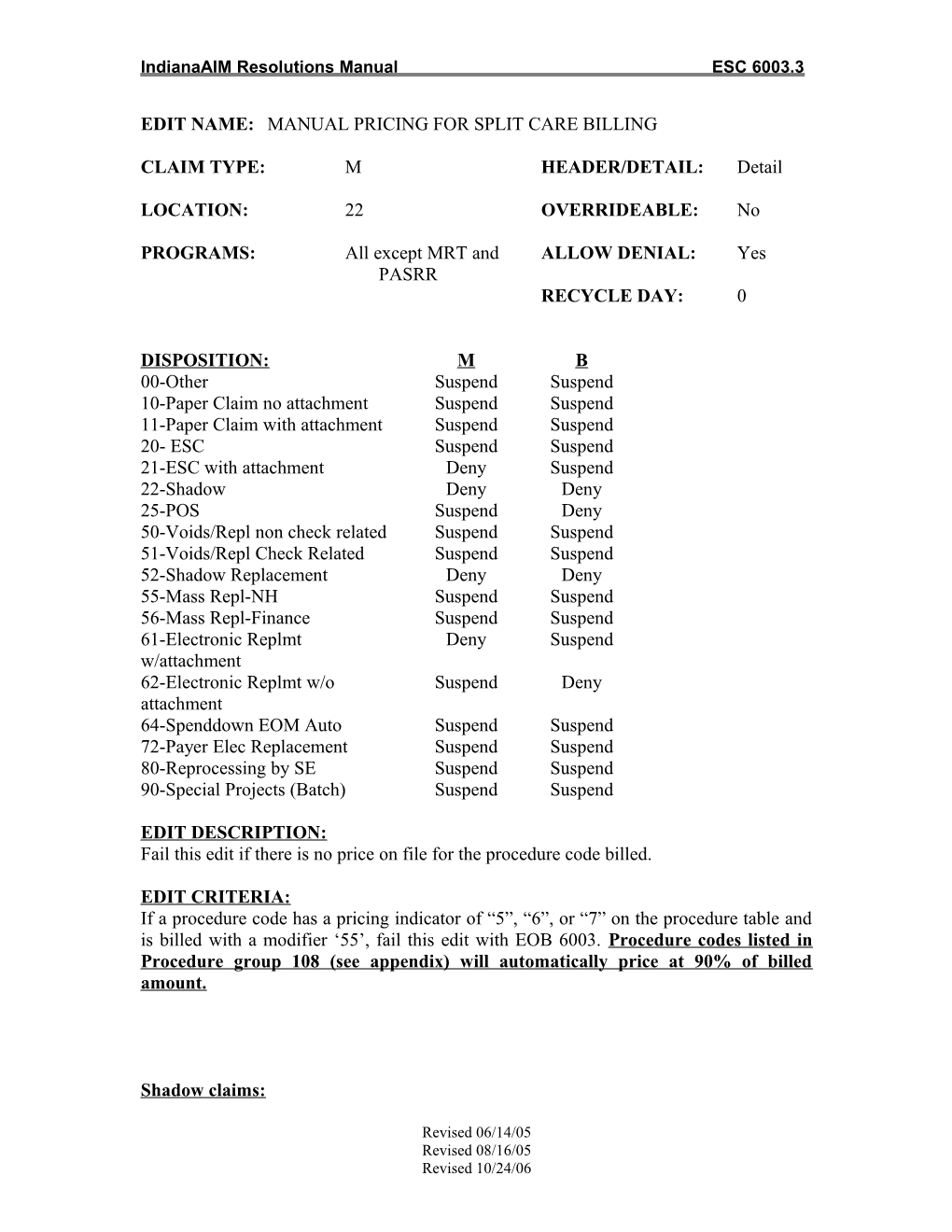
IndianaAIM Resolutions Manual ESC 6003.3
EDIT NAME: MANUAL PRICING FOR SPLIT CARE BILLING
CLAIM TYPE: M HEADER/DETAIL: Detail
LOCATION: 22 OVERRIDEABLE: No
PROGRAMS: All except MRT and ALLOW DENIAL: Yes PASRR RECYCLE DAY: 0
DISPOSITION: M B 00-Other Suspend Suspend 10-Paper Claim no attachment Suspend Suspend 11-Paper Claim with attachment Suspend Suspend 20- ESC Suspend Suspend 21-ESC with attachment Deny Suspend 22-Shadow Deny Deny 25-POS Suspend Deny 50-Voids/Repl non check related Suspend Suspend 51-Voids/Repl Check Related Suspend Suspend 52-Shadow Replacement Deny Deny 55-Mass Repl-NH Suspend Suspend 56-Mass Repl-Finance Suspend Suspend 61-Electronic Replmt Deny Suspend w/attachment 62-Electronic Replmt w/o Suspend Deny attachment 64-Spenddown EOM Auto Suspend Suspend 72-Payer Elec Replacement Suspend Suspend 80-Reprocessing by SE Suspend Suspend 90-Special Projects (Batch) Suspend Suspend
EDIT DESCRIPTION: Fail this edit if there is no price on file for the procedure code billed.
EDIT CRITERIA: If a procedure code has a pricing indicator of “5”, “6”, or “7” on the procedure table and is billed with a modifier ‘55’, fail this edit with EOB 6003. Procedure codes listed in Procedure group 108 (see appendix) will automatically price at 90% of billed amount.
Shadow claims:
Revised 06/14/05 Revised 08/16/05 Revised 10/24/06 IndianaAIM Resolutions Manual ESC 6003.3
Move the amount billed, to the amount allowed, and pay the claim as billed. Do not fail the claim for this edit.
EOB CODES: 6003 – The payment has been calculated according to current Medicaid policies.
9000 – The submitted charge exceeds the allowed charge. Claim paid at Medicaid allowed amount.
9002 – Actual itemized cost invoice must be submitted when billing this procedure code.
9006 – This item should not be billed with this procedure code.
9007 – A procedure code is required when billing this revenue code.
9008 – Line item submitted with unclear itemization. Please resubmit with appropriate and/or additional information.
9905 – Service denied—Medical Necessity documentation must be provided with claim stating the medical necessity.
ARC CODE: A2 – Contractual Adjustment
REMARK CODE: N14- Payment based on a contractual amount or agreement, fee schedule, or maximum allowable amount.
METHOD OF CORRECTION: Check for keying errors and correct any errors found. If no keying errors are found, price the claim per attached guidelines. a. If invoice is required to price claim, and invoice is not present, deny the claim with EOB 9002. b. If invoice is present, or if not necessary for service billed, calculate Medicaid payment using attached guidelines and EOB 6003.
THE MANUAL PRICING PROCEDURES On codes that suspend for manual pricing we pay as follows:
Surgery Codes: Surgery codes ending in XXX99 are routed to PA. These codes are paid at the operation report at 90% of billed. These codes must have the operation report.
Revised 06/14/05 Revised 08/16/05 Revised 10/24/06 IndianaAIM Resolutions Manual ESC 6003.3
NOTE: If a reimbursement amount has not yet been approved by the State for a new HCPC code, then price the code on the aforementioned method until pricing as been approved.
Revised 06/14/05 Revised 08/16/05 Revised 10/24/06