. We describe our experience with amiodarone in two patients who developed postoperative JET after repair of congenital heart defects. Dosing regimens and previous experience with amiodarone in patients with JET are reviewed.
Comments: one month-old patient with post-operative JET received IV amiodarone, responding favorably. The other patient described received oral amiodarone. Review of literature done includes reports of oral amiodarone, as well as IV. (LOE 5, quality FAIR, supportive) Perry, 1993 Perry, JC, Knilans TK, Marlon D, Denfield SW, Fenrich AL, Friedman RA. (1993). Intravenous amiodarone for life-threatening tachyarrhythmias in children and young adults. J Am Coll Cardiol 22(1): 95-98. OBJECTIVES. The purpose of this study was to evaluate the efficacy of intravenous amiodarone in young patients. BACKGROUND. Oral amiodarone therapy has proved useful for problematic arrhythmias in children, but its pharmacokinetics with the oral route preclude its use in several acute settings. METHODS. Intravenous amiodarone was administered in 1-mg/kg body weight aliquots followed by continuous infusion to patients with potentially life-threatening tachyarrhythmias that had not been abolished by standard therapies. RESULTS. Ten patients (mean age 6.8 years) received intravenous amiodarone: for ventricular tachycardia in seven patients and for atrial tachycardia, junctional tachycardia and multiple arrhythmias in one patient each. Surgery for congenital heart defects had been performed previously in six patients. Two patients had a hamartoma causing ventricular tachycardia. Six of 10 patients had complete resolution of arrhythmia with intravenous amiodarone: 4 of 7 with ventricular tachycardia, 1 of 1 with atrial tachycardia and 1 of 1 with postoperative junctional ectopic tachycardia. Intravenous amiodarone was not successful in the two patients with a hamartoma but slowed ventricular tachycardia in one, allowing successful surgical cure. Average drug load at the time of effect was 4.8 mg/kg body weight. Four patients had transient hypotension during loading, corrected with volume or low dose calcium. Intravenous infusion of amiodarone, 10 mg/kg per day, continued an average of 3 days. Four of 10 patients died, all of nonarrhythmic causes not attributable to intravenous amiodarone. CONCLUSIONS. Intravenous amiodarone was well tolerated in this small series of patients. Postoperative ventricular tachycardia was responsive to intravenous amiodarone in 80% (8 of 10) of the patients (95% confidence interval 40% to 99%). Use of this drug in acute, postoperative tachyarrhythmias may be lifesaving in some patients when standard intravenous therapies fail. Comments: Describes use of IV amiodarone in predominantly ventricular arrhythmias, that were refractory to other antiarrhythmic medications. Remarkably high overall mortality rate (40%) speaks toward the overall seriousness of the patients’ underlying conditions and why the primary arrhythmias may not have been responsive to initial forms of therapy. (LOE 5, quality FAIR, supportive) Perry, 1996 Perry JC, Fenrich AL, Hulse JE, Triedman JK, Friedman RA, Lamberti JJ. Pediatric use of intravenous amiodarone: efficacy and safety in critically ill patients from a multicenter protocol. 0129ccccc0366140524d77f7510e2364.doc Page 14 of 21
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
Journal of the American College of Cardiology. 27(5):1246-50, 1996 Apr.
OBJECTIVE. The purpose of this study was to analyze the efficacy and safety of intravenous amiodarone in young patients with critical, drug-resistant arrhythmias. BACKGROUND. Intravenous amiodarone has been investigated in adults since the early 1980s. Experience with the drug in young patients is limited. A larger pediatric study group was necessary to provide responsible guidelines for the drug's use before its market release. METHODS. Eight centers obtained institutional approval of a standardized protocol. Other centers were approved on a compassionate use basis after contacting the primary investigator (J.C.P). RESULTS. Forty patients were enrolled. Standard management in all failed. Many patients had early postoperative tachyarrhythmias (25 of 40), with early successful treatment in 21 (84%) of 25. Twelve patients had ventricular tachyarrhythmias: seven had successful therapy, and six died, none related to the drug. Eleven patients had atrial tachyarrhythmias: 10 of 11 had immediate success, but 3 later died. Fourteen patients had junctional ectopic tachycardia, which was treated with success (sinus rhythm or slowing, allowing pacing) in 13 of 14, with no deaths. Three other patients had supraventricular tachycardias, with success in two and no deaths. The average loading dose was 6.3 mg/kg body weight, and 50% of patients required a continuous infusion. Four patients had mild hypotension during the amiodarone bolus. One postoperative patient experienced bradycardia requiring temporary pacing. There were no proarrhythmic effects. Deaths (9[23%] of 40) were not attributed to amiodarone. CONCLUSIONS. Intravenous amiodarone is safe and effective in most young patients with critical tachyarrhythmia. Intravenous amiodarone can be lifesaving, particularly for postoperative junctional ectopic tachycardia, when standard therapy is ineffective.
Comments: Eleven patients of 40 pts in this series died (NOT nine as mentioned in the abstract.) Two patients died within 3 hours of receiving IV amiodarone. (LOE 3, quality FAIR, supportive) Soult, 1995 Soult JA, Munoz M, Lopez JD, Romero A, Santos J, Tovaruela A. (1995). Efficacy and safety of intravenous amiodarone for short-term treatment of paroxysmal supraventricular tachycardia in children. Pediatr Cardiol 16(1):16-19
The use of intravenous amiodarone was assessed during 23 episodes of paroxysmal supraventricular tachycardia in 15 children aged 9 days to 11 years. Five of the fifteen patients had congenital structural heart disease, and three had Wolf-Parkinson-White syndrome. Tachyarrhythmias were returned to sinus rhythm during 20 of the 23 episodes (87%). No major adverse effects occurred. Recurrence of tachycardia was not observed during short-term follow-up. In conclusion, intravenous amiodarone is an effective, safe antiarrhythmic drug for short-term treatment of supraventricular tachycardia in children.
Comments: Only adverse effects were nausea. In the three cases where IV amiodarone was not effective, subsequent other medical therapy also failed, and either intracardiac pacing (2) or endotracheal intubation (1), resulted in restoration of sinus rhythm. (LOE 5, quality FAIR, supportive) Valsangiacomo, 2002 Valsangiacomo E, et al. Early postoperative arrhythmias after cardiac operation in children. Ann Thorac Surg 2002;74(3):792-6.
BACKGROUND: Arrhythmias are a recognized complication of cardiac operations. However, little is known about the incidence, treatment, and risk factors for early postoperative arrhythmias in children after cardiac operations. METHODS: Diagnosis and treatment of early postoperative arrhythmias were prospectively analyzed in an intensive care unit in 100 consecutive children with a median age of 17 months (range, 1 day to 191 months) who had undergone cardiac operation. Patients were grouped in three different categories of surgical complexity. RESULTS: During a median postoperative time of 1 day (range, 0 to 15 days), 64 critical arrhythmias occurred in 48 patients. Arrhythmias consisted of sinus bradycardia in 30, atrioventricular block II to III in 7, supraventricular tachyarrhythmias in 14, and premature complexes in 13 instances. Treatment of 52 arrhythmias was successful and included pacing in 41, intravenous amiodarone in 8, body cooling in 5, overdrive pacing in 3, and electrolyte correction in 2 cases, with more than one treatment modality in 8 cases. Risk factors for arrhythmias were lower body weight (p < 0.05), longer cardiopulmonary bypass duration (p < 0.05), and a category of higher surgical complexity (p < 0.001). CONCLUSIONS: Early postoperative arrhythmias occur frequently after cardiac operations 0129ccccc0366140524d77f7510e2364.doc Page 15 of 21
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
in children. Sinus bradycardia, atrioventricular block II to III, and supraventricular tachyarrhythmias are the most frequent arrhythmias, which, however, can be treated effectively by means of temporary pacing, cooling, and antiarrhythmic drug therapy. Lower body weight, longer cardiopulmonary bypass duration, and a higher surgical complexity are risk factors for early postoperative arrhythmias.
Comments: Another study focused on arrhythmias in the post-operative cardiac setting. Amiodarone did not receive much attention but it was the drug of choice for JET and dosing regimens were specified. Amiodarone was successful in 6 of the 7 cases in which it was used (not 8 as specified in the abstract. (LOE 5, quality FAIR, supportive) Yap, 2000 Yap SC. Hoomtje T. Sreeram N. Polymorphic ventricular tachycardia after use of intravenous amiodarone for postoperative junctional ectopic tachycardia. International Journal of Cardiology. 76(2-3):245-7, 2000 Nov-Dec.
Comment: 3 patients all developed coarse ventricular fibrillation at two, three, and twelve hours after receiving IV amiodarone for the treatment of JET. The authors do not state the total number of patients receiving amiodarone at their institution (to yield an incidence of proarrhythmia). Their cardiac lesions were not particularly complex (total anomalous pulmonary venous return, ventricular septal defect, Tetralogy of Fallot). (LOE 5, quality FAIR, opposing) *Type the citation marker in the first field and then paste the full citation into the second field. You can copy the full citation from EndNote by selecting the citation, then copying the FORMATTED citation using the short cut, Ctrl-K. After you copy the citation, go back to this document and position the cursor in the field, then paste the citation into the document (use Ctrl-V). For each new citation press Tab to move down to start a new field. 0129ccccc0366140524d77f7510e2364.doc Page 16 of 21
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
EXCLUDED REFERENCES
Reingardiene DI. Azaravichiene AP. Vashkeliene II. [Amiodarone-induced keratopathy]. [Russian]Kardiologiia. 43(5):56-9, 2003.
Smetana P. Pueyo E. Hnatkova K. Batchvarov V. Camm AJ. Malik M. Effect of amiodarone on the descending limb of the T wave. American Journal of Cardiology. 92(6):742-6, 2003 Sep 15.
Bostan OM. Celiker A. Ozme S. Spontaneous resolution of ventricular tachycardia with right bundle branch block morphology: a case report. Turkish Journal of Pediatrics. 45(2):170-3, 2003 Apr-Jun.
Wang JD. Fu YC. Jan SL. Chi CS. Verapamil sensitive idiopathic ventricular tachycardia in an infant. Japanese Heart Journal. 44(5):667-71, 2003 Sep.
De Simone A. De Pasquale M. De Matteis C. Canciello M. Manzo M. Sabino L. Alfano F. Di Mauro M. Campana A. De Fabrizio G. Vitale DF. Turco P. Stabile G. Verapamil plus antiarrhythmic drugs reduce atrial fibrillation recurrences after an electrical cardioversion (VEPARAF Study). European Heart Journal. 24(15):1425-9, 2003 Aug.
McMahon CJ. Laird WP. Fenrich AL. Amiodarone-induced 2 to 1 atrioventricular block in association with prolongation of the QT interval. Cardiology in the Young. 13(3):305-7, 2003 Jun.
Krittayaphong R. Raungrattanaamporn O. Bhuripanyo K. Sriratanasathavorn C. Pooranawattanakul S. Punlee K. Kangkagate C. A randomized clinical trial of the efficacy of radiofrequency catheter ablation and amiodarone in the treatment of symptomatic atrial fibrillation. Journal of the Medical Association of Thailand. 86 Suppl 1:S8-16, 2003 May.
Jouannic JM. Delahaye S. Le Bidois J. Fermont L. Villain E. Dommergues M. Dumez Y. [Results of prenatal management of fetuses with supraventricular tachycardia. A series of 66 cases]. [French] Journal de Gynecologie, Obstetrique et Biologie de la Reproduction. 32(4):338-44, 2003 Jun.
Zhi J. Moore R. Kanitra L. Mulligan TE. Effects of orlistat, a lipase inhibitor, on the pharmacokinetics of three highly lipophilic drugs (amiodarone, fluoxetine, and simvastatin) in healthy volunteers. Journal of Clinical Pharmacology. 43(4):428-35, 2003 Apr.
Hall CM. McCormick KP. Amiodarone and breast feeding. Archives of Disease in Childhood Fetal & Neonatal Edition. 88(3):F255-4, 2003 May.
Walker GM. McLeod K. Brown KL. Franklin O. Goldman AP. Davis C. Extracorporeal life support as a treatment of supraventricular tachycardia in infants. Pediatric Critical Care Medicine. 4(1):52-4, 2003 Jan.
Malfatto G. Facchini M. Zaza A. Characterization of the non-linear rate-dependency of QT interval in humans. Europace. 5(2):163-70, 2003 Apr.
Briassoulis G. Stefanaki K. Peristeri I. Endoh Y. Hatzis T. Is KL-6 a serum indicator of early pulmonary fibrosis in childhood cancer patients? Medical & Pediatric Oncology. 40(1):44-7, 2003 Jan.
Reingardene DI. Azaravichene AP. Korobkova IZ. [Examining the effect of amiodarone on the lung: prospective follow-up data]. [Russian] Vestnik Rentgenologii i Radiologii. (6):29-31, 2002 Nov-Dec.
Ouarda F. M'Saad H. Chaker L. Hakim K. Abid F. [Atrial flutter in neonates and infants: diagnosis and treatment]. [French] Tunisie Medicale. 80(12):764-8, 2002 Dec.
Aurengo A. Leenhardt L. Aurengo H. [Adaptation of thyroid function to excess iodine]. [French] Presse Medicale. 31(35):1658- 63, 2002 Oct 26.
Anonymous. Index of suspicion.[erratum appears in Pediatr Rev. 2003 Sep;24(9):319]. Pediatrics in Review. 23(9):323-8, 2002 Sep.
Junker J. Haverkamp W. Schulze-Bahr E. Eckardt L. Paulus W. Kiefer R. Amiodarone and acetazolamide for the treatment of genetically confirmed severe Andersen syndrome. Neurology. 59(3):466, 2002 Aug 13.
Shah MJ. Rhodes LA. The Institute of Cardiovascular Diseases, Madras Medical Mission, Madras, India. Pediatric Cardiology. 23(2):213-5, 2002 Mar-Apr. 0129ccccc0366140524d77f7510e2364.doc Page 17 of 21
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
Doggrell SA. Amiodarone -- waxed and waned and waxed again. [Review] [73 refs] Expert Opinion on Pharmacotherapy. 2(11):1877-90, 2001 Nov.
Dubin AM. Van Hare GF. Collins KK. Bernstein D. Rosenthal DN. Survey of current practices in use of amiodarone and implantable cardioverter defibrillators in pediatric patients with end-stage heart failure. American Journal of Cardiology. 88(7):809- 10, 2001 Oct 1.
Seto W. Trope A. Carfrae L. Walker S. Visual compatibility of sodium nitroprusside with other injectable medications given to pediatric patients. American Journal of Health-System Pharmacy. 58(15):1422-6, 2001 Aug 1.
Manojkumar R. Sharma A. Grover A. Secondary lymphoma of the heart presenting as recurrent syncope. Indian Heart Journal. 53(2):221-3, 2001 Mar-Apr.
Markou K. Georgopoulos N. Kyriazopoulou V. Vagenakis AG.Iodine-Induced hypothyroidism. [Review] [85 refs] Thyroid. 11(5):501-10, 2001 May.
Vanbesien J. Casteels A. Bougatef A. De Catte L. Foulon W. De Bock S. Smitz J. De Schepper J. Transient fetal hypothyroidism due to direct fetal administration of amiodarone for drug resistant fetal tachycardia. American Journal of Perinatology. 18(2):113-6, 2001.
Rokicki W. Durmala J. Nowakowska E. [Amiodarone for long term treatment of arrhythmia in children]. [Polish] Wiadomosci Lekarskie. 54(1-2):45-50, 2001.
Silvetti MS. Drago F. Bevilacqua M. Ragonese P. Amiodarone-induced torsade de pointes in a child with dilated cardiomyopathy. Italian Heart Journal: Official Journal of the Italian Federation of Cardiology. 2(3):231-6, 2001 Mar.
Effects of amiodarone administration during pregnancy on neonatal thyroid function and subsequent neurodevelopment. [Review] Journal of Endocrinological Investigation. 24(2):116-30, 2001 Feb.
Etheridge SP. Craig JE. Compton SJ. Amiodarone is safe and highly effective therapy for supraventricular tachycardia in infants. [see comment]. Comment in: Am Heart J. 2001 Jan;141(1):3-5; American Heart Journal. 141(1):105-10, 2001 Jan.
Perez Parras MA. Marin Paton M. Negrillo Cantero AM. Caro Cruz E. Gonzalez Rivera F. Moreno Carazo A. [Amiodarone- induced hyperthyroidism]. [Spanish] Anales Espanoles de Pediatria. 53(4):377-9, 2000 Oct.
Bink-Boelkens MT. Pharmacologic management of arrhythmias. [Review] [32 refs] Pediatric Cardiology. 21(6):508-15, 2000 Nov- Dec.
Edwards KE. Wenstone R. Successful resuscitation from recurrent ventricular fibrillation secondary to butane inhalation. British Journal of Anaesthesia. 84(6):803-5, 2000 Jun.
Lupoglazoff JM. Denjoy I. Luton D. Magnier S. Azancot A. Prenatal diagnosis of a familial form of junctional ectopic tachycardia. Prenatal Diagnosis. 19(8):767-70, 1999 Aug.
Thorne SA. Barnes I. Cullinan P. Somerville J. Amiodarone-associated thyroid dysfunction: risk factors in adults with congenital heart disease. Circulation. 100(2):149-54, 1999 Jul 13.
Magee LA. Nulman I. Rovet JF. Koren G. Neurodevelopment after in utero amiodarone exposure. Neurotoxicology & Teratology. 21(3):261-5, 1999 May-Jun.
Castelli G. Ciaccheri M. Cecchi F. Troiani V. Nannini M. Marconi P. Olivotto J. Montereggi A. Dolara A. Nonsustained ventricular tachycardia as a predictor for sudden death in patients with idiopathic dilated cardiomyopathy. The role of amiodarone treatment. Giornale Italiano di Cardiologia. 29(5):514-23, 1999 May.
Elliott PM. Sharma S. Varnava A. Poloniecki J. Rowland E. McKenna WJ. Survival after cardiac arrest or sustained ventricular tachycardia in patients with hypertrophic cardiomyopathy. Journal of the American College of Cardiology. 33(6):1596-601, 1999 May. 0129ccccc0366140524d77f7510e2364.doc Page 18 of 21
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
Kothari SS. Balijepally S. Taneja K. Amiodarone-induced pulmonary toxicity in an adolescent. Cardiology in the Young. 9(2):194-6, 1999 Mar.
Lane J. Van Hare GF. Paroxysmal long RP tachycardia in a three year old: what is the rhythm? Journal of Cardiovascular Electrophysiology. 10(2):261-2, 1999 Feb.
Mehdirad AA. Clem KL. Love CJ. Nelson SD. Schaal SF. Department of Internal Medicine, Ohio State University Medical Center, Columbus, USA. Pacing & Clinical Electrophysiology. 22(1 Pt 2):233-7, 1999 Jan.
Yadav BS. Garg N. Raj D. Hydatid cyst of heart presenting as ventricular tachycardia. Journal of the Association of Physicians of India. 47(3):342-3, 1999 Mar.
Villain E. Bonnet D. Acar P. Aggoun Y. Sidi D. Kachaner J. Service de cardiologie pediatrique. [Recommendations for the treatment of recurrent supraventricular tachycardia in infants]. [French] Archives de Pediatrie. 5(2):133-8, 1998 Feb.
Saidi AS. Friedman RA. el Said H. Nuchtern JG. Fenrich AL. Ventricular tachycardia during repair of gastroschisis.
Grosso S. Berardi R. Cioni M. Morgese G. Transient neonatal hypothyroidism after gestational exposure to amiodarone: a follow- up of two cases. Journal of Endocrinological Investigation. 21(10):699-702, 1998 Nov.
Drouin E. Lande G. Charpentier F. Amiodarone reduces transmural heterogeneity of repolarization in the human heart. Journal of the American College of Cardiology. 32(4):1063-7, 1998 Oct.
Villain E. Butera G. Bonnet D. Acar P. Aggoun Y. Kachaner J. [Neonatal ventricular tachycardia]. [French] Archives des Maladies du Coeur et des Vaisseaux. 91(5):623-9, 1998 May.
Bowers PN. Fields J. Schwartz D. Rosenfeld LE. Nehgme R. Amiodarone induced pulmonary fibrosis in infancy. Pacing & Clinical Electrophysiology. 21(8):1665-7, 1998 Aug.
Sapin R. Schlienger JL. Goichot B. Gasser F. Grucker D. Evaluation of Elecsys free triiodothyronine assay: relevance of age- related reference ranges. Clinical Biochemistry. 31(5):399-404, 1998 Jul.
Aguinaga L. Mont L. Anguera I. Valentino M. Matas M. Brugada J. [Patients with structural heart disease, syncope of unknown etiology and inducible ventricular arrhythmias treated with implantable defibrillators]. [Spanish] Revista Espanola de Cardiologia. 51(7):566-71, 1998 Jul.
Uebing A. Stieh J. Jung O. Kramer HH. Oldigs HD. [Atrial ectopic tachycardia in infancy caused by tumor of the interatrial septum]. [German] Zeitschrift fur Kardiologie. 87(6):478-81, 1998 Jun.
Hutcheson J. Peters CA. Diamond DA. Amiodarone induced epididymitis in children. Journal of Urology. 160(2):515-7, 1998 Aug.
Gandy J. Wonko N. Kantoch MJ. Risks of intravenous amiodarone in neonates. Canadian Journal of Cardiology. 14(6):855-8, 1998 Jun.
Drago F. Mazza A. Garibaldi S. Mafrici A. Santilli A. Ragonese P. Isolated neonatal atrial flutter: clinical features, prognosis and therapy.Giornale Italiano di Cardiologia. 28(4):365-8, 1998 Apr.
Prasad K. Frenneaux MP. Hypertrophic cardiomyopathy: is there a role for amiodarone?[comment]. Comment on: Heart. 1998 Apr;79(4):331-6; Heart (British Cardiac Society). 79(4):317-8, 1998 Apr.
Lengyel M. [Effect of chronic amiodarone therapy on left ventricular function in dilated cardiomyopathy studied by the new Doppler-index]. [Hungarian] Orvosi Hetilap. 139(19):1147-51, 1998 May 10.
Birmingham WP. More on an infant with acute pulmonary toxicity during amiodarone therapy.[comment] American Journal of Cardiology. 81(9):1171, 1998 May 1.
Naitoh N. Washizuka T. Takahashi K. Aizawa Y. Effects of class I and III antiarrhythmic drugs on ventricular tachycardia- interrupting critical paced cycle length with rapid pacing. Japanese Circulation Journal. 62(4):267-73, 1998 Apr. 0129ccccc0366140524d77f7510e2364.doc Page 19 of 21
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT van Daele ME. Berger RM. Smeets J. Hess J. [Sudden death in young persons caused by arrhythmogenic right ventricular dysplasia].[see comment]. [Dutch] Comment in: Ned Tijdschr Geneeskd. 1998 Mar 28;142(13):739-40; Nederlands Tijdschrift voor Geneeskunde. 142(1):32-6, 1998 Jan 3.
Brugada J. Brugada R. Brugada P. Right bundle-branch block and ST-segment elevation in leads V1 through V3: a marker for sudden death in patients without demonstrable structural heart disease. Circulation. 97(5):457-60, 1998 Feb 10.
Cilliers AM. du Plessis JP. Clur SA. Dateling F. Levin SE. Junctional ectopic tachycardia in six paediatric patients. Heart (British Cardiac Society). 78(4):413-5, 1997 Oct. Martin-Du Pan R. Konfino O. Zimmermann M.
MacNeil DJ. The side effect profile of class III antiarrhythmic drugs: focus on d,l-sotalol. [Review] [73 refs] American Journal of Cardiology. 80(8A):90G-98G, 1997 Oct 23. Pharmacologic management of supraventricular tachycardias in children. Part 1: Wolff- Parkinson-White and atrioventricular nodal reentry. [Review] [135 refs] Annals of Pharmacotherapy. 31(10):1227-43, 1997 Oct.
Cecchi F. Montereggi A. Olivotto I. Marconi P. Dolara A. Maron BJ. Risk for atrial fibrillation in patients with hypertrophic cardiomyopathy assessed by signal averaged P wave duration. Heart (British Cardiac Society). 78(1):44-9, 1997 Jul.
Hohnloser SH. Kuck KH. Atrial fibrillation: maintaining stability of sinus rhythm or ventricular rate control? The need for prospective data: the PIAF trial. Pacing & Clinical Electrophysiology. 20(8 Pt 1):1989-92, 1997 Aug.
Villain E. Amiodarone as treatment for atrial tachycardias after surgery. Pacing & Clinical Electrophysiology. 20(8 Pt 2):2130-2, 1997 Aug.
Yalcinkaya S. Kumbasar SD. Semiz E. Tosun Z. Paksoy N. Sustained ventricular tachycardia in cardiac hemochromatosis treated with amiodarone. Journal of Electrocardiology. 30(2):147-9, 1997 Apr.
Calkins H. Bahu M. Shyr Y. Schork A. Bolling S. Kou W. Kirsch M. Morady F. Relationship of amiodarone to postoperative complications of transthoracic implantation of automatic implantable cardioverter defibrillators.
Villain E. Bonnet D. Iserin L. Aggoun Y. Sidi D. Kachaner J. [Treatment and prognosis of tachyarrhythmia after atrial surgical repair of transposition of great vessels]. [French] Archives des Maladies du Coeur et des Vaisseaux. 89(7):851-6, 1996 Jul.
Larbuisson R. Venneman I. Stiels B. The efficacy and safety of intravenous propafenone versus intravenous amiodarone in the conversion of atrial fibrillation or flutter after cardiac surgery. Journal of Cardiothoracic & Vascular Anesthesia. 10(2):229-34, 1996 Feb.
Bouillon T. Schiffmann H. Bartmus D. Gundert-Remy U. Amiodarone in a newborn with ventricular tachycardia and an intracardiac tumor: adjusting the dose according to an individualized dosing regimen. Pediatric Cardiology. 17(2):112-4, 1996 Mar-
Maragnes P. Villain E. Iselin M. David N. Foucault JP. Archives des Maladies du Coeur et des Vaisseaux. 89(5):605-9, 1996 May. Lopes LM. Cha SC. Scanavacca MI. Tuma-Calil VM. Zugaib M. Fetal idiopathic ventricular tachycardia with nonimmune hydrops: benign course. Pediatric Cardiology. 17(3):192-3, 1996 May-Jun.
Piketty ML. d'Herbomez M. Le Guillouzic D. Lebtahi R. Cosson E. Dumont A. Dilouya A. Helal BO. Clinical comparison of three labeled-antibody immunoassays of free triiodothyronine. Clinical Chemistry. 42(6 Pt 1):933-41, 1996 Jun.
Perry JC. Fenrich AL. Hulse JE. Triedman JK. Friedman RA. Lamberti JJ. Pediatric use of intravenous amiodarone: efficacy and safety in critically ill patients from a multicenter protocol. Journal of the American College of Cardiology. 27(5):1246-50, 1996 Apr.
Williams MJ. Low CJ. Restieaux NJ. Tachycardia and cardiomyopathy. New Zealand Medical Journal. 109(1017):78-9, 1996 Mar 8.
Sharada K. Narasimhan C. Rao KN. Soma Raju B. Refractory adenosine-sensitive congenital His bundle tachycardia: response to calcium-channel blockers. Indian Heart Journal. 55(3):259-61, 2003 May-Jun.
Trappe HJ. [Cardiac arrhythmias during pregnancy--what to do?]. [Review] [66 refs] [German] Herz. 28(3):216-26, 2003 May.
Gordon K. Walters W. Jaslow D. Prehospital management of pediatric SVT. Emergency Medical Services. 32(10):48-57, 64, 2003 Oct. 0129ccccc0366140524d77f7510e2364.doc Page 20 of 21
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
Hung YF. Yang W. Chang ML. Supraventricular tachycardia after fenoterol inhalation: report of two cases. Acta Paediatrica Taiwanica. 44(3):165-7, 2003 May-Jun.
Yen HR. Chu SM. Paroxysmal supraventricular tachycardia in neonatal tuberous sclerosis complex and cardiac rhabdomyoma: report of one case. Acta Paediatrica Taiwanica. 44(2):112-5, 2003 Mar-Apr.
Hebbar AK. Hueston WJ. Management of common arrhythmias: Part II. Ventricular arrhythmias and arrhythmias in special populations. [Review] [27 refs] American Family Physician. 65(12):2491-6, 2002 Jun 15.
Matsuoka K. Kasai A. Fujii E. Omichi C. Okubo S. Teramura S. Uchida F. Nakano T. Electrophysiological features of atrial tachycardia arising from the atrioventricular annulus. Pacing & Clinical Electrophysiology. 25(4 Pt 1):440-5, 2002 Apr.
Moura C. Vieira A. Guimaraes H. Areias JC. Perinatal arrhythmias -- diagnosis and treatment. Revista Portuguesa de Cardiologia. 21(1):45-55, 2002 Jan.
Leroy V. Belin V. Farnoux C. Magnier S. Auburtin B. Gondon E. Saizou C. Dauger S. [A case of atrial flutter after umbilical venous catheterization]. [French] Archives de Pediatrie. 9(2):147-50, 2002 Feb.
Toal SC. Vajifdar BU. Gupta AK. Vora AM. Lokhandwala YY. Department of Cardiology, K E M Hospital, Mumbai, India. Adenosine induced PR jump on surface ECG to differentiate atrioventricular nodal re-entrant tachycardia from concealed accessory pathway mediated tachycardia: a bedside test. Heart (British Cardiac Society). 87(1):37-40, 2002 Jan.
Rao BS. Maharana P. Jagannath G. Basu SB. Jha BN. Treatment of recurrent attacks of supraventricular tachycardia during pregnancy causing complications in both mother and fetus. Indian Heart Journal. 53(6):785-7, 2001 Nov-Dec.
Abraham P. International Journal of Clinical Practice. 55(8):569-70, 2001 Oct.
Morrison LJ. Allan R. Vermeulen M. Dong SL. McCallum AL.Conversion rates for prehospital paroxysmal supraventricular tachycardia (PSVT) with the addition of adenosine: a before-and-after trial. Prehospital Emergency Care. 5(4):353-9, 2001 Oct-Dec.
Lee C. Mason LJ. Pediatric cardiac emergencies. [Review] [80 refs] Anesthesiology Clinics of North America. 19(2):287-308, 2001 Jun.
Epstein MR. Saul JP. Weindling SN. Triedman JK. Walsh EP. Atrioventricular reciprocating tachycardia involving twin atrioventricular nodes in patients with complex congenital heart disease. Journal of Cardiovascular Electrophysiology. 12(6):671-9, 2001 Jun.
Trappe HJ. Pfitzner P. [Cardiac arrhythmias in pregnancy]. [Review] [55 refs] [German] Zeitschrift fur Kardiologie. 90 Suppl 4:36- 44, 2001.
Dierkes S. Vester EG. Dobran LJ. Perings C. Strauer BE. Adenosine in the noninvasive diagnosis of dual AV nodal conduction: use as a follow-up parameter after slow pathway ablation in AVNRT. Acta Cardiologica. 56(2):103-8, 2001 Apr.
Benito Bartolome F. Sanchez Fernandez-Bernal C. Comite de Nutricion de la Asociacion Espanola de Pediatria. [Radiofrequency catheter ablation in children with Wolff-Parkinson-White syndrome and sudden cardiac death who had been resuscitated]. [Spanish] Anales Espanoles de Pediatria. 54(4):353-8, 2001 Apr.
Facchini M. Bauersfeld U. Fasnacht M. Candinas R. [Maternal cardiac arrhythmias in pregnancy]. [Review] [51 refs] [German] Schweizerische Medizinische Wochenschrift. Journal Suisse de Medecine. 130(51-52):1962-9, 2000 Dec 23.
Belhassen B. Fish R. Viskin S. Glick A. Glikson M. Eldar M. Adenosine-5'-triphosphate test for the noninvasive diagnosis of concealed accessory pathway. Journal of the American College of Cardiology. 36(3):803-10, 2000 Sep.
Paul T. Bertram H. Bokenkamp R. Hausdorf G. Supraventricular tachycardia in infants, children and adolescents: diagnosis, and pharmacological and interventional therapy. [Review] [42 refs] Paediatric Drugs. 2(3):171-81, 2000 May-Jun.
Paul T. Bertram H. Kriebel T. Windhagen-Mahnert B. Tebbenjohanns J. Hausdorf G. [Supraventricular tachycardia in infants, children and adolescents: diagnosis, drug and interventional therapy]. [Review] [58 refs] [German] 0129ccccc0366140524d77f7510e2364.doc Page 21 of 21
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
Sugiyama H. Yanai J. Komai T. Tan T. Komori S. Nakazawa S. Neonatal catecholaminergic ventricular tachycardia--a case report. Japanese Circulation Journal. 63(9):727-8, 1999 Sep.
Gracious BL. Atrioventricular nodal re-entrant tachycardia associated with stimulant treatment. Journal of Child & Adolescent Psychopharmacology. 9(2):125-8, 1999.
Osborn DA. Lau KC. Uther JB. Coughtrey H. Rochefort MJ. Radiofrequency catheter ablation in a haemodynamically compromised premature neonate with hydrops fetalis. Journal of Paediatrics & Child Health. 35(4):406-8, 1999 Aug.
Tebbenjohanns J. Niehaus M. Korte T. Drexler H. Noninvasive diagnosis in patients with undocumented tachycardias: value of the adenosine test to predict AV nodal reentrant tachycardia. Journal of Cardiovascular Electrophysiology. 10(7):916-23, 1999 Jul.
Markowitz SM. Stein KM. Mittal S. Slotwiner DJ. Lerman BB. Differential effects of adenosine on focal and macroreentrant atrial tachycardia. Journal of Cardiovascular Electrophysiology. 10(4):489-502, 1999 Apr.
Taniguchi Y. Yeh SJ. Wen MS. Wang CC. Lin FC. Wu D. Variation of P-QRS relation during atrioventricular node reentry tachycardia. Journal of the American College of Cardiology. 33(2):376-84, 1999 Feb.